Tips, Tricks, and Pearls For the Minimally Invasive Zadek Osteotomy
Achilles tendinopathy is a debilitating condition affecting both the active (ie athlete) and inactive (ie overweight with no increase in activity) alike.1 Approximately 6 percent of the general population will suffer from this condition in a lifetime.2 The disorder has been subdivided into two categories: insertional and midportion.1 Insertional Achilles tendinopathy, is as the name suggests, inflammation and painful thickening of the tendon at its insertion on the posterior calcaneus.2 It often involves the tendon-bone interface and can be associated with a large posterior superior calcaneal tuberosity (Haglund’s deformity) and/or gastrocnemius/Achilles contracture. The pathophysiology is not fully understood but may be due to several factors including overuse, mechanical irritation, and bursitis, which ultimately leads to collagen fibril injury. Tendinopathy results when there is failed or inadequate healing of the tendon.
What Are the Available Treatment Options?
Conservative management of this condition includes eccentric exercises, extracorporeal shockwave therapy, stretching, heel lifts, platelet-rich plasma injections, and activity modification.3,4 However, failure of nonsurgical management remains high. Generally, if there has been no improvement after 3 to 6 months, then surgical treatment becomes a consideration. It is wise to tailor the surgical procedure to the individual pathology, however, for most patients the approach involves detachment of the tendon followed by debridement, calcaneoplasty with resection of the Haglund’s deformity along with any bone spurs, and reattachment.5 Another approach is the Zadek osteotomy, which is a dorsal closing wedge osteotomy. This approach is thought to reduce the overall length of the calcaneus and elevate the insertion of the Achilles tendon, reducing the lever arm of the Achilles and the mechanical irritation caused by the posterior prominence.6
