Double-Barrel Left Main Stenting and Simultaneous ‘Ping-Pong’ TAVR Technique With Impella Support
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Blerina Asllanaj, MD; Andrii Maryniak, MD; Filip Oleszak, MD; Marian S. Petrasko, MD, PhD; Adam T. Stys, MD; Tomasz P. Stys, MD
Sanford Health, Sioux Falls, South Dakota
The authors can be contacted via Blerina Asllanaj, MD, at blerina.asllanaj@sanfordhealth.org.
The management of patients with both obstructive coronary artery disease (CAD) and severe aortic stenosis (AS) presents a significant challenge, particularly when the patient is considered a poor surgical candidate. Traditionally, percutaneous coronary intervention (PCI) is performed prior to transcatheter aortic valve replacement (TAVR) to optimize coronary perfusion before addressing the valve pathology. However, emerging evidence suggests that PCI performed after TAVR may also yield favorable outcomes, especially in high-risk patients. This case highlights the complexities of managing severe AS and complex CAD, underscoring the importance of a multidisciplinary approach to decision-making, procedural planning, and post-procedural care.
Clinical Case
A 70-year-old male with a medical history significant for hypertension, hyperlipidemia, chronic diastolic heart failure, and Parkinson’s disease was admitted to the hospital with persistent angina. His angina was refractory to medical therapy, and his condition was further complicated by functional impairment due to Parkinson’s disease.
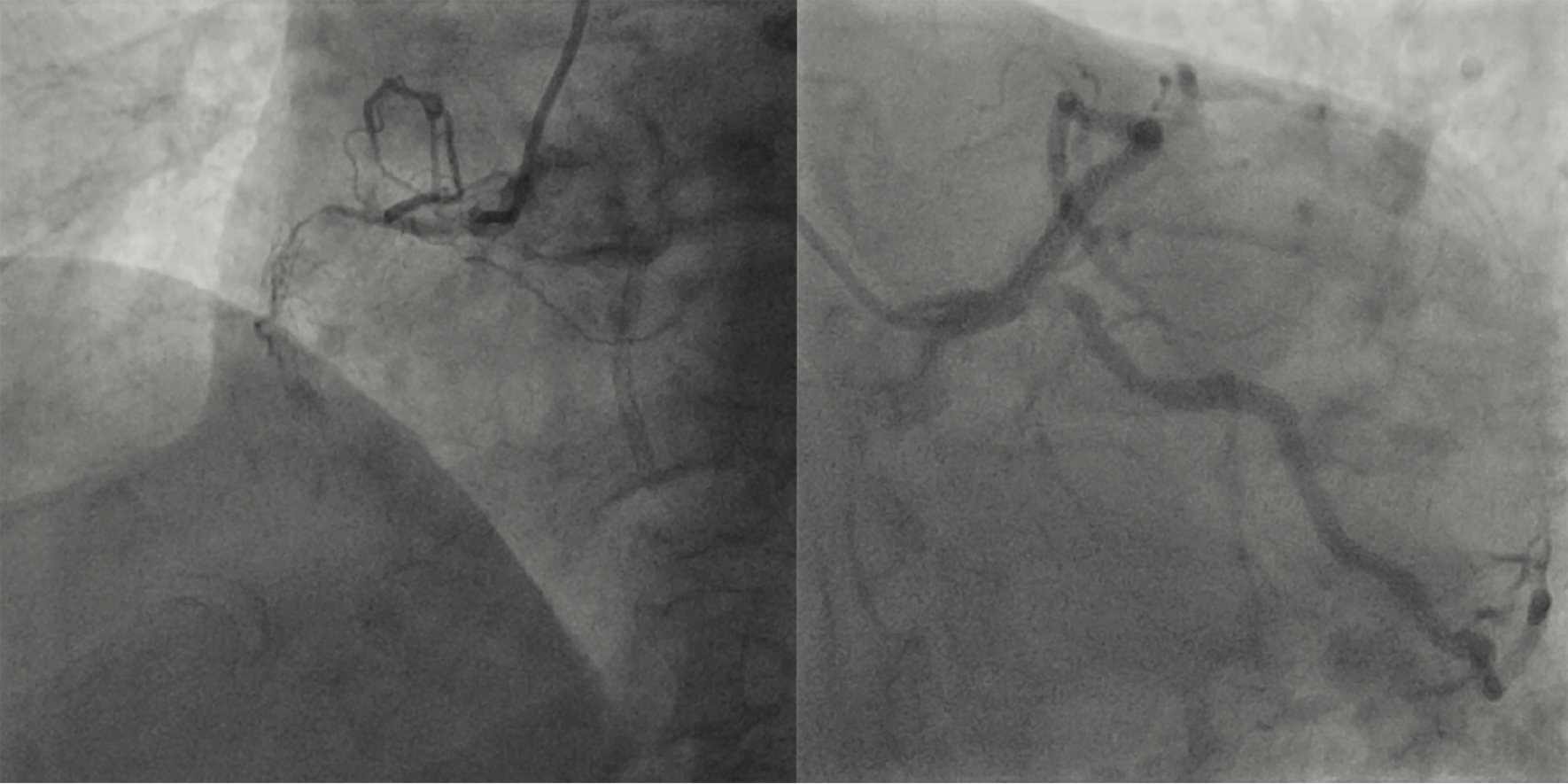
Echocardiography revealed severe aortic stenosis, with a valve area of 0.6 cm², a mean gradient of 34 mmHg, and a peak velocity of 4 m/s, consistent with severe AS. Coronary angiography demonstrated severe coronary artery disease, including left main (LM) stenosis and multivessel CAD (Figure 1). Given the complexity of his coronary pathology, he was deemed unsuitable for traditional coronary artery bypass grafting (CABG) due to the high surgical risk associated with both his coronary disease and comorbidities.
