A Rare Presentation of an Epidermal Inclusion Cyst Secondary to a Plantar Ulceration: A Case Report
Epidermal inclusion cysts (EICs) are common benign intradermal or subcutaneous soft tissue masses that form after implantation and proliferation of squamous epithelium secondary to trauma.1 Usually, this type of cyst will form after an inciting trauma to the pilosebaceous unit of a hair follicle.1 Therefore, it is rare to see an EIC form in glabrous skin, such as that seen in the palms of the hands and the soles of the feet.1 Locations with glabrous skin comprise less than 10 percent of EIC presentations, making diagnosis somewhat difficult due to this rarity.2
How exactly these inclusion cysts form in these unexpected anatomic locations is unclear. A theory exists that EICs in the glabrous skin may arise from Human Papilloma Virus (HPV) infecting the eccrine ducts,3 although further research is necessary in this area. Iatrogenic etiology following surgery4 is also discussed.
Early diagnosis and treatment of EICs are important due to the potential for malignant transformation, specifically into basal cell or squamous cell carcinomas.5,6 Additionally, while these benign lesions are generally asymptomatic, when on a load-bearing surface such as the sole of the foot, they can cause significant discomfort and impact the patient’s gait.
The aim of this case report is to highlight the management of an epidermal inclusion cyst which formed over the course of a year secondary to a healed ulceration in the glabrous skin of the foot that caused significant pain and negatively impacted gait.
Details From the Case
A 60-year-old male presented with a painful soft tissue mass on the plantar left foot near the third metatarsal head. The mass had been present for over one year, significantly increased in size over the previous six months, and was very painful. He was well known to the podiatry clinic, as a year prior he had been treated for and healed a plantar third metatarsal head ulceration, which had formed secondary to pressure from left foot drop. That ulceration had been minor, only breaking the top layer of skin and was less than 1.0 cm in diameter. The treatment course at that time included standard wound care and offloading, which resulted in the ulcer healing completely after a few weeks.
His past medical history included left foot drop secondary to trauma, resulting from a motor vehicle accident 25 years prior. He also had peripheral neuropathy treated with pregabalin, and a history of alcohol dependence. The patient had no history of past podiatric surgery. He had no known drug allergies, was not on anticoagulant therapy, and did not have a history of tobacco use. Review of systems was unremarkable.
The physical examination demonstrated palpable pedal pulses and diminished protective sensation bilaterally. The musculoskeletal and biomechanical exams revealed a complete loss of active dorsiflexion and noticeable muscle wasting and hammertoe deformities in the left foot. Pes planus was evident bilaterally, but otherwise the right foot was unremarkable. We noted a 2.4 x 2.4 x 1.6 cm oval-shaped, well-circumscribed, nonmobile soft tissue mass with a central punctum on the plantar aspect of the left third metatarsal head (Figure 1). There was no surrounding edema, erythema, or ecchymosis, and no clear open wound.

