What’s Evolving in Podiatric Dermatology: Research and Tools to Elevate Practice
As podiatrists, we see firsthand how common nail and skin conditions of the foot can have a surprisingly complex backstory. From nail thickening and ingrown nails to plantar keratoses and fissures, what may look straightforward at first glance often reveals a deeper interplay of biomechanical stress, systemic health, and, in some cases, infectious causes. A wave of recent dermatology and podiatry research is helping us rethink how we approach these conditions in daily practice.
An Overview of the Contemporary Research
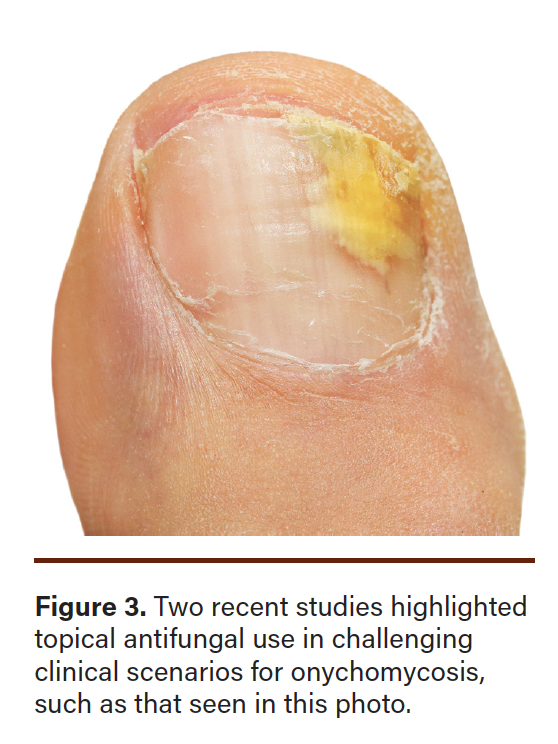
An area of continuing interest is onychomycosis. A 2025 study published in Mycoses by Lipner and colleagues showed that topical efinaconazole remains highly effective in patients over 65, a group often unable to tolerate oral antifungals.1 In addition, a 2024 review by Pandit and team reassured clinicians that they can safely and effectively use efinaconazole even when patients wear nail gel cosmetics, making it easier for patients to stay consistent with treatment.2
In the realm of nail trauma, a simple tool is gaining new relevance. Hill and colleagues, in a 2025 Journal of the American Academy of Dermatology article, described how the Brannock device, long used in shoe stores and in many of our practices, can uncover subtle foot length differences that contribute to nail problems like retronychia or pincer nails.3 Often overlooked, these slight size discrepancies can lead to chronic microtrauma when patients wear shoes that only fit one foot properly.
Other skin-related research is expanding our role in systemic care. A 2024 study in Scientific Reports used nailfold videocapillaroscopy (NVC) to detect early microvascular changes in patients with type 2 diabetes.4 Their findings linked specific capillary changes to diabetic nephropathy, suggesting that dermatologists and podiatrists may one day use NVC as a noninvasive tool to assess systemic microvascular health in patients with diabetes—well before foot complications arise.
Finally, our understanding of intractable plantar keratosis (IPK) is evolving. A 2024 study published in the Journal of Medical Virology by Iannuzzi and team revealed that some IPKs may have a viral component, specifically human papillomavirus (HPV).5 This discovery challenges the assumption that these lesions are purely mechanical, opening the door to potential antiviral therapies in select cases.
These studies remind us that even the most common foot concerns—whether thickened nails, painful calluses, or persistent lesions—deserve a closer look. By blending insights from dermatology, biomechanics, systemic health, and infectious disease, podiatrists can continue to lead in diagnosing and treating the often-overlooked dermatologic conditions that affect our patients’ feet every day.
A Deeper Dive Into Onychomycosis Insights
Onychomycosis remains a common and challenging condition in podiatric practice, especially among older adults and in patients who would like to pursue cosmetic coverage while treating. Recent advances have focused on improving efficacy and patient adherence through topical therapies. Two recent studies shed light on the benefits and practical considerations of efinaconazole 10% solution in diverse clinical scenarios.