Given his advanced age and high operative risk, a decision was made to pursue a combined intervention approach, consisting of TAVR and coronary revascularization. This strategy aimed to address both his severe aortic stenosis and high-risk coronary lesions in a single procedural session.

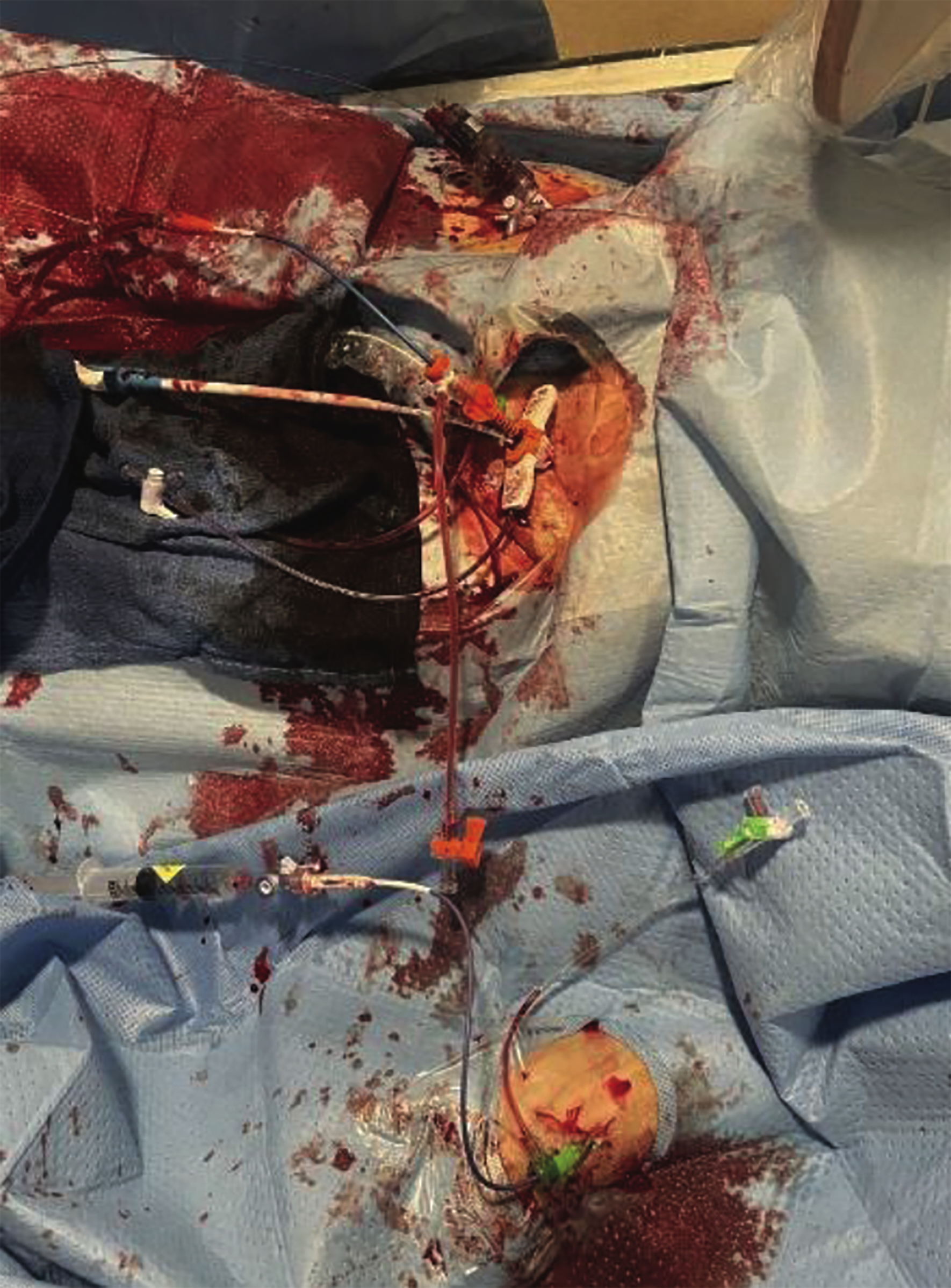
Pre-procedural planning included the use of a heart team approach, including cardiology, cardiothoracic surgery, and anesthesia. The patient was monitored closely, and given his diastolic heart failure, an Impella percutaneous circulatory support device (Abiomed) was utilized to ensure hemodynamic stability during the procedure. The procedure began with transvenous pacing wire insertion via the left femoral vein. Bifemoral and left radial access were established with 6 French sheaths (Figure 2), allowing the team to “alternate” (or “ping-pong”) between coronary intervention and valve delivery without exchanging catheters or losing support. A 7 French sheath was inserted for coronary stenting. The Impella device was placed in the left ventricle to provide circulatory support during the PCI, particularly given the patient’s severe CAD and the anticipated hemodynamic instability from his underlying heart failure (Figure 3).