With the increasing popularity of minimally invasive surgery (MIS), techniques have been developed to perform both procedures percutaneously.7 Surgeons may advocate for one method over the other, and this can lead to confusion for those beginning to adopt MIS methods for this pathology. The traditional method of elevating and reattaching the Achilles, simultaneously resecting the Haglund has demonstrated effectiveness.8 In our observation, determining which patient will benefit from a minimally invasive dorsal closing wedge osteotomy without addressing the Achilles tendon can be challenging for those wanting to add these methods to their armamentarium. More publications are demonstrating benefits of this technique with early return to activity and increased range of motion.6,9 However, it is still early before we can abandon traditional or mini-open Achilles repair in favor of osteotomy alone. Therefore, the goal of this article is to offer clinical tips and pearls to determine which patient will perhaps do better with the MIS closing wedge osteotomy, via a case example-based approach, to aid the young surgeon or surgeons just starting to adopt MIS techniques, when performing the MIS Zadek osteotomy.
Important Considerations in Patient Selection
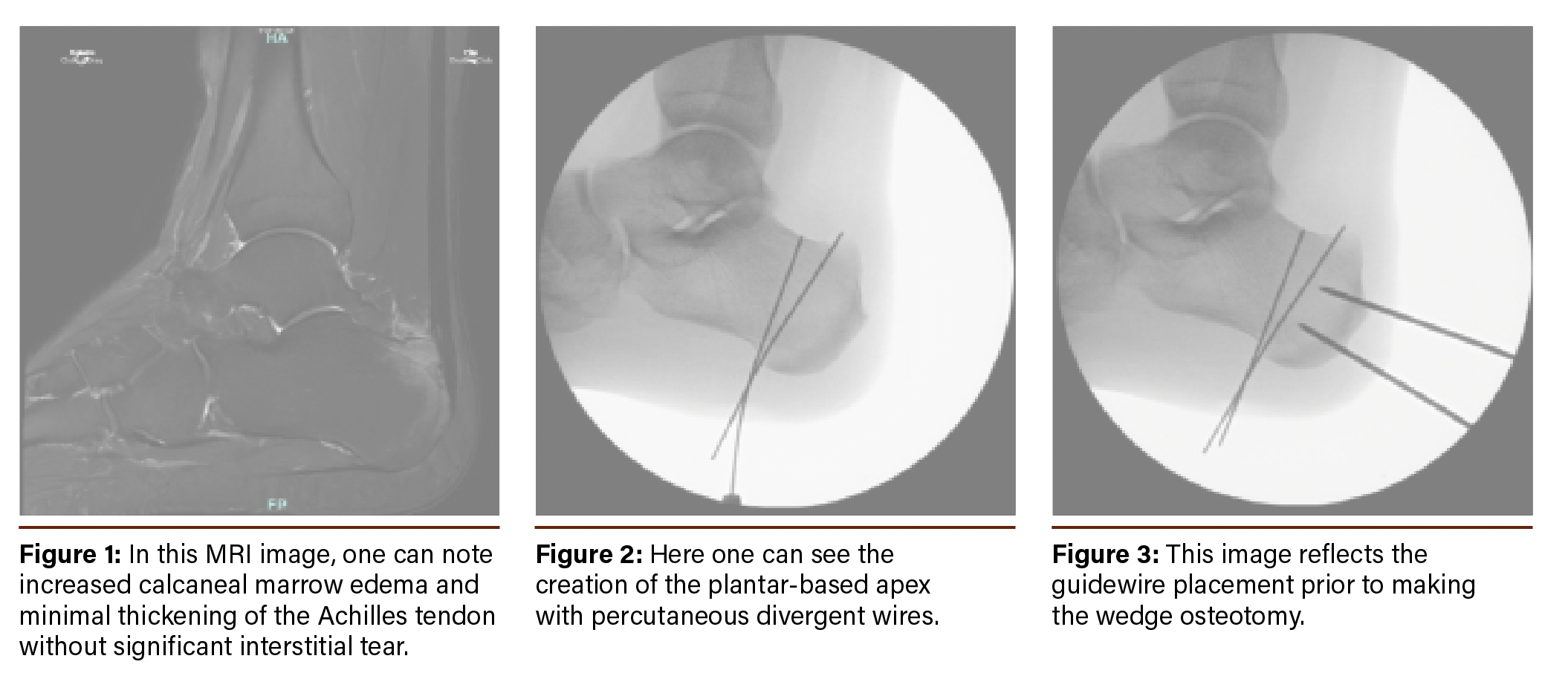
From the authors’ experience, the decision to perform this procedure stems from both the clinical examination as well as magnetic resonance imaging (MRI) findings. In fact, it is our practice to order an ankle MRI for all patients with this condition for whom conservative management has failed. MRI findings focus on Achilles tendon involvement and the calcaneal findings (Figure 1).
