Dealing With Dense Calcium
Key Summary
- Dense calcium remains a major barrier to successful wire crossing in chronic total occlusions in peripheral arterial disease.
- These cases illustrate feasible adjunctive strategies for balloon or wire uncrossable calcified chronic total occlusions; findings are limited to 3 illustrative cases, without comparative data or generalizable outcomes.
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Vascular Disease Management or HMP Global, their employees, and affiliates.
VASCULAR DISEASE MANAGEMENT. 2025;22(12):E110-E114
Abstract
Calcium remains one of the most significant challenges facing interventional operators. Despite advances in alternative access, procedural tools, and techniques for complex lesion management, heavy calcification continues to be a major barrier to procedural success. Calcific plaque and increasing patient age are among the strongest predictors of failure to cross chronic total occlusions (CTOs) in peripheral arterial disease. In the management of calcified CTOs, common procedural failure modes include an inability to knuckle the wire subintimally, failure to obtain distal target access for retrograde intervention, inadequate device support, and the presence of a large proximal side branch at the proximal cap. This report presents 3 case examples demonstrating novel techniques designed to address these challenges and facilitate successful treatment of heavily calcified CTOs.
Introduction
Calcium, one may argue, is the greatest challenge to interventional operators. In the modern era of alternative access, highly evolved procedural tools, and well-defined approaches to complex lesions, calcium remains our greatest single obstacle to procedural success.1 Calcific plaque and age, which is likely a partial surrogate for calcium, have been shown to be 2 of the strongest predictors of failure to cross chronic total occlusions (CTO) in peripheral arterial disease (PAD).2