Coronary angiography revealed critical stenosis of the left main coronary artery and significant disease in the left anterior descending (LAD) and left circumflex (LCx) arteries. A double-barrel technique was successfully employed to stent the left main bifurcation, with optimal angiographic results achieved.
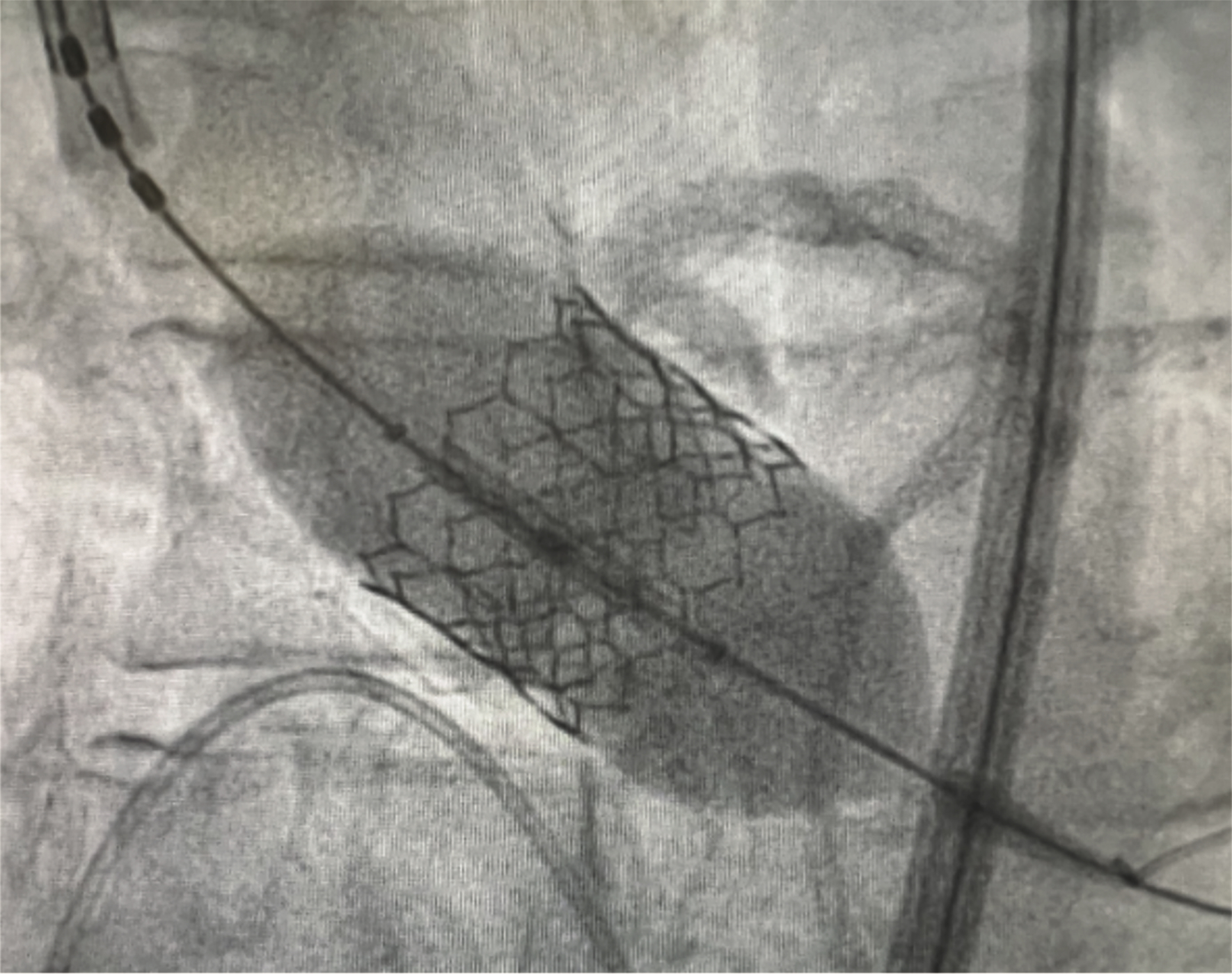
After coronary revascularization, the TAVR was performed using a 26 mm Sapien 3 Ultra valve (Edwards Lifesciences), which was deployed successfully with no complications (Figure 4).
