CDC: Infection Prevalence Down In Hospitals
By Brian McCurdy, Managing Editor
 A recent National and State Healthcare-Associated Infections Progress Report notes that nearly all hospital-related infections experienced “significant reductions” in 2013 at the national level, according to the Centers for Disease Control and Prevention (CDC).
A recent National and State Healthcare-Associated Infections Progress Report notes that nearly all hospital-related infections experienced “significant reductions” in 2013 at the national level, according to the Centers for Disease Control and Prevention (CDC).
Specifically, between 2011 and 2013, the CDC points to an 8 percent decrease in hospital-onset methicillin resistant Staphylococcus aureus (MRSA) and a 10 percent decrease in hospital-onset Clostridium difficile. The report also notes a 46 percent decrease in central-line associated bloodstream infections between 2008 and 2013, and a 19 percent decrease in surgical site infections in 10 procedures tracked during the same time period.
“Effective infection prevention techniques can be both some of the easiest and most difficult tasks for healthcare providers to perform,” notes Valerie Schade, DPM. As she notes, proper hand hygiene remains the keystone to infection prevention. To help minimize the risk of infection transmission, Dr. Schade emphasizes appropriate gowning, gloving, use of personal protective equipment and disposable medical equipment, and thorough cleaning of non-disposable equipment.
Dr. Schade, Ryan Fitzgerald, DPM, and Craig Breslauer, DPM, FACFAS, CWS, emphasize appropriate hand hygiene techniques and educating patients and physicians on hygiene. Dr. Breslauer comments that many hospitals ask patients to wash the night before surgery with antibacterial soap. As Dr. Schade notes, research has shown that proper hand hygiene by patients and their support network is a cost-effective and successful intervention to prevent transmission of pathogens.
“All healthcare staff should make the performance of proper hand hygiene part of providing patient care,” stresses Dr. Schade.
Patients with MRSA or C. difficile infections should have a private room with contact precautions in place, according to Dr. Schade, a Fellow of the American College of Foot and Ankle Surgeons and the American College of Foot and Ankle Orthopedics and Medicine. Likewise, Dr. Fitzgerald, an Assistant Professor of Surgery at the University of South Carolina School of Medicine in Greenville, S.C., says one should utilize appropriate contact precautions in those patients who have been placed in isolation.
Drs. Schade and Breslauer say these precautions include mandatory gowns, gloves and masks as applicable prior to entering the room and performing proper hand hygiene prior to entering and leaving the room. Dr. Schade warns that alcohol gels do not inactivate C. difficile spores. Although she cites studies showing that the increased use of alcohol gels is not associated with an increase in C. difficile infections, she recommends hand washing as opposed to isolated use of an alcohol gel.
In addition, Dr. Breslauer stresses close adherence to the protocols in place for the use of prophylactic antibiotics before surgery. When treating infections, physicians should use organism-specific antibiotic therapy and avoid more broad spectrum or newer, powerful antibiotics when not indicated, according to Dr. Breslauer, who practices at South Florida Orthopaedics & Sports Medicine in Florida.
Although we most frequently consider pathogen spread as direct contact between the patient and their provider within the patient’s room, Dr. Schade says indirect transmission can occur via provider and surface contact both in the patient’s room and throughout the hospital, such as on sofas, chair backs, hand rails and isolation carts. She says frequent surface wiping of these items can aid in reducing the potential for pathogen transmission.
Credentialing Guidelines Proposed For Podiatrists To Use HBOT
By Brian McCurdy, Managing Editor
Acknowledging the increasing number of podiatrists incorporating hyperbaric oxygen therapy (HBOT) into the treatment of diabetic foot ulcers and other conditions, authors of a recent article in the Journal of the American Podiatric Medical Association propose new guidelines for hospital credentialing of DPMs for HBOT.
