Study Proposes New Risk Score To Predict Amputation
 The severity of diabetes mandates vigilance against risk factors for amputation and a new study in Diabetes Care devises a new risk score to further physicians’ efforts at preventing complications.
The severity of diabetes mandates vigilance against risk factors for amputation and a new study in Diabetes Care devises a new risk score to further physicians’ efforts at preventing complications.
The study focused on 575 patients with infected diabetic foot ulcers, 28 percent of whom went on to amputation. The authors validated the prognostic value of the International Working Group on the Diabetic Foot and also developed a new risk score for physicians to use in practice, one for any amputation and one for amputations excluding the lesser toes.
Researchers also acknowledged the following independent risk factors for amputation: deep ulcers, increased exudate, foul smell, periwound edema, pretibial edema, fever and raised C-reactive protein levels.
Valerie Schade, DPM, says the study confirms the findings of previous studies. She uses similar risk management categories as those in the study, calling them essential in diagnosing the true severity of a patient with diabetes who presents with an infected foot.
Barry Rosenblum, DPM, notes the classification system in the study appears to subclassify the signs one would normally see with infection into predictive factors. He speculates whether physicians would use the risk score in a program to attempt to reduce the number of diabetic foot amputations.
Dr. Schade notes that approximately 50 percent of patients with diabetes with a severe foot infection, as defined by the Infectious Diseases Society of America (ISDA), will not present with systemic signs, making it difficult to determine patients who require emergent surgical incision, drainage and debridement. As she notes, determining infection severity requires a physician to look at all aspects of a patient’s history and physical examination, and laboratory and imaging studies.
“The subtle findings of a patient with an elevated heart rate and pain, edema and erythema on examination, and extreme hyperglycemia increase my concern for a severe infection even if the patient is afebrile and without an elevated white blood cell count,” says Dr. Schade, a Fellow of the American College of Foot and Ankle Surgeons, and the American College of Foot and Ankle Orthopedics and Medicine.
As Dr. Schade advises, patients who present with any concerns for a moderate or severe diabetic foot infection as defined by the IDSA require emergent surgical incision, drainage and debridement of all infected soft tissue and bone.
Dr. Rosenblum has found that risk factors for amputation are primarily the presence of infection and peripheral arterial disease.
“Early recognition of infection, which certainly may be consistent with the findings of the authors, may not only help to predict amputation but possibly prevent it. This is important as is the ability to recognize (and reverse) critical limb ischemia,” says Dr. Rosenblum, an Assistant Clinical Professor of Surgery at Harvard Medical School and the Associate Chief of the Division of Podiatric Surgery at Beth Israel Deaconess Medical Center in Boston.
Editor’s note: For further reading, see the DPM Blogs “The Importance Of Assessing Risk In Patients With Diabetes” at https://tinyurl.com/k4qbjzc or “Saving Two Feet In Three Minutes” at https://tinyurl.com/kbk75of .
Is Polydeoxyribonucleotide A Viable Option For Plantar Fasciitis?
By Brian McCurdy, Managing Editor
 A new study in International Orthopaedics suggests podiatric physicians may want to consider polydeoxyribonucleotide as a treatment for plantar fasciitis.
A new study in International Orthopaedics suggests podiatric physicians may want to consider polydeoxyribonucleotide as a treatment for plantar fasciitis.
The randomized study focused on 40 patients with plantar fasciitis with the patients being equally divided between those who received polydeoxyribonucleotide and those who received a normal saline injection once a week for three weeks. Researchers found patients who received polydeoxyribonucleotide had significantly improved Visual Analogue Scale scores and Manchester-Oxford Foot Questionnaire scores at both four and 12 weeks while the placebo group had no such improvements. The study authors noted no injection complications.
As Thomas Belken, DPM, explains, physicians have proposed polydeoxyribonucleotide as a broad spectrum, anti-inflammatory agent. Citing study data, Dr. Belken notes that polydeoxyribonucleotide’s anti-inflammatory effect comes from activating the adenosine receptor by decreasing inflammatory cytokines such as tumor necrosis factor alpha and interleukin 6, and increasing the anti-inflammatory cytokine interleukin 10.
Dr. Belken says preliminary studies are encouraging. The hypothesis is that polydeoxyribonucleotide leads to the stimulation of vascular endothelial growth factor (which stimulates new vessel formation and collagen synthesis) and decreases inflammatory cytokines, according to Dr. Belken, who is in private practice at Foot Healthcare Associates in Michigan.
In Dr. Belken’s practice, the advanced conservative treatment options for plantar fasciitis are: ultrasound-guided, platelet rich plasma injections, botulinum Type A injections (Botox, Allergan), extracorporeal shockwave and physical therapy modalities such as A-Stim (Abrexis) and the Graston technique.
When treating plantar fasciitis, Dr. Belken will lay out all of the treatment options at the start and tell patients to think about the treatment like steps and they will go up as many steps as needed to get them better. Shockwave and surgeries are the end of his treatment protocol. He alters the protocol slightly depending on the patient’s progress and demeanor.
“New treatment options such as polydeoxyribonucleotide not only break the cycle of inflammation but also increase vascularity to the site,” says Dr. Belken. “It may be that this increase in blood flow and the re-establishing of the normal healing process could lead to increased long-term successful outcomes for our patients with chronic recalcitrant plantar fasciitis.”
What Effect Does Age Have On Total Ankle Arthroplasty?
By Brian McCurdy, Managing Editor
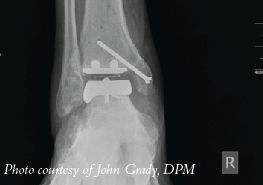
A new study in Foot and Ankle International concludes that among patients having total ankle arthroplasty, outcomes were the same as far as pain and physical performance regardless of age.
The study authors focused on 395 patients who had total ankle arthroplasty with a mean follow-up of 3.5 years. Researchers noted no differences in the Visual Analogue Scale pain score or the physical performance outcomes between the age groups. However, the study did find that patients under age 55 had a greater improvement in Short-Form 36 (SF-36) Vitality and American Orthopaedic Foot & Ankle Society (AOFAS) function scores in comparison with patients over 70.
In his experience performing total ankle arthroplasty procedures, Lawrence DiDomenico, DPM, notes that almost all patients feel a decrease in pain after arthroplasty regardless of age. As he explains, the older patient population fares the best because generally their activity level before and after the surgery is relatively lower in comparison to younger patients.
As a general rule, Dr. DiDomenico suggests using ankle implants in an older population, preferably those who are thin and have a low physical demand, although he notes this is subjective.
“Successful arthroplasty procedures do improve outcomes as the secondary effects on other joints are much better compared with arthrodesis over a long period of time,” says Dr. DiDomenico, the Section Chief of the Department of Podiatry at St. Elizabeth Hospital in Youngstown, Ohio. “(Arthroplasty) also provides a more normal gait compared to arthrodesis, given that the implant is successful.”