The procedure was completed with femoral artery closure using MANTA devices (Teleflex). Post-procedural recovery was uneventful, with the patient experiencing stable hemodynamics and resolution of his angina symptoms.
Online Exclusive Figure: Technique Summaries
Double-Barrel Stenting
- Access: 7F guide catheter; wire both LAD and LCx.
- Stent Positioning: Advance two DES from LM into LAD and LCx — side-by-side, aligned at ostia.
- Simultaneous Deployment: Inflate both stents at nominal pressure to create a “double barrel” in the LM.
- Proximal optimization technique (POT): Post-dilate LM with NC balloon sized to LM diameter.
- Final Kissing Balloon: Rewire if needed; perform kissing inflation in LAD and LCx.
- Re-POT (if needed): Optimize LM stent apposition.
- Confirm: Use angiography ± IVUS to confirm TIMI 3 flow and stent expansion.
Ping Pong Technique for TAVR + Impella Support
- Dual Access: Obtain two femoral arterial accesses — one for TAVR delivery system, one for Impella.
- Stage 1 – Impella Insertion:
- Place Impella (usually CP or 5.5) via 14F sheath.
- Position across the aortic valve into the LV under fluoroscopy.
- Stage 2 – TAVR Setup:
- Use second femoral access for TAVR delivery system (via 14–16F sheath).
- Valve Crossing:
- Just before valve deployment, pull back Impella into ascending aorta (avoid entrapment).
- TAVR Deployment:
- Deploy valve per standard technique (balloon- or self-expandable).
- Re-Advance Impella:
- Re-position Impella across the new valve post-deployment to resume support.
- Hemodynamic Monitoring:
- Ensure stable support and adequate function through entire sequence.
Key Points
- Maintains continuous support without losing vascular access.
- Enables safe repositioning and avoids stent frame entrapment.
- Ideal for high-risk or cardiogenic shock patients undergoing TAVR.
Discussion
This case exemplifies the evolving role of combined TAVR and PCI in high-risk patients with both severe aortic stenosis and complex coronary artery disease. While conventional practice has typically favored PCI prior to TAVR to optimize coronary perfusion, recent studies suggest that PCI following TAVR may also be a viable strategy. This approach can be particularly beneficial in patients with extensive coronary pathology who are at high surgical risk, as it minimizes the need for multiple separate procedures and allows for more comprehensive management of both cardiac conditions in a single session.1
The decision to combine TAVR and PCI in a single procedure reflects the increasing recognition of the need for a tailored, individualized approach to treating patients with complex coronary and valvular disease. As both TAVR and PCI technologies continue to evolve, future studies will be required to further refine the optimal sequencing and timing of these interventions, as well as to assess long-term clinical outcomes in this high-risk cohort.
Conclusion
This case underscores the complexities involved in managing patients with severe aortic stenosis and complex coronary artery disease, particularly those deemed poor surgical candidates. The combined approach of TAVR and PCI, supported by the Impella device, can offer significant clinical benefits in such high-risk patients, improving outcomes and potentially reducing the need for multiple procedures.
Reference
1. Siontis GCM, Overtchouk P, Cahill TJ, et al. Transcatheter aortic valve implantation vs. surgical aortic valve replacement for treatment of symptomatic severe aortic stenosis: an updated meta-analysis. Eur Heart J. 2019 Oct 7; 40(38): 3143-3153. doi:10.1093/eurheartj/ehz275.
Authors’ Note – An abstract of this case was previously published: Asllanaj B, et al. J Am Coll Cardiol. 2025 Apr 1; 85(12) Suppl A. jacc.org/doi/abs/10.1016/S0735-1097%2825%2903922-1, and was presented at ACC.25 on March 29, 2025.
Find More:
Renal Denervation Topic Center
Cardiovascular Ambulatory Surgery Centers (ASCs) Topic Center
Grand Rounds With Morton Kern, MD
Peripheral Artery Disease Topic Center
Go to Cath Lab Digest's Current Issue
Go to the Journal of Invasive Cardiology Issue










