Tibiofibular Fixation With Total Ankle Replacement: A Case Series
Total ankle replacement (TAR) has been a mainstay along with ankle arthrodesis for surgical treatment of end-stage ankle primary and post-traumatic arthritis, paralleling each other ever since the 1990s.1 Implants have improved over time and patient selection has become more precise over this time. Specifically, newer implants better replicate ankle joint anatomy.1 First-generation implants consisted of 2 components, a polyethylene tibial component and a metal talar component. These required large amounts of bone resection and eventually became abandoned because of high failure rates. The second rollout of implants were almost all semi-constrained, cementless, and used porous coatings. The third generation incorporated a 3-part mobile bearing system.2 Furthermore, fourth-generation implants focused on improving outcomes, minimizing bone resection, biomaterials, surface coatings, and preoperative navigation systems.3
The first total ankle replacement system to be approved by the Food and Drug Administration (FDA) was a second-generation implant called the Agility (DePuy Orthopaedics) total ankle system prosthesis.2 This converted a 3-bone joint into a 2-bone joint by utilizing tibiofibular arthrodesis. It also provided an increased surface area for tibial component fixation.4 The Agility total ankle replacement appears to have relatively successful outcome rates reported in the literature, showing relatively low rates of radiographic hindfoot arthritis and revision procedures at an average of 9 years.5 The senior surgeon’s early use of and personal success with the Agility total ankle implant inspired him to adapt similar techniques, such as tibiofibular fixation, to enhance stability in newer-generation implants.
To the authors knowledge, there is no literature reported on utilizing syndesmotic fixation or arthrodesis as an adjunctive procedure with newer generation implants. We propose that by utilizing syndesmotic fixation and/or arthrodesis with newer total ankle replacement systems, surgeons can work to provide better longevity of the implant through additional stability and better control in the frontal plane. From our experience, we feel this may be especially useful for patients at higher risk of implant failure.
Thoughts on the Technique
For a lateral approach with a third-generation trabecular metal implant, the same incision, surgical technique, and fibular bone cut are utilized regardless of whether one performs tibiofibular joint fixation or fusion. If arthrodesis is undertaken, the surgeon uses a rongeur, curette, high-speed burr, and osteotomes to resect the syndesmosis proximal to the fibular bone cut. Due to the converging nature of the tibia and fibula at this level, this resection creates a characteristic “Christmas tree”–shaped excision.
If only fixation is planned, the surgeon proceeds with the standard lateral total ankle replacement technique. Once the implant is properly seated within the ankle mortise, the surgeon repairs the fibula and incorporates syndesmotic fixation into the lateral plate. The senior author typically utilizes 2 to 4, 3.5 mm screws, placed 2–4 cm proximal to the ankle mortise. Insertion of these screws is in the standard 30-degree posterior-to-anterior orientation and typically cross 4 cortices.
The postoperative course remains relatively unchanged. However, in the senior author’s most recent 20 total ankle replacements that included syndesmotic fixation or fusion, only 30% of patients required hardware removal. Hardware-related complications were rare and typically limited to occasional symptomatic hardware necessitating removal.
Key Cases to Consider
The senior surgeon will typically reserve adjunctive tibiofibular fixation with total ankle replacement for patients with noted laxity/instability, frontal plane deformity, and/or patients with obesity. Arthrodesis is typically considered in patients deemed higher risk, particularly those with more significant frontal plane malalignment. As previously noted, the senior surgeon developed this idea from previous use of tibiofibular arthrodesis with the Agility total ankle replacement system. He expanded this idea to newer generation implants, in hopes of possibly enhancing implant longevity in patients potentially more prone to implant failure. The total ankle system he most commonly uses for this technique involves a lateral approach and a trabecular metal third-generation implant. We present a representative series of such cases below. All 3 cases included patients with body mass index (BMI) of over 33. Ages of the patients highlighted ranged from 45–75 years.