When approaching a calcified CTO, common failure modes include an inability to knuckle the wire subintimally, failure to gain distal access for a retrograde option, inadequate support, or a large side-branch at the proximal cap. Here, we provide 3 case examples of novel techniques to overcome these failure modes and deal with dense calcium.
Case 1
An 81-year-old man with a history of controlled diabetes with secondary peripheral neuropathy, severe venous insufficiency, and PAD presented with rest pain and a left great and second toe ulcer for 3 to 4 months. Ankle-brachial index on the left was 0.6, and vascular ultrasound showed a short occlusion of the mid-superficial femoral artery. The patient agreed to proceed to diagnostic angiography.
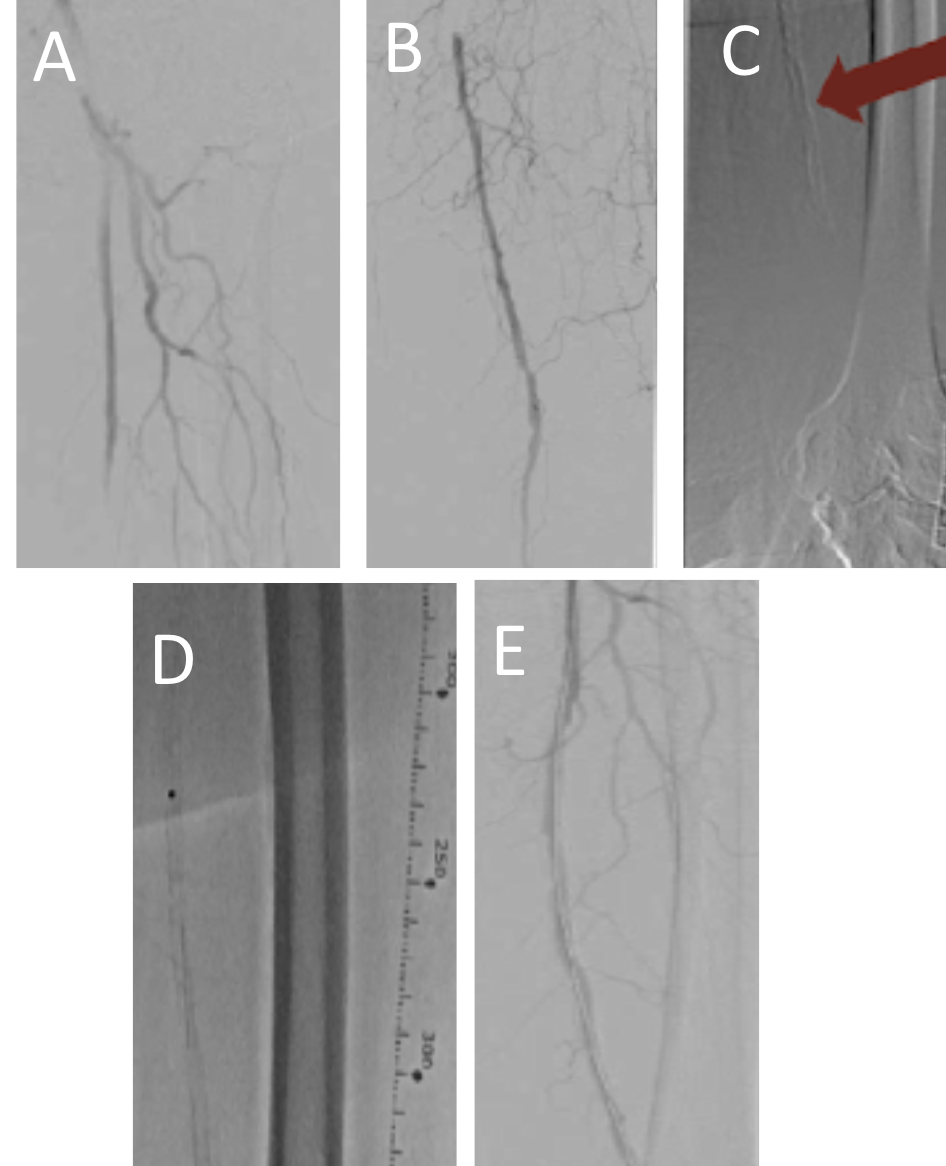
Access was obtained in the contralateral groin; a 7F Destination 45-cm sheath (Terumo) was placed in the left common femoral artery and diagnostic angiography was performed (Figures 1A-C and Videos 1A and 1B). Attempts at crossing with antegrade wire escalation and accompanying supportive microcatheters failed. Next, we prepared a 2.3 Turbo-Power laser (Philips) at a fluency of 60 mJ/mm² and a rate of 80 Hz. We placed the laser adjacent to the calcified CTO and retracted the wire into the laser catheter (of note, it is important to avoid using the laser on the hydrophilic portion of the wire as the wire tip can break). Gentle forward pressure with the laser was applied for a total of 2 minutes during therapy. The laser treatment resulted in easy wire passage through the CTO with a 0.014-inch hydrophilic tipped wire (Figure 1D). Next, 2 passes with the laser for plaque debulking were performed. Despite the laser atherectomy, a standard balloon would still not fully expand, so a 5 x 60-mm Shockwave intravascular lithotripsy balloon (Shockwave Medical) was utilized at 4 atmospheres with good expansion. Finally, a drug-coated balloon was deployed in the treated segment with good results (Figure 1E, Videos 1C and 1D). The patient’s wounds healed after 2 months of follow-up and wound care.