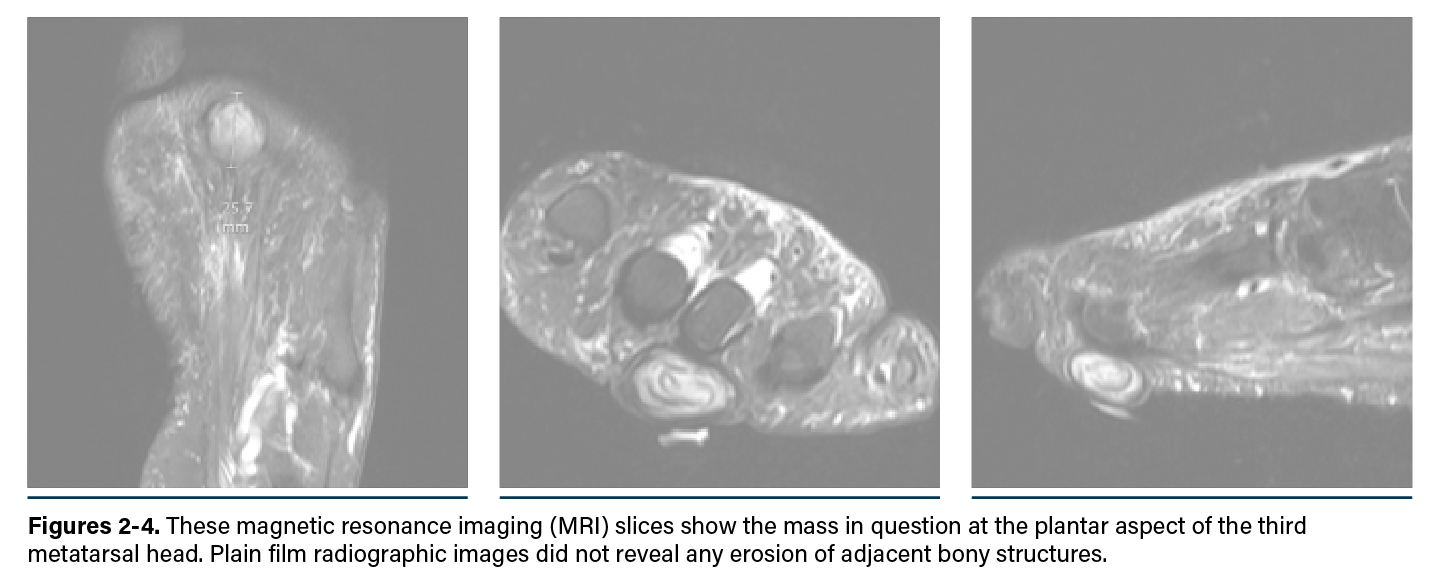
Radiographic images did not reveal any osseous erosion of adjacent structures (Figures 2-4). Magnetic resonance imaging (MRI) without contrast of the left foot favored a nonaggressive soft tissue lesion based on its morphological appearance, signal and enhancement characteristics, and thickness. The lesion was heterogeneous, with T2 hyperintense signal centrally and a T1/T2 hypointense signal at the periphery of the capsule.
Ancillary blood tests, including complete blood count (CBC) with differential, basic metabolic panel (BMP), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) showed no concerning findings for infection or systemic involvement. The patients glycosylated hemoglobin (HbA1c) was found to be 5.4.
Our differential diagnosis included a complex sebaceous cyst, stigmata of prior infection, foreign body granuloma formation, chronic hematoma, and non-aggressive soft tissue lesions such as complex plantar fibroma and other subdermal lesions.
We discussed both surgical and nonsurgical treatments in-depth with the patient including continued observation with offloading and padding, minimally invasive diagnostic options like needle aspiration and punch biopsy, and gold standard definitive treatment with complete surgical excision. The patient elected to pursue complete surgical excision.
Notes on the Surgical Course
After a local anesthetic block, we prepped and draped the left foot in the usual aseptic manner, and applied a pneumatic ankle tourniquet with ample cast padding. We then created a 4.0cm curvilinear incision beginning distal to the mass within the toe sulcus (Figure 5). Protecting neurovascular structures and maintaining hemostasis, we dissected down to the soft tissue mass and performed an en bloc excision. The mass was excised in its entirety without rupture. The mass was round, with a pearly luster, felt firm and solid throughout, and had not penetrated any deep structures beyond the subcutaneous layer.

We then sent the soft tissue mass for pathology and examined the surgical site thoroughly for any further abnormalities, noting none. We flushed the area with copious sterile saline and reapproximated the deep structures utilizing 3-0 absorbable suture. Skin closure was with 3-0 nylon and we also administered a 1 mL injection of 10mg/mL dexamethasone sodium phosphate. The dressing included betadine-soaked Owen silk, sterile gauze, cast padding, and an elastic compression bandage. Due to the location of the incision, the patient was instructed to maintain non-weight-bearing on his left foot for two weeks and protect the surgical site with a postoperative shoe.
The pathology report noted a pale gray-tan cystic structure measuring 2.6cm x 2.4cm x 1.3cm, which upon sectioning contained grumous gray-tan material. Microscopic examination confirmed a diagnosis of an epidermal inclusion cyst (Figure 6).

The patient followed up three days postop at our clinic, where we reviewed the pathology results and examined the surgical site. The patient continued to offload his left foot and perform regular dressing changes for two more weeks, after which we removed the sutures and progressed him to full weight-bearing. The patient healed well from the procedure and had only minimal scarring from the surgical incision.
