Utilizing Implantable Loop Recorders in the Management of Atrial Fibrillation
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of EP Lab Digest or HMP Global, their employees, and affiliates.
Featured is the presentation entitled " Utilizing Implantable Loop Recorders in the Management of Atrial Fibrillation" by Sana M. Al-Khatib, MD, MHS, FHRS, from Session 6 at the 2025 Western AF Symposium.
Clinical Summary
- Design/population: Per Western AF Symposium 2025, Session 6 (presentation), Sana M. Al-Khatib reviewed clinical use of implantable loop recorders (ILRs)/insertable cardiac monitors (ICMs) for atrial fibrillation (AF) management across U.S. practice, drawing on observational studies, guidelines, and ongoing trials (adult AF populations, including post-ablation and cryptogenic stroke).
- Key outcomes: ICMs enable continuous characterization of AF (burden, recurrence, pattern/density) and ventricular rate control. Observational evidence presented suggests higher AF detection compared with conventional monitoring. Ongoing and planned studies are using ICMs to inform post-ablation management and antithrombotic strategies, with outcomes including clinically overt stroke, systemic embolism, and imaging-detected cerebrovascular events.
- Clinical relevance/limits/next steps: Guidelines support ICM use (e.g., visual EGM confirmation; class IIa after cryptogenic stroke). Limits include battery life (~3.5 years), sensing/classification errors, connectivity, and cost; AI has reduced false positives. Future directions include integrating risk-factor monitoring (activity, metabolic metrics).
Reviewed by Jodie Elrod, Managing Editor
Transcripts
It's such a great pleasure for me to be with you today. This is one of my favorite meetings to attend. I'd like to start by wholeheartedly thanking Nassir for trusting me with the fellowship part of this meeting and for inviting me to present on this topic.
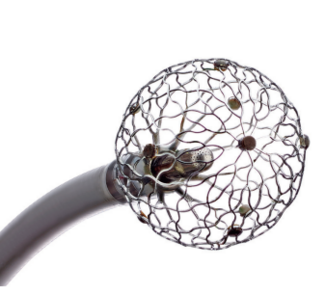
I will be talking about how implantable loop recorders (ILRs) can be utilized to manage patients with atrial fibrillation (AFib). As we all know, we have many different types of devices to monitor patients for AFib, ranging from Holter and event monitors, to wearables, to handheld electrocardiograms, to cardiac implantable electronic devices (CIEDs) including ILRs or insertable cardiac monitors. In this talk, I'm going to focus on the use of ICMs for managing patients with AFib.
Before I move on in my talk, I'd like to ask the audience a question. With a show of hands, how many of you use an ICM in all patients with AFib who do not have a CIED device? Okay, no one. How many of you actually use an ICM in some patients with AFib? Yes, some of us do, of course. How many of you never use ICM for managing AFib? Okay, well, that's what I would have expected. Thank you.
Let me move on and talk about the use of ICMs in the US. This was a really interesting study that was conducted by Dr Ken Ellenbogen's son. As you see here, he showed an exponential rise in the use of ICMs in the US. This study just goes to 2018. However, there is no reason to suspect that those trends have not continued because there are more uses for ICMs that technology is improving and we all have seen value that we derive from using ICMs in many of our patients.
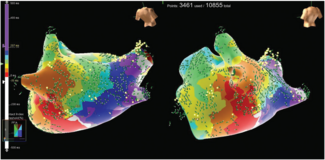
So, what information can an ICM provide to help inform management of AFib? The first thing is, of course, as we try to control the rhythm, it is very important to accurately assess the burden of AFib, recurrences of AFib, pattern, clustering of AFib, also referred to as density, and when patients go into AFib, we want to make sure that their ventricular rate is not too fast. In fact, my colleague, Suneet Mittal, published this interesting paper on the use of ICMs in AFib. These are really nice figures that show you the different patterns of AFib: the left top showing just one isolated episode of AFib, the right top showing frequent recurrences of paroxysmal AFib, the bottom left showing clustering of AFib, and then we have a perfect example of persistent AV. This is so helpful to us as clinicians to use these data.