Case 2
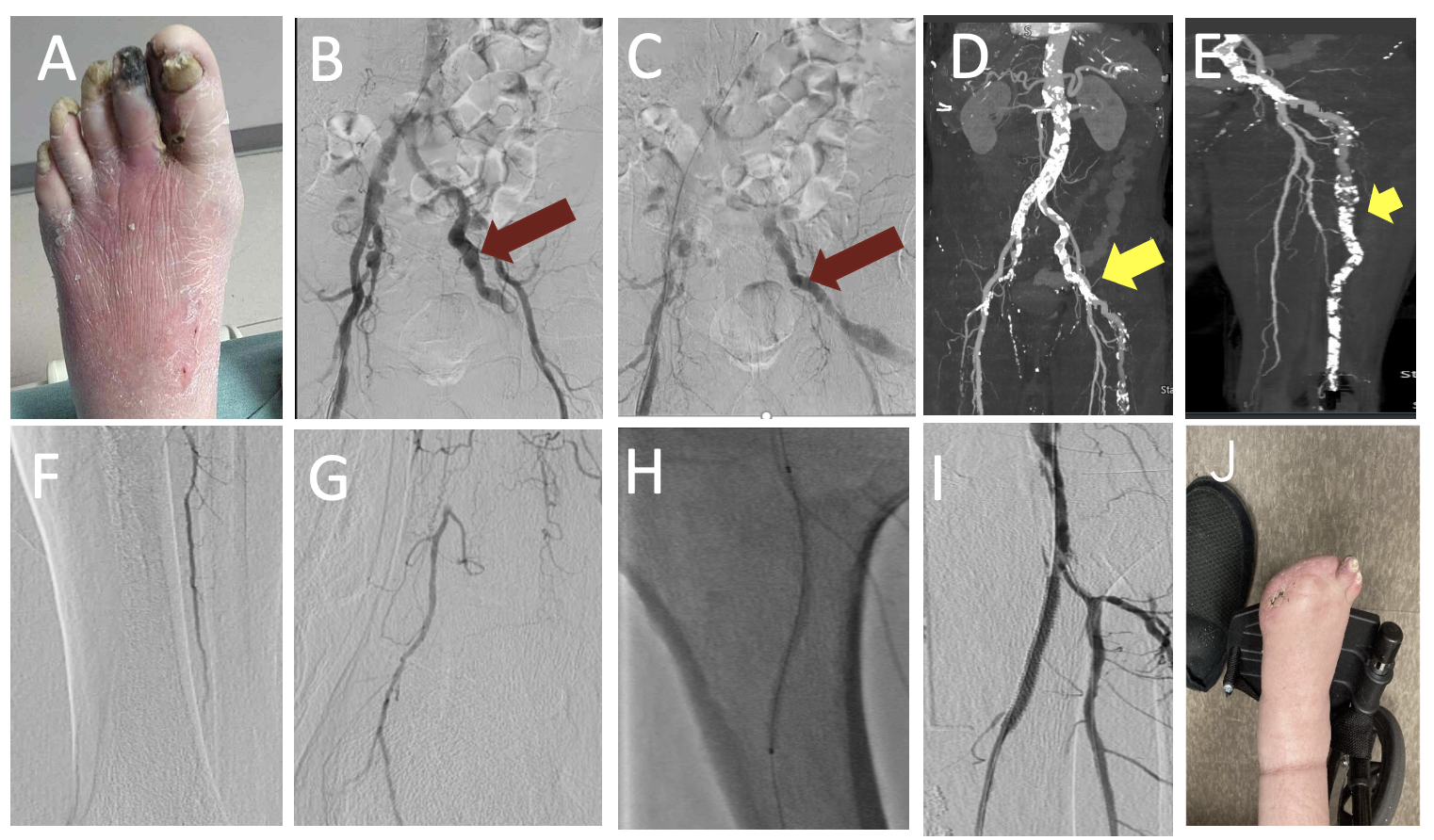
A 77-year-old man with a history of coronary artery disease, hypertension, ongoing heavy smoking, and cirrhosis presented with dry gangrene of the first and second toes (Figure 2A). The patient underwent angiography with planned intervention of the left lower extremity. The inflow images showed abnormal flow in the left internal iliac artery with a diminutive superficial femoral artery (Figures 2B and 2C, Videos 2A and 2B). At this point, the procedure was aborted and a computed tomography (CT) runoff was obtained for additional procedural planning. The CT confirmed the presence of a persistent sciatic artery with severe calcific popliteal and infrapopliteal disease (Figures 2D and 2E).
A persistent sciatic artery occurs in 0.025% to 0.04% of the population and is frequently bilateral. Cowie’s sign is associated with this condition and is described as an absent femoral pulse in combination with a palpable popliteal pulse. The persistent sciatic artery results from a failure of the sciatic artery to involute during embryonic development.
The following day, the patient returned to the angiography suite. We placed a 65-cm 6F Terumo sheath via the internal iliac artery into the persistent sciatic artery that fed the lower leg (Video 2C). The peroneal was wired antegrade with a 0.014-inch Gladius Mongo wire (Asahi) through a 0.018-inch CXI crossing catheter (Cook Medical). A distal injection through the CXI catheter in the peroneal artery confirmed true luminal position and allowed for visualization of a small reconstituted posterior tibial (PT) artery at the ankle (Figures 2F and 2G, Video 2D). Next, we performed laser atherectomy of the popliteal into the peroneal. This was followed by intravascular ultrasound imaging and nominal ballooning of these vessels.