The first patient was a 55-year-old female with diabetes who initially sustained a fracture-dislocation of the left ankle, requiring open reduction and internal fixation. She later underwent hardware removal and ankle arthroscopy due to persistent pain and progressive joint degeneration. Even after these interventions, she suffered from severe post-traumatic arthritis of the ankle (see preoperative X-rays in Figures 1a and 1b) and had exhausted conservative treatment options. The patient underwent total ankle replacement with adjunctive tibiofibular fixation. Anteroposterior and lateral radiographs at a follow-up of 7 months and 12 days showed adequate alignment of the ankle mortise with maintenance of the ankle implant (Figures 1c and 1d). At final follow-up, she exhibited excellent range of motion, was pain-free, and ambulated well in regular shoe gear.

The second patient suffered from severe osteoarthritis of the tibiotalar joint with frontal plane valgus deformity (Figures 2a and 2b). Anteroposterior and lateral radiographs at 10 months and 25 days postoperatively showed maintenance of the ankle implant with no malalignment in the frontal plane (Figures 2c and 2d). At final follow-up, this 75-year-old female demonstrated painless range of motion, had returned to normal activities in regular shoe-wear, and reported no ongoing pain.
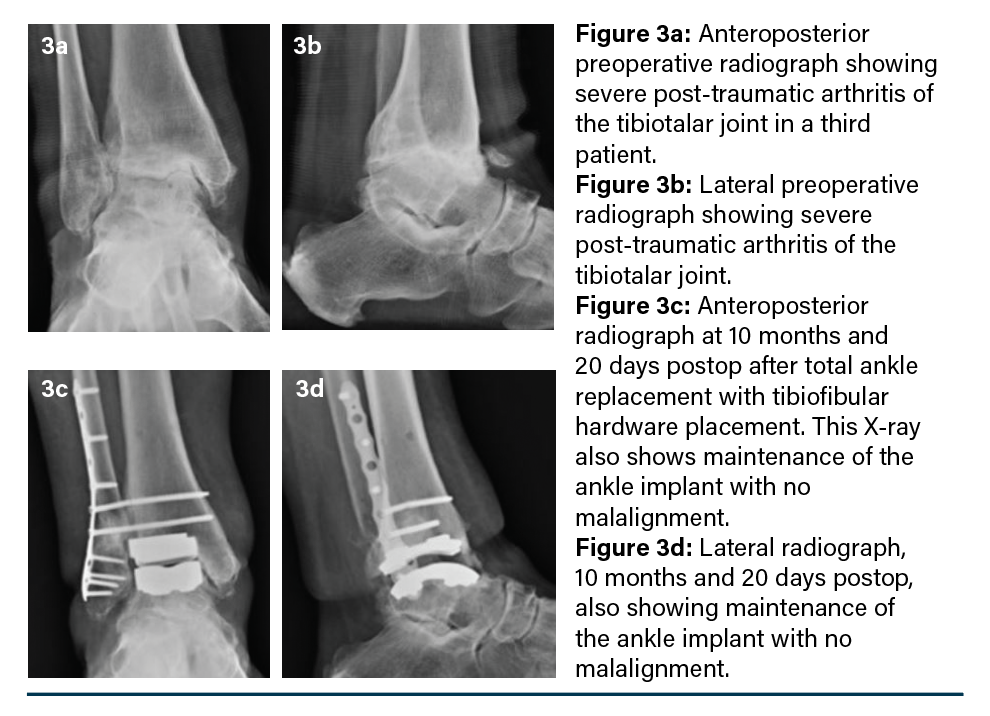
The third patient, a 47-year-old female, initially sustained a fracture-dislocation of the left ankle, treated with open reduction and internal fixation. The hardware was subsequently removed, and she underwent ankle arthroscopy. Despite these interventions, she continued to experience pain and discomfort, with progressive joint degeneration (Figures 3a and 3b). She eventually underwent total ankle replacement with adjunctive tibiofibular fixation. At a follow-up of 10 months and 20 days anteroposterior and lateral radiographs (Figures 3c and 3d) showed maintenance of the ankle implant with no malalignment. At final follow-up, the patient reported no pain and had returned to full activity. Clinically, the foot and ankle remained stable and maintained a plantigrade position.