Several months following the initial removal surgery, the patient was seen for follow up and found to have a new mass the same location. MRI without contrast revealed the new mass measured 3.6 x 2.3 x 1.3cm, approximately 33% percent larger than the original. Following the same preoperative, surgical, and postoperative protocols as the original lesion, we excised this new mass in its entirety and intact. Pathology examination confirmed another epidermal inclusion cyst. The patient healed well from this second procedure with only minimal scarring at the surgical incision site and has now had over one year since the last surgery without reoccurrence.
Important Points to Consider
Epidermal inclusion cysts are benign lesions that typically respond well to total excision. However, they are rarely observed on non-hair-bearing surfaces of the body, such as the sole of the foot. This rarity underscores the importance of conducting a thorough patient history and physical examination to develop a comprehensive differential diagnosis, minimizing the risk of overlooking uncommon presentations. Care must be taken to avoid rupturing the cyst or performing an incomplete excision, as these actions can lead to recurrence or the formation of keratin granulomas. This case study contributes to the limited number of reported instances of epidermal inclusion cysts occurring on the plantar aspect of the foot. It is interesting to note that the patient had a history of ulceration at the site of the subsequent epidermal inclusion cyst, a history which may have induced its growth. We suspect that as the pressure ulceration healed, epidermal cells were trapped in the dermis, continued to proliferate and produce keratin, and formed the EIC.
When presented with this case, our goals of therapy were to alleviate the patient’s discomfort, confirm our diagnosis with surgical pathology, and to completely excise the soft tissue mass to avoid future complications. The outcome of this case supports surgical excision as the treatment of choice for EICs. Imaging obtained at the end of the therapeutic period, along with the physical exam, demonstrated no reoccurrence of the soft tissue mass after the second procedure. The patient experienced full pain resolution and full restoration of limb function and gait. This case report demonstrates the novel theory of EIC formation secondary to ulceration.
Dr. Lagstein and Dr. Evensen are third-year residents in the Department of Veteran Affairs at Southern Arizona Veteran Affairs Healthcare System in Tucson, Arizona. Dr. Jacobson is a second-year reident in the same Department and Healthcare System.
Dr. Walters is a Diplomate of the American Board of Foot and Ankle Surgery and a podiatrist in the Department of Veteran Affairs at Southern Arizona Veteran Affairs Healthcare System in Tucson, Arizona.
The authors of this article declare no conflict of interest.
This material is based upon work supported by the Department of Veterans Affairs, Veterans Health Administration, and Office of Research and Development. The authors gratefully acknowledge the Southern Arizona VA Health Care System which provided facilities and materials for this research.
References
1. Ramakrishnaiah SB, Rajput SS, Gopinathan NS. Epidermoid cyst of the sole: a case report. J Clin Diagn Res. 2016;10(11):PD06–PD07.
2. Posthuma JJ, de Winter T, Schotanus MGM. Traumatic epidermal inclusion cyst after minimally invasive surgery of a displaced intra-articular calcaneal fracture: a case report. J Foot Ankle Surg. 2018;57(6):1253–1255.
3. Egawa K, Honda Y, Inaba Y, et al. Detection of human papillomaviruses and eccrine ducts in palmoplantar epidermoid cysts. Br J Dermatol. 1995;132(4):533–542.
4. Skolnik J, Pontious J, Hasenstein T. Development of multiple epidermal inclusion cysts after radiofrequency microtenotomy for plantar fasciitis: a case report. J Foot Ankle Surg. 2021;60(5):1088–1093.
5. Coulter PD, Bouché RT. Traumatically induced inclusion cyst secondary to shoe impingement: report of three cases. J Foot Ankle Surg. 1999;38(4):271–277.
6. Sheff J, Bregman P, Curran T. Bilaterally symmetrical epidermal inclusion cysts with foreign-body giant-cell reaction. J Am Podiatr Med Assoc. 1988;88(8):410–413.
7. Harish S, Jan E, Ghert M, et al. Pseudotumoural appearance of a ruptured epidermal cyst in the foot. Skeletal Radiol. 2006;35(11):867–861. doi:10.1007/s00256-006-0168-3.