We then treated the PT CTO using retrograde access into the patent distal vessel. The PT was traversed with retrograde wiring using external ultrasound navigation. Kissing balloon dilation was performed into the peroneal and PT arteries. Subsequent stenting of the proximal PT was performed with 3.5 x 38-mm drug-eluting stent. Completion angiography was performed, and the patient’s wound healed after minor amputation (Figures 2H-J, Video 2E).
Case 3
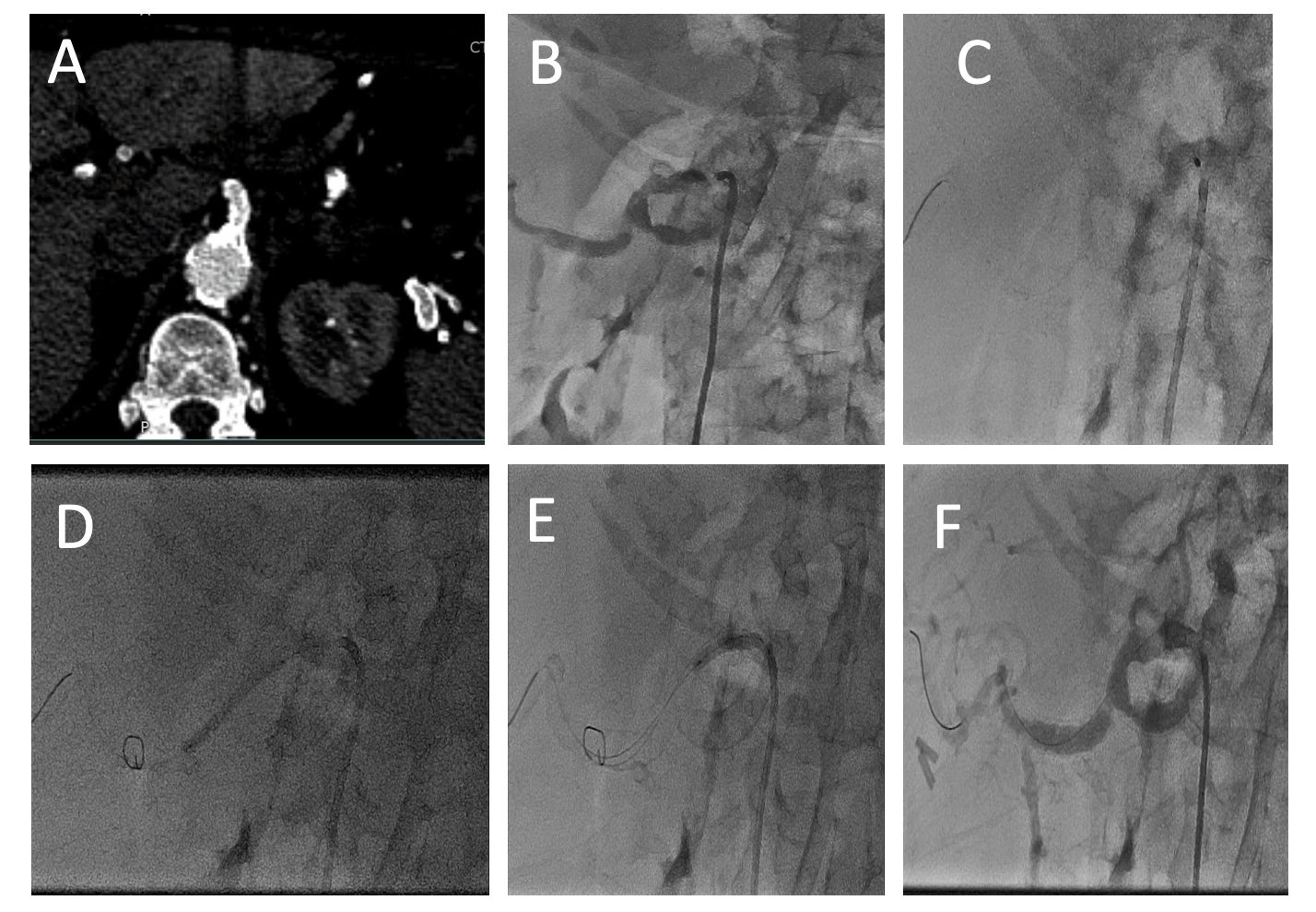
A 69-year-old woman with a history of coronary artery disease and ongoing heavy tobacco abuse presented with several months of severe abdominal pain and weight loss. At the time of presentation, the patient noted an abrupt worsening, which brought her to the hospital. She reported a total weight loss of 40 lb since her symptoms began and was having trouble tolerating oral medications. A CT scan showed a subtotaled, calcified celiac artery and a CTO of the superior mesenteric artery (Figure 3A). Treatment of the celiac lesion had been attempted a week prior by another physician, with an inability to cross the subtotaled celiac artery. She was brought back to the angiography suite for a reattempt.