As demonstrated above, all 3 patients progressed well postoperatively and at final follow-up all ambulated freely with no ankle pain. None of the discussed patients required syndesmotic hardware removal or exchange.
Further Insights
Total ankle replacement is a challenging, yet rewarding, procedure. Published literature has shown improved outcomes with newer generation implants, including longer implant survivability. Results show survivorship at around 89% at 10 years.6 Studies that include and analyze patients with obesity show mixed results. Bouchard and team found revision rates of over 17% in patients with obesity at a mean follow-up of 3.76 years.7 Schipper and colleagues evaluated 97 patients, including those with obesity, and showed a major revision rate of over 20 percent and an implant failure rate of over 17 percent at 5-year follow-up.8
In Conclusion
Of note, the senior surgeon has performed tibiofibular fixation with total ankle replacement frequently over the previous 10 years and has not seen any implant failures or ankle malalignment when using tibiofibular fixation. We believe, from our experience, that by utilizing tibiofibular fixation and/or arthrodesis with newer generation total ankle replacements, we can work towards increased stability and control in the frontal plane. We feel this may increase longevity of the implant and potentially reduce implant failure in higher-risk patients. Further prospective studies are necessary to evaluate this concept and to better understand the impact of this approach.
Dr. King is an Associate of the American College of Foot and Ankle Surgeons and practices at the NOMS Foot and Ankle Center in Boardman, OH.
Dr. DiDomenico is a Fellow of the American College of Foot and Ankle Surgeons and practices at the NOMS Foot and Ankle Center in Boardman, OH.
<div class="riddle2-wrapper" data-rid-id="cGfCeIZK" data-auto-scroll="true" data-is-fixed-height-enabled="false" data-bg="#fff" data-fg="#00205b" style="margin:0 auto; max-width:100%; width:640px;" ><script src="https://www.riddle.com/embed/build-embedjs/embedV2.js"></script><iframe title="082825 PT TibFib Intent" src="https://www.riddle.com/embed/a/cGfCeIZK?lazyImages=false&staticHeight=false" allow="autoplay" referrerpolicy="strict-origin"></iframe></div>
1. Vickerstaff JA, Miles AW, Cunningham JL. A brief history of total ankle replacement and a review of the current status. Med Eng Phys. 2007;29(10):1056-1064.
2. Bonasia DE, Dettoni F, Femino JE, et al. Total ankle replacement: why, when and how? Iowa Orthop J. 2010;30:119-130.
3. Prissel MA, Consul D, Thompson MJ. Keys to maximizing outcomes with fourth-generation total ankle replacements.
Podiatry Today. 2021;34(1). Available at: https://www.hmpgloballearningnetwork.com/site/podiatry/keys-maximizing-outcomes-fourth-generation-total-ankle-replacements. Accessed August 13, 2025.
4. Mulcahy H, Chew FS. Current concepts in total ankle replacement for radiologists: complications. Am J Roentgenol. 2015;205(6):1244-1250. doi:10.2214/AJR.14.14171
5. Knecht SI, Estin M, Callaghan JJ, Zimmerman MB, Alliman KJ, Alvine FG, Saltzman CL. The Agility total ankle arthroplasty: seven to sixteen-year follow-up. J Bone Joint Surg Am. 2004;86(6):1161-1171.
6. Zaidi R, Cro S, Gurusamy K, et al. The outcome of total ankle replacement: a systematic review and meta-analysis. Bone Joint J. 2013;95-B(11):1500-1507. doi:10.1302/0301-620X.95B11.31633
7. Bouchard M, Amin A, Pinsker E, et al. The impact of obesity on the outcome of total ankle replacement. J Bone Joint Surg Am. 2015;97(11):904-910. doi:10.2106/JBJS.N.00837
8. Schipper ON, Denduluri SK, Zhou Y, Haddad SL. Effect of obesity on total ankle arthroplasty outcomes. Foot Ankle Int. 2016;37(1):1-7. doi:10.1177/1071100715604392