Notes on Dr. Siddiqui’s Surgical Technique
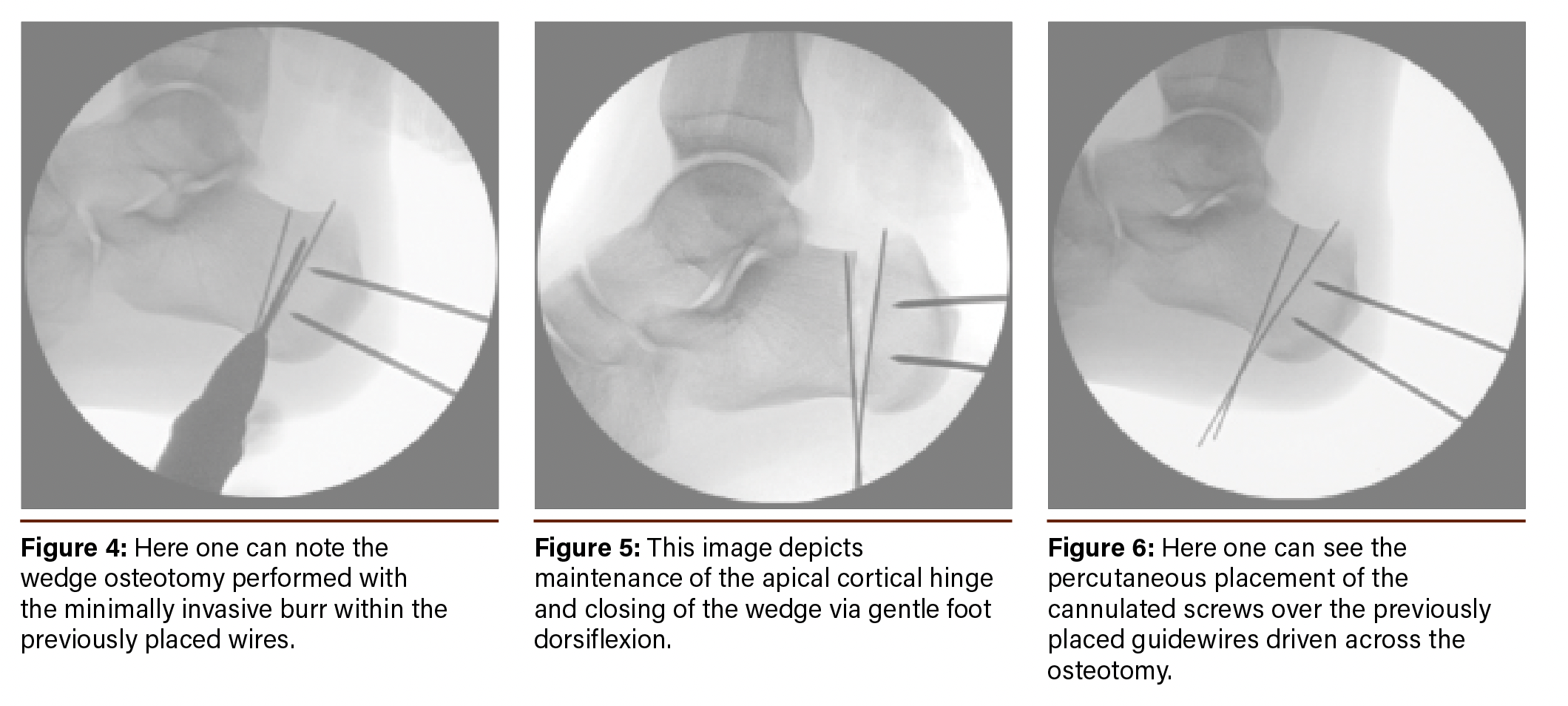
Patient placement is in a supine position with the heels off the edge of the bed. Standard prep, scrub, and drape of the operative limb takes place to the level of the proximal thigh. We do not utilize a tourniquet for this method, however, one can certainly place one. The high prep facilitates easy manipulation of the limb in internal and external rotation for surgery and fluoroscopy. Under image intensification, we place percutaneous wires through the inferior aspect of the calcaneus with an apex plantar and base dorsal (Figure 2). Next, we make a 1 cm incision on the lateral wall of the calcaneus and bluntly dissect down to bone. Subperiosteal dissection with an elevator in the path of the osteotomy is the next step. One can also place the guidewires for the compression screws at this time, with position being confirmed on the lateral and axial views (Figure 3).
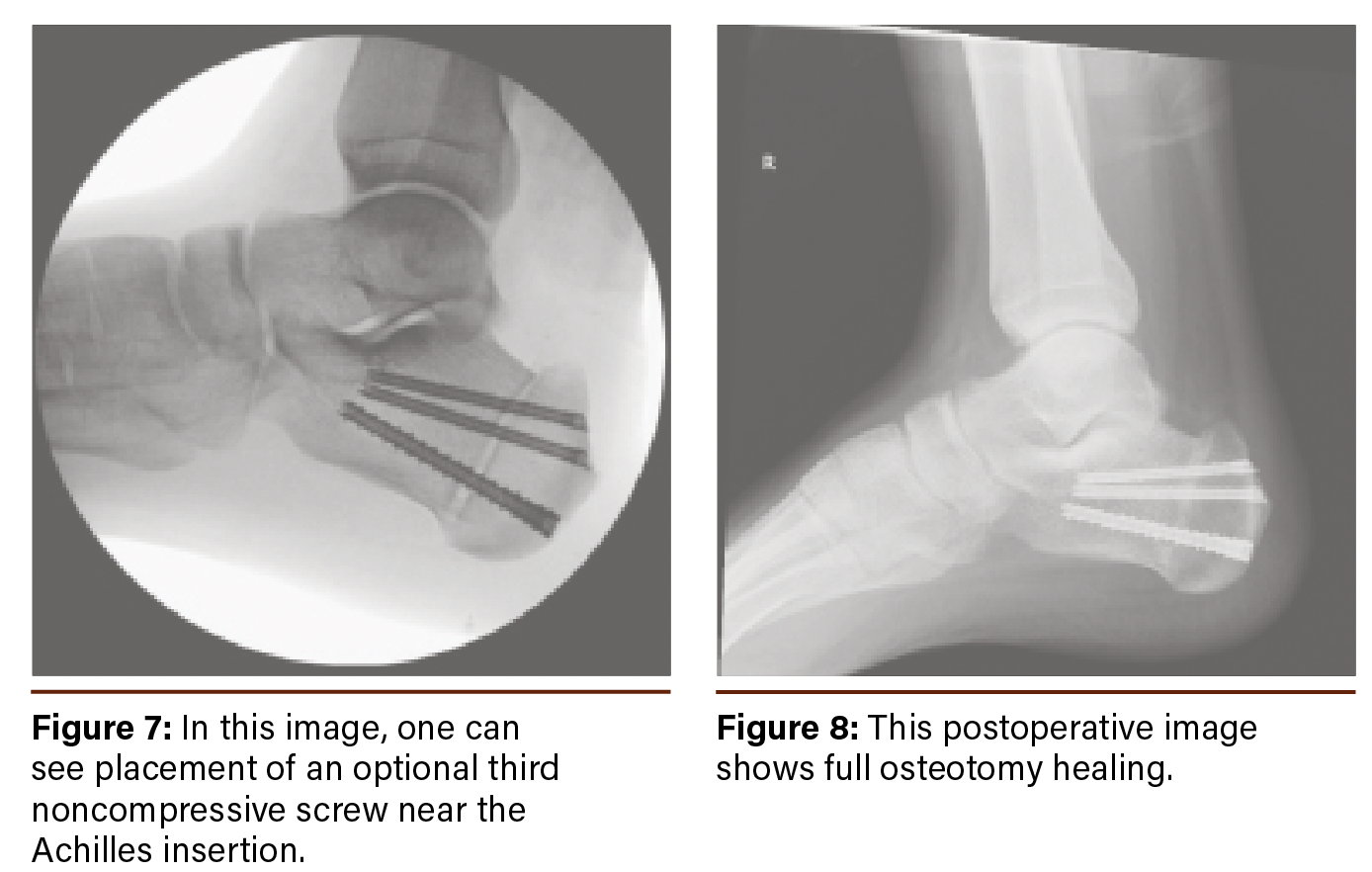
We then insert a minimally invasive surgical burr to create a closing wedge osteotomy (Figure 4). The posterior and anterior arms of the wedge are created first with no attempt to eliminate the bone. Once we are satisfied with the arms of the wedge, we proceed with a combination of a wedge and straight-cutting burr to pulverize the medullary content within the wedge. This takes place with continuous irrigation to minimize thermal injury. Throughout, we take care to leave a 5-8mm plantar hinge at the apex of the osteotomy. Then, we reduce the osteotomized segments by gentle dorsiflexion of the foot, allowing it to hinge on the plantar cortex before placing 2 cannulated screws from posterior to anterior (Figure 5). Additionally, we often place a third noncompressive screw for patients with a larger body habitus near the Achilles tendon insertion for added stability (Figures 6 and 7).
