Leading Pulsed Field Ablation Integration in a High-Volume Electrophysiology Program: An Interview With Sandeep Goyal, MD
An Interview With Sandeep Goyal, MD
An Interview With Sandeep Goyal, MD
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of EP Lab Digest or HMP Global, their employees, and affiliates.
EP LAB DIGEST. 2026;26(2):7-9.
Interview by Jodie Elrod
In this interview, Sandeep Goyal, MD, medical director of the electrophysiology (EP) lab at Piedmont Healthcare, discusses how Piedmont Healthcare has integrated 2 key technologies shaping the future of atrial fibrillation (AF) treatment: the Affera™ mapping and ablation system and the PulseSelect™ pulsed field ablation (PFA) system (Medtronic). Dr Goyal shares insights on system selection, workflow optimization, safety considerations, and how these technologies complement each other in both simple and complex AF ablations across a multi-hospital network.
Can you provide an overview of the EP program at Piedmont Healthcare, including annual procedural volume and procedure types performed?
 At Piedmont Healthcare, we have a large, multi-hospital EP program with high-volume tertiary referral labs serving the Atlanta, Athens, and Augusta regions. We also operate smaller EP labs at 3 hospitals—Piedmont Fayette, Piedmont Henry, and Piedmont Cartersville—giving us a broad, statewide footprint. Across the system, we perform several thousand EP procedures each year, including nearly 4000 catheter ablations, approximately 1000 left atrial appendage occlusion (LAAO) procedures, and close to 4000 device implants. Both ablation and LAAO volume continues to grow at a rapid pace.
At Piedmont Healthcare, we have a large, multi-hospital EP program with high-volume tertiary referral labs serving the Atlanta, Athens, and Augusta regions. We also operate smaller EP labs at 3 hospitals—Piedmont Fayette, Piedmont Henry, and Piedmont Cartersville—giving us a broad, statewide footprint. Across the system, we perform several thousand EP procedures each year, including nearly 4000 catheter ablations, approximately 1000 left atrial appendage occlusion (LAAO) procedures, and close to 4000 device implants. Both ablation and LAAO volume continues to grow at a rapid pace.
My primary practice is based at the Piedmont Heart Institute, where I serve as the medical director for the EP lab at Piedmont Atlanta Hospital (PAH). PAH is a quaternary referral center for complex ablations, LAAO, and lead management. At PAH, we perform around 2000 catheter ablations, approximately 600 LAAO procedures, and about 1000 device implants each year. Because our focus at the main hospital is on ablations and LAAO, our device volume is proportionally smaller compared with the broader system.
What key factors or considerations have guided your decision-making when selecting PFA technologies for your practice?
When PFA became available, especially with multiple systems coming online, it prompted important internal discussions about which platform would best meet our needs. We evaluated systems with strong efficacy data from IDE studies and, where available, durability data from real-world experience. We then placed significant emphasis on safety, as one of our major reasons for adopting PFA was to enhance the safety of catheter ablation for AF. Specifically, we examined rates of coronary spasm, hemolysis, perforation risk, and cerebrovascular events. In parallel, we sought platforms that offered procedural versatility, allowing a range of ablation strategies to be performed within a single ecosystem. Collectively, these factors guided our decision-making process.
We decided to partner most extensively with Medtronic, particularly at Piedmont Atlanta, because they were able to offer an ecosystem that included both a safe and effective platform like the PulseSelect catheter as well as a more versatile system capable of mapping, ablating, and remapping within the same workflow using the Affera mapping and ablation system and Sphere-9™ catheter platform (Medtronic). We also wanted partners with a strong commitment to innovation—organizations that are forward-thinking about the future of EP and AF ablation and are actively expanding their portfolios to address non-AF arrhythmias such as ventricular tachycardia and supraventricular tachycardias. Medtronic has consistently demonstrated that commitment, which was a key factor in choosing their ecosystem as our primary platform.

What are the main factors that influence your choice of ablation technology—for example, considerations related to patient selection and cost?
In day-to-day practice, my choice of technology is driven by the patient’s phenotype, their known anatomy, and their overall risk profile. For patients who we anticipate will require pulmonary vein isolation (PVI) only, the PulseSelect system is an excellent fit. It allows us to perform PVI efficiently, safely, and effectively. We also have strong safety data with the PulseSelect catheter, particularly its low risk of perforation. This safety profile has made it possible to use the PulseSelect system at some of our sites that are not equipped for cardiac surgery, where safety considerations are even more critical.
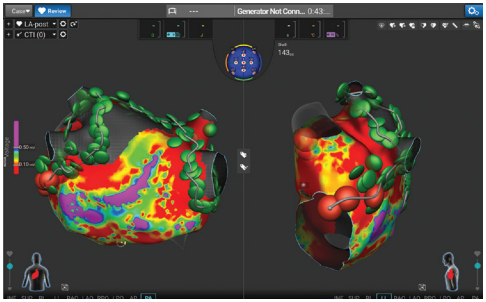
At Piedmont Atlanta, a large proportion of our patients require more extensive mapping and non-PV ablation—whether due to persistent or late-persistent AF, redo procedures, or atypical flutters. These are the cases where the Affera mapping and ablation system and Sphere-9 catheter really stand out. The ability to rapidly map, deliver ablation, and immediately remap using the same catheter—combined with the option for dual-energy delivery—makes it especially well-suited for these more complex scenarios.