The first study, a post hoc analysis of 2 pivotal Phase III trials, evaluated adults aged 65 to 71 years that received treatment with daily efinaconazole or vehicle for 48 weeks.1 This research demonstrated achievement of complete cure (defined as no clinical involvement along with mycologic cure) in 13.6 percent of the efinaconazole group compared to only 3.6 percent of the vehicle group. Additionally, this study showed complete or almost complete cure (≤5 percent involvement plus mycologic cure) in 19.1 percent versus 5.4 percent, respectively. The researchers also reported solely mycologic cure in 59.2 percent of the efinaconazole group compared to 12.5 percent of the control group. Another notable finding in the study was that patients treated with efinaconazole demonstrated significantly greater new nail growth. Safety outcomes were favorable, with only 6 percent of patients reporting treatment-related adverse events, comparable to the overall safety profile observed in broader clinical trials.1 These findings underscore the relevance of topical efinaconazole for older patients, especially those with comorbidities or contraindications to oral antifungals.
The second study, a narrative review, explored whether gel nail polish interferes with the efficacy of efinaconazole.2 It included both in vitro and clinical research, including a prospective trial that combined efinaconazole with gel nail polish over 6 months in 9 adults. The study found that efinaconazole 10% solution effectively penetrated the nail regardless of whether traditional nail polish was present.2 A 52-week clinical study revealed similar improvements in onychomycosis outcomes regardless of polish use. In the gel polish study, all patients achieved mycologic clearance and demonstrated visible improvement without compromising polish appearance.2 These findings suggest that patients can continue using gel nail polish during treatment with efinaconazole without reducing its therapeutic effect.
From a clinical perspective, these studies offer valuable guidance for podiatrists. Topical efinaconazole 10% solution represents a treatment option for older patients and those with underlying conditions that preclude oral antifungal therapy. Allowing patients to wear nail cosmetics during treatment can also improve adherence, especially for those concerned with the visual appearance.
Using the Brannock Device for Nail Issues
Podiatrists frequently encounter traumatic nail disorders in practice, often presenting with onycholysis, pincer nails, onychauxis, and ingrown nails. These conditions may stem from overt trauma or more commonly from chronic, low-grade mechanical forces tied to gait abnormalities and foot structure discrepancies. For many patients, particularly those who cannot recall a specific traumatic event, the mystery of nail damage becomes a frustrating barrier to both diagnosis and recovery.
A recent clinical report published in the Journal of the American Academy of Dermatology highlights a deceptively simple, yet insightful, approach: measuring foot length with the Brannock device.3 Traditionally used in shoe stores, this tool offers precise measurements of foot length, width, and arch. In clinical practice, it provides a quantifiable method to assess foot length discrepancies that might otherwise go unnoticed during routine physical exams. A difference as small as half a shoe size—roughly one-third of an inch—can lead to abnormal foot loading and toe compression, ultimately contributing to nail plate trauma and deformity.
The authors describe a case of a female patient with retronychia affecting the left great toenail. Using the Brannock device, they discovered that the affected foot was a half size larger than the unaffected right foot. While visually subtle, this difference had practical consequences for footwear fit and function.3 Such findings emphasize the importance of precise foot measurement in evaluating unexplained or chronic nail pathology.
Contributing factors like obesity, aging, and pregnancy may further alter foot structure and resilience over time. The loss of toe spacing and changes in soft tissue padding in older adults, for instance, can increase susceptibility to mechanical nail trauma. Despite these risks, most patients wear shoes based on perceived rather than measured size, sometimes exacerbating nail deformities unknowingly.
While some have occasionally used the approach of drawing foot outlines on to highlight improper shoe fit, this method lacks reproducibility and quantifiable data. In contrast, the Brannock device offers clinicians and patients a consistent, visual explanation for how anatomical asymmetries might contribute to onychodystrophy. Moreover, advising patients to wear the larger of 2 shoe sizes when discrepancies exist can be a simple intervention with meaningful outcomes. Though the device cannot correct underlying foot deformities, it empowers patients to make smarter footwear choices that reduce ongoing trauma.
For podiatrists, incorporating Brannock measurements into nail disorder evaluations adds minimal time but considerable clinical value. It provides patients with a concrete, actionable insight into their condition and supports better patient education regarding proper shoe selection. As the field increasingly appreciates nails as dynamic, biomechanically sensitive structures, such practical tools align with a more nuanced understanding of nail health.