Patients are kept non-weight-bearing until suture removal. They are then fitted for a tall immobilization boot and allowed to partial weight-bear at first postoperative visit. They can typically transition out of the boot and into a regular sneaker between 6-8 weeks postop and resume full activity after 12 weeks.
Key Points Common Among Patients That Have Done Well With the MIS Zadek Procedure
In the authors’ experience, the below pearls establish a common thread among successful MIS Zadek procedures:
1. MRI exam is beneficial and can help guide the surgeon’s decision to perform the osteotomy in some scenarios:
- MRI findings with minimal involvement of the Achilles tendon. Such as, no significant interstitial tears or tendinopathy.
- No signs of calcific changes or bony enthesopathy at the attachment to the tendon
- Prominent bony edema at the insertion of the Achilles tendon without tendon involvement should be given high consideration for this method
2.
Maintaining an apical cortical hinge during wedge closure prevents plantar fascia strain and pain.
3.
Early mobilization/range of motion of the Achilles tendon postoperatively is helpful in recovery and helps maintain ankle the range of motion gained during the procedure (no additional posterior muscle group lengthening is performed with this method).
Addressing Chronic Right Heel Pain in a 25-Year-Old Patient
A 25-year-old male presented with chronic right heel pain that had been present for many months. Initial treatment included immobilization along with rest, ice, compression, and elevation (RICE) therapy by an outside provider. The referral at this time was for potential surgical intervention.