Using right common femoral access and a 6F sheath, a renal standard guide was placed near the celiac ostium and angiography was performed (Figure 3B, Video 3A). We were able to wire the lesion with a 0.014-inch Gladius Mongo ES; however, the lesion was uncrossable with a coronary balloon or microcatheter. Next, a Javelin forward-facing lithotripsy catheter (Shockwave Medical) was utilized x 100 pulses to soften the plaque (Figure 3C, Video 3B). A buddy wire was advanced beyond the lesion to stabilize the guide catheter. After treatment with the Javelin, a 5.0 coronary balloon easily crossed and successfully predilated the ostial celiac lesion and the second lesion in the hepatic artery branch. This was followed by intravascular ultrasound for sizing. Finally, a 5 x 18-mm Herculink (Abbott Cardiovascular) was deployed at nominal pressure with good expansion in the ostium of the celiac artery (Figures 3D-F, Video 3C). The patient did well and was discharged 2 days later.
Conclusion
These 3 cases exemplify novel techniques to deal with dense calcium in the superficial femoral artery, infrapopliteal vessels, and mesenteric arteries. Case 1 demonstrated leading with a laser to penetrate a recalcitrant proximal cap. Case 2 demonstrated a rare congenital anatomic variation with dense calcium and utilized retrograde pedal access with subsequent kissing balloon inflations to preserve multiple infrapopliteal vessels. Case 3 showed the use of the Shockwave Javelin to treat a balloon uncrossable lesion in the celiac artery. n
Affiliations and Disclosures
Matthew T. Finn, MD, MSc; Pradeep Nair, MD; and Craig Walker, MD, are from Cardiovascular Institute of the South in Gray, Louisiana. Sahil A. Parikh, MD, is from Columbia University Irving Medical Center in New York, New York.
Manuscript accepted December 4, 2025.
Dr. Finn has received consultant fees and honoraria from Nipro, Philips, Haemonetics, and Angiodynamics. He owns stock in Johnson and Johnson via Abiomed, and Fastwave. Dr Finn’s spouse is employed by Johnson and Johnson (Abiomed).
Dr. Parikh receives institutional research funding from Abbott, Acotec, AVS, Boston Scientific, Cagent Vascular, Concept Medical, Fastwave, Medinol, Philips, Veryan Medical, Reflow Medical, R3 Vascular, and Shockwave Medical. He is an advisor to Abbott, Boston Scientific, Cordis, Medtronic, and Philips, and is a consultant to Abiomed, Penumbra, Stryker, and Terumo. He holds stock options in Advanced Nanotherapies and Encompass Vascular.
Address for Correspondence: Matthew T. Finn, MD, MSc, Cardiovascular Institute of the South, 191 Innovation Ct, Suite A, Gray, LA 70359. Email: Matthew.Finn@cardio.com
References
1. Armstrong EJ. Challenges of calcium in critical limb ischemia describing the prevalence of calcium in CLI, its impact on outcomes, and the use of IVUS to improve identification before intervention. Supplement to Endovascular Today. 2021;20(5):9-11.
2. Matthaiou N, Klontzas ME, Kasioumi K, Kakkos GA, Kehagias E, Tsetis D. Development of a scoring system to predict endovascular crossing of femoropopliteal artery chronic total occlusions: the Endo VAscular CROSsing Score for Chronic Total Occlusions (EVACROSS-CTO). Br J Radiol. 2025;98(1168):551-555. doi:10.1093/bjr/tqaf004