When evaluating cost, our focus is on the total value delivered by a system rather than the disposable cost in isolation. We consider factors such as procedure duration, lab throughput, anesthesia time, complication rates, and the likelihood of redo procedures. From both a hospital perspective and a population health standpoint, a system that is more effective and more efficient often proves to be less expensive over time than a system with lower upfront costs but longer procedures, higher complication rates, or less durable outcomes. At the same time, we remain very mindful of stewardship and work closely with our C-suite to ensure they understand the rationale for adopting new technologies, particularly as these innovations require institutional approval.
How does access to both PF and radiofrequency (RF) energy with the Sphere-9 catheter influence your workflow during ablation procedures?
Historically, we used primarily an RF-based approach for ablation and were accustomed to using a single ablation catheter for the majority of ablation procedures. With the growing body of safety and efficacy data supporting PFA-based PVI, we were eager to incorporate PFA into our practice. However, we are a highly safety-conscious program, and based on available data, we were not comfortable performing PFA lesions near the annulus because of concerns regarding coronary spasm. As a result, when using single-shot PFA technologies, cases that required more than PVI necessitated the addition of a separate RF catheter to perform ablation near the annulus. While effective, this approach reduced procedural efficiency, required catheter exchanges, and increased overall cost.
The Sphere-9 catheter aligned well with our established workflow by addressing these limitations. The ability to perform cavotricuspid isthmus (CTI) or mitral isthmus ablation near the coronary arteries and seamlessly toggle to RF on the same catheter significantly improves both efficiency and safety by eliminating catheter exchanges. This dual-energy capability has allowed us to maintain a conservative safety posture while streamlining procedures and optimizing resource utilization.
This approach also reduces cost because we are not purchasing a separate RF catheter in addition to a PFA catheter. There are also cases where we want to stack energy sources; in those situations, we can seamlessly switch—either applying RF after PFA or vice versa—to achieve durable lesion formation. The availability of both RF and PFA in a single catheter has had a significant positive impact on our workflow. It has improved efficiency and has enabled us to perform most cases with essentially zero fluoroscopy and without catheter exchanges.
How does the PulseSelect PFA system complement or enhance your EP lab’s capabilities when used alongside the Affera mapping and ablation system?
The PulseSelect PFA system became available first, and we initially adopted it as our primary PFA system; the Sphere-9 catheter was introduced later. I view the PulseSelect system and Affera mapping and ablation system as complementary technologies, each serving different roles and patient populations. The Sphere-9 catheter provides high-density mapping and dual-energy ablation, while the PulseSelect catheter excels at efficient, standardized PVI in appropriately selected AF patients. It is a particularly compelling option when the goal is rapid and safe isolation without the need for extensive mapping.
In addition, the PulseSelect system provides important operational flexibility across our procedure suites. It can be deployed in alternate rooms when the Affera mapping and ablation system is reserved for more complex AF cases. Its open-platform architecture allows seamless integration with existing mapping systems, including CARTO (Johnson & Johnson MedTech) and EnSite NavX (Abbott). This interoperability enhances case scheduling, optimizes utilization of available resources, and enables us to consistently align the most appropriate technology with each patient while maintaining efficient lab operations.

Can you describe your workflow when using the Sphere-9 and PulseSelect catheters, including catheter preparation and visualization strategies?
Much of our workflow is built on common foundations: we consistently perform procedures on uninterrupted anticoagulation, rely on ultrasound-guided venous access, intracardiac echocardiography (ICE)–guided transseptal access, and place strong emphasis on meticulous catheter and sheath preparation. With the Sphere-9 catheter, once we obtain venous access and complete the transseptal puncture, we typically use a standard fixed-curve sheath for PVI ± CTI cases, or a steerable sheath (8.5 French [F] inner diameter), depending on operator approach. We are very deliberate about de-airing both the sheath and the catheter system before entering the LA, and we ensure the ACT is close to 350 or higher.
Once in the LA, we create a rapid map of the chamber and proceed with PVI, often performing substrate-based non-PVI ablation or targeting atypical flutter. Then, we can return to the right atrium (RA) to perform a CTI line and other RA mapping and ablation.
What has been particularly notable in my experience is that, for PVI ± CTI cases, the entire procedure can be performed using just 2 venous access sites. By leveraging the vector propagation arrows within the Affera mapping and ablation system to confirm conduction block across ablation lines, I can avoid the routine placement of a coronary sinus catheter. This streamlines the workflow and meaningfully reduces vascular risk by eliminating one of the 3 access sites typically required. In more complex ablation cases, however, we continue to place a coronary sinus catheter to provide additional reference and confirmation, as it remains valuable in those procedural contexts.
I believe the PulseSelect catheter is a more dedicated PVI tool. We use the FlexCath Contour™ steerable sheath and the FlexCath Cross™ transseptal solution (Medtronic) for transseptal access. One of the advantages I appreciate with the PulseSelect catheter is that it functions as an effective mapping catheter on its own. Particularly when we are using EnSite, we do not always use a dedicated mapping catheter because the PulseSelect catheter provides reliable mapping