Ultimately, this approach reminds clinicians that sometimes the best diagnostic innovations are those that reconnect us with simple, foundational principles. Accurate measurement, individualized assessment, and thoughtful patient education remain pillars of effective care. With tools like the Brannock device, podiatrists are better equipped to reduce trauma-induced nail disorders and improve long-term outcomes for their patients.
The Role of Visualization of Nailfold Capillaries and Type 2 Diabetes
Nailfold videocapillaroscopy (NVC) is an emerging tool that may enhance podiatrists’ ability to detect early microvascular changes in patients with type 2 diabetes. A recent cross-sectional study highlights its relevance for identifying systemic complications such as diabetic nephropathy through noninvasive evaluation of nailfold capillaries.4 This article explores the implications of these findings for clinical practice in podiatric medicine.
Microvascular complications of diabetes, including nephropathy, retinopathy, and neuropathy, remain leading causes of morbidity. While podiatrists routinely assess peripheral circulation and neuropathic risk, tools that provide insight into systemic microvascular damage are not widely integrated into clinical practice. Nailfold videocapillaroscopy, a noninvasive imaging technique used to visualize capillaries at the nailfold, may bridge this gap.
A recent 2024 study published in Scientific Reports evaluated the relationship between nailfold capillary abnormalities and renal function in patients with type 2 diabetes,4 suggesting that podiatrists could leverage this method to enhance diabetes risk stratification and care coordination.
The study analyzed 453 adults with type 2 diabetes using NVC to identify and score structural abnormalities in nailfold capillaries.4 The research team correlated these results with renal function markers, including estimated glomerular filtration rate and urinary albumin-to-creatinine ratio. Participants with advanced kidney disease, particularly those with an eGFR below 30 mL/min/1.73 m², exhibited a significantly higher burden of capillary abnormalities, including comma-shaped and ramified capillaries. Patients with high levels of albuminuria also demonstrated shorter capillary loops and more severe structural changes. Capillary dropout and tortuosity were especially prevalent among individuals with lower renal function, signaling microvascular damage that could precede or coincide with nephropathy progression.4
The authors concluded that NVC may serve as an early, noninvasive indicator of microvascular dysfunction in diabetes, especially for individuals with developing or established kidney disease.4 These insights offer significant clinical utility for clinicians who frequently encounter patients at risk for both systemic and lower-extremity complications.
Although NVC is more traditionally employed in rheumatology and dermatology for evaluating conditions like systemic sclerosis, its application in diabetic care could be increasingly relevant for podiatric clinicians. The nailfolds, easily accessible during routine foot exams, offer a unique view into systemic microvascular health. For podiatrists managing patients with diabetes, especially those with comorbidities such as hypertension or chronic kidney disease, capillaroscopic findings could support more personalized and proactive care.
These findings may help in identifying patients at higher risk for nephropathy or retinopathy, justify earlier referrals to specialists such as nephrologists or endocrinologists, and reinforce the need for more aggressive management of glycemic control, blood pressure, and foot protection. Furthermore, NVC is non-invasive, repeatable, and relatively affordable once equipment is in place, making it a practical tool for both private practices and larger clinical institutions.
However, one must acknowledge several limitations. Accurate interpretation of NVC images requires adequate training and standardization. Availability of the technology within podiatric practices may also currently be limited. Moreover, while the correlation between nailfold changes and nephropathy is compelling, further longitudinal research is needed to determine whether these findings can predict foot-specific outcomes such as ulceration or
amputation risk.
Despite these challenges, the integration of interdisciplinary diagnostic tools such as NVC aligns with the evolving role of podiatrists as frontline providers in chronic disease management. As podiatric care continues to overlap with dermatologic and vascular health, technologies like NVC may enhance comprehensive diabetic assessment.
This study underscores the diagnostic potential of nailfold videocapillaroscopy in identifying early microvascular changes in patients with type 2 diabetes. For podiatrists, this technique represents a novel opportunity to visualize systemic microvascular health during routine foot exams, offering early indications of underlying complications such as nephropathy. As access to this technology expands, NVC may become an adjunct to standard diabetic foot screening and a valuable tool in multidisciplinary care delivery.