As we define the pattern, the burden density of AFib, this can help us have informed discussions with our patients and make the right recommendations for them to really enable them to make the best decisions for themselves. As we monitor the control of rate in AFib, it's very important to have this information as well.
I know that you've seen this figure time and again today. It's actually such a nice figure in the most recent AHA/ACC/HRS guideline for managing patients with AFib. This highlights the 3 pillars of AFib, and as we all know, the ICM helps us a lot with that third pillar, which is basically rhythm control, rate control.
I do want to give you this one example, and there are several other examples of studies that have looked at the use of ICMs to monitor patients for developing AFib. This particular study was actually focused on patients undergoing ablation for atrial flutter. As we all know, a lot of those patients move on to develop AFib. In this particular study, you see that patients who received an ILR versus people who were in the conventional monitoring arm were much more likely to be diagnosed with recurrent AFib because we're more able to catch AFib promptly and then treat those patients accordingly.
That's all good in terms of rhythm control. What about ICM use for stroke intervention in patients with AFib? This of course refers to the first pillar of AF management. Here, we want to briefly talk about this trial. There have been many other trials that are now going—you heard about the SMILE-AF trial—but there are other trials that are indeed implementing the ICM to look for recurrences of AFib. This is just one example of patients who are indeed enrolled within 12 months or more than 12 months after an AFib ablation, and they undergo some testing at baseline. Then after enrollment, some of these patients are undergoing ICM implantation and they're being randomized to aspirin versus rivaroxaban with this follow-up, again, looking at the inclusion of criteria mentioned here, CHA2DS2-VASc score of 1 or more. These are adult patients with nonvalvular AFib. The primary outcome is a composite of all clinically overt stroke, systemic embolism, incident stroke detected by brain MRI. This is so important to be able to correlate some of those outcomes with what these investigators observe on the ICMs. Again, this is just one example. There are many other examples of trials using this.
What does the AF guideline document tell us about ICMs? There are actually several recommendations in the guidelines, the first of which here in patients with an intracardiac rhythm device capable of a diagnosis of AFib. A diagnosis of AFib should only be made after you visually look at the intracardiac tracings (EGMs). This is incredibly important. All of us know this. I don't think I need to mention it, but there are other things that could mimic AFib—such as noise or far-field oversensing—so always make sure to look at the EGMs yourself. This is mostly for the trainees. And keep in mind that if you have patients who have had a cryptogenic stroke, putting an ICM in those patients to look for AFib is indeed a class IIA recommendation. I think probably all of us in this room do implant ICMs for that indication. Then of course, among patients with a diagnosis of AFib, the topic of this talk, it is reasonable to infer AF frequency duration burden using these different modalities, but the ICM is mentioned here as well. So certainly, the guidelines support us in doing so.
Now, it is important to highlight some potential limitations of ICM use. Of course, as we all know, the battery is not indefinite. Three and a half years is probably what you will get from the best devices on the market. That's still pretty good in my view compared with other modalities. Of course, you have issues with sensing, either oversensing or undersensing, but with the improved technology, we're seeing fewer of those episodes in a human patient. Again, inaccurate classification of AFib is an issue, especially trying to distinguish that from other types of atrial arrhythmias.
We used to have a really high number of false positives, but now with the advent of AI incorporated into ICMs, that number has gone down. Also, we need to ensure connectivity and all of that and costs have to be taken into account. However, I do find ICMs to be pretty easy to use in a lot of patients in my clinic.
The last thing I want to leave you with is trying to look into the future. I'm very excited about the potential uses of ICM for the second pillar of AF management, which is basically controlling risk factors for AFib. We heard about that all morning, almost all day today. How do you control these risk factors? So, I look forward to seeing what the vendors will be able to incorporate into the ICMs. For example, can we start tracking people's activity, can we monitor glucose levels, or other things? I think the sky is the limit. So, we'll see what the future brings.
The transcripts have been edited for clarity and length.