For initial HBOT privileging, the authors propose completing a 40-hour course of HBOT safety and proctoring 10 HBOT dives. To renew privileges, DPMs should have supervised more than 25 dives in the past 24 months and completed an eight-hour refresher course on HBOT, according to the authors. The article notes that a majority of states allow podiatric physicians to prescribe and supervise HBOT although the Undersea and Hyperbaric Medicine Society cannot certify DPMs.
Kazu Suzuki, DPM, CWS, calls the proposed requirements “sufficient and realistic,” saying they are on par with the HBOT classes designed for MDs and DOs by many wound care center management companies.
“I do believe this is an excellent first step in DPM credentialing in HBOT supervision and this will be a stepping stone in establishing a nationwide acceptance for DPMs to supervise non-emergent HBOT sessions,” says Dr. Suzuki.
David Swain, DPM, agrees, saying that as someone who oversees HBOT use, the recommended credentialing would be easy for DPMs to obtain and sufficient for adequate supervision. He suggests also requiring a minimum of two hours of CMEs related to HBOT per year to maintain privileges.
“I would like the ability for podiatrists to oversee HBOT of any body part or condition in the future,” says Dr. Swain, a co-founder of the First Coast Center for Amputation Prevention in Jacksonville, Fla. “I would also like to eventually see a board certification in HBOT available to DPMs as this would further legitimatize our role with this treatment modality.”
However, Dr. Suzuki does not believe the credentials will lead to more podiatrists using HBOT as supervision rights for DPMs are limited by the state scope of practice. He cites data in the article saying more than 15,000 non-emergent HBOT sessions have had supervision by non-MDs or DOs such as DPMs, with no serious adverse events or patients requiring the emergency department.
“DPMs are in the frontline of diabetic foot management and limb preservation in this country, and I believe it only make sense that we actively participate in the process of HBOT supervision,” says Dr. Suzuki, the Medical Director of the Tower Wound Care Center at Cedars-Sinai Medical Towers.
How Many Weeks Of Antibiotics Are Enough For Osteomyelitis?
By Brian McCurdy, Managing Editor
 Physicians have debated how long a course of antibiotics one should prescribe for non-surgical treatment of osteomyelitis. A recent study in Diabetes Care suggests that six weeks is sufficient and 12 weeks may be overkill.
Physicians have debated how long a course of antibiotics one should prescribe for non-surgical treatment of osteomyelitis. A recent study in Diabetes Care suggests that six weeks is sufficient and 12 weeks may be overkill.
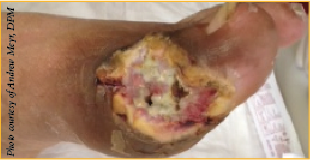
The study focused on 40 patients, evenly divided between those receiving six weeks or 12 weeks of antibiotics for osteomyelitis. Remission of osteomyelitis occurred in a total of 26 patients (12 in the six-week group and 14 in the 12-week group). Researchers defined remission as wound healing for more than four weeks, absence of recurrent infection at the initial site or at adjacent rays, and no need for surgical bone resection or amputation at the end of a follow-up period of at least 12 months after completing antibiotic treatment.
For Nicholas Bevilacqua, DPM, the optimal management of osteomyelitis combines surgical and medical management. However, in select patients, he may consider six weeks of antibiotics. These patients include those with forefoot involvement, those without severe or necrotizing soft tissue infection, and those without peripheral arterial disease.
The advantages of a shorter duration treatment of six weeks are a lower cost and fewer adverse effects caused by the antibiotic therapy, according to Dr. Bevilacqua, a Fellow of the American College of Foot and Ankle Surgeons, who is in private practice with North Jersey Orthopaedic Specialists in Teaneck, N.J.
The study notes that fewer study patients using six weeks of antibiotics experienced gastrointestinal events in comparison to patients on a 12-week regimen. Dr. Bevilacqua notes that in addition to gastrointestinal events, those taking a longer duration of some antibiotics are also at risk for adverse laboratory abnormalities.