On physical exam we noted tenderness with palpation of the Achilles attachment on the calcaneus and with range of motion of the ankle in dorsiflexion and plantarflexion. Plain film X-rays did not show significant spurring, however a Haglund’s deformity was noted. Since the patient had not attempted physical therapy yet, we referred him there to work on flexibility and edema control. He also took time off from his job, which required him to be on his feet all day.
Unfortunately, he found no relief with this plan after several months of treatment. An MRI revealed no focal Achilles tears, but did show interstitial tendinosis with bone marrow edema (Figure 1). After reviewing multiple other treatment options, the patient elected to have surgery as outlined in the previous discussion (Figures 2-6). At the most recent follow-up he was ambulating without pain and working with physical therapy to improve strength and range of motion. He no longer experienced pain with palpation of the Achilles tendon at the calcaneal attachment or with range of motion of the ankle. He had been able to return to work without issue.
In Conclusion
Minimally invasive procedures continue to provide alternative methods of tackling difficult foot and ankle pathology. A minimally invasive dorsal closing wedge osteotomy of the calcaneus has certainly shown to be promising. Whether it replaces traditional methods to address Haglund’s deformity is not yet determined. However, in our experience, it is a viable method that can be utilized effectively if the patient has been correctly selected. This article can serve as an initial guide for those that are looking to determine which patient would benefit from this method as they expand their MIS skill set.
Acknowledgement: The images shared in this piece are copyright to Sinai Hospital of Baltimore, Inc. and are used with permission.
Dr. Siddiqui is a Fellow of the American College of Foot and Ankle Surgeons and practices with the International Center for Limb Lengthening, Rubin Institute of Advanced Orthopedics, Sinai Hospital of Baltimore, Baltimore, MD
Dr. Sato is a Fellow at the International Center for Limb Lengthening, Rubin Institute of Advanced Orthopedics, Sinai Hospital of Baltimore, Baltimore, MD
References
1.
Longo UG, Ronga M, Maffulli N. Achilles tendinopathy. Sports Med Arthrosc Rev. 2009;17(2):112-126. doi:10.1097/JSA.0b013e3181a3d625
2.
Ko VM, Cao M, Qiu J, et al. Comparative short-term effectiveness of non-surgical treatments for insertional Achilles tendinopathy: a systematic review and network meta-analysis. BMC
Musculoskelet Disord. 2023;24(1):102. Published 2023 Feb 7. doi:10.1186/s12891-023-06170-x
3.
Gaston TE, Daniel JN. Achilles Insertional
Tendinopathy- Is There a Gold Standard?. Arch Bone Jt Surg. 2021;9(1):5-8. doi:10.22038/abjs.2020.53988.2704
4.
Dilger CP, Chimenti RL. Nonsurgical
Treatment Options for Insertional Achilles Tendinopathy. Foot Ankle Clin. 2019 Sep;24(3):505-513. doi: 10.1016/j.fcl.2019.04.004. Epub 2019 May 22. PMID: 31371000; PMCID: PMC7216975.
5.
Chen J, Janney CF, Khalid MA, Panchbhavi VK. Management of Insertional Achilles Tendinopathy. J Am Acad Orthop Surg. 2022;30(10):e751-e759. doi:10.5435/JAAOS-D-21-00679
6.
Tourné Y, Francony F, Barthélémy R, Karhao T, Moroney P. The Zadek calcaneal osteotomy in Haglund’s syndrome of the heel: Its effects on the dorsiflexion of the ankle and correlations to clinical and functional scores. Foot Ankle Surg. 2022;28(6):789-794. doi:10.1016/j.fas.2021.11.001
7.
Hall S, Kaplan JRM, Schipper ON, et al. Minimally Invasive Approaches to Haglund’s Deformity and Insertional Achilles Tendinopathy: A Contemporary Review. Foot Ankle Int. 2024;45(6):664-675. doi:10.1177/10711007241237529
8.
Johnson KW, Zalavras C, Thordarson DB. Surgical management of insertional calcific achilles tendinosis with a central tendon splitting approach. Foot Ankle Int. 2006 Apr;27(4):245-50