The Relationship Between IPKs and Plantar Warts
Persistent intractable plantar keratosis (IPK) continues to frustrate both patients and clinicians. Despite standard interventions such as offloading, debridement, and topical keratolytics, these lesions frequently recur or resist treatment altogether. A new study published in the Journal of Medical Virology introduces an important paradigm shift by proposing a viral etiology in a subset of these lesions.5 Specifically, the study suggests a strong association between IPK and human papillomavirus (HPV), a virus more commonly linked with plantar warts.
In this study, researchers analyzed plantar keratotic tissue from patients whose lesions failed to resolve after routine mechanical and supportive interventions. Using polymerase chain reaction (PCR) assays, they detected HPV DNA in a significant number of cases. The findings challenge the long-held belief that IPK arises exclusively from chronic mechanical pressure and friction. Notably, several identified HPV strains overlapped with those typically implicated in cutaneous warts, indicating a potential diagnostic overlap between refractory corns and masked viral lesions.
This emerging evidence has important implications for podiatric practice. First, it invites a reconsideration of the diagnostic process for persistent hyperkeratotic lesions. If HPV is a contributing factor in select cases of IPK, clinicians may need to employ diagnostic tools such as dermoscopy, histopathology, or PCR testing in recalcitrant presentations. Second, therapeutic approaches may need to expand beyond mechanical care. Antiviral strategies including cryotherapy, topical therapies, and laser may offer relief for patients with virally mediated keratoses. These modalities could reduce recurrence and improve long-term outcomes when conventional treatments fail.
For podiatrists, this research also reinforces the importance of clinical vigilance and flexibility. Not all thickened plantar lesions are created equal, and misclassification may delay appropriate intervention. The typical diagnostic dichotomy between warts and corns may no longer be sufficient. Instead, practitioners should approach persistent keratotic lesions with a broader differential diagnosis, particularly when typical offloading and debridement do not yield sustained improvement.
The integration of PCR and other diagnostic tools into standard podiatric workflows remains aspirational for many practices due to cost and accessibility. While this study focused on a relatively small patient cohort, it raises a compelling hypothesis that warrants further investigation through multicenter trials. Confirming HPV’s role in persistent plantar keratoses could significantly shift therapeutic algorithms and improve quality of life for patients struggling with these stubborn lesions.
Ultimately, this research encourages podiatrists to think beyond the mechanical and embrace a more nuanced, microbiologically informed approach to plantar skin pathology. Persistent plantar keratosis may no longer be viewed strictly as a pressure problem but as a dermatologic condition with potential viral underpinnings. By expanding our diagnostic and therapeutic toolkit, we are better positioned to deliver comprehensive, lasting care for our patients.
Final Thoughts
Recent literature related to lower extremity dermatology has provided interesting nuances and insights for consideration in podiatric practice. This could challenge practitioners to question long-held paradigms associated with common pedal skin conditions. Hopefully, by employing an evidence-based approach and thoughtfully incorporating new thinking where applicable, these emerging insights could advance care and patient outcomes.
Dr. Vlahovic is a Professor at Samuel Merritt University College of Podiatric Medicine in Oakland, CA.
Disclosure: The author is a consultant for OrthoDermatologics.
1. Lipner SR, Gupta AK, Joseph WS, Elewski B, Guenin E, Vlahovic TC. Efficacy and safety of efinaconazole 10% topical solution for treatment of onychomycosis in older adults: A post hoc analysis of two phase 3 randomised trials. Mycoses. 2025;68(5):e70069.
2. Pandit B, Elewski B, Vlahovic TC. Concealing meets healing in the treatment of toenail onychomycosis: A review of concurrent nail polish use with topical efinaconazole 10% solution. J Clin Aesthet Dermatol. 2024;17(9):38-42.
3. Hill RC, Axler E, Forman CA, Lipner SR. Use of the Brannock device to detect differences in foot length in patients with traumatic nail disease. J Am Acad Dermatol. 2025;92(3):e45-e46.
4. Takehara K, Shinohara Y, Wada T, et al. Association between nailfold videocapillaroscopic findings and diabetic nephropathy in type 2 diabetes: A cross-sectional study. Sci Rep. 2024;14:13625.
5. Alou L, Becerro-de-Bengoa-Vallejo R, Losa-Iglesias ME, et al. Strengthening the relationship between intractable plantar keratosis and human papillomavirus. J Med Virol. 2024;96(2):e29431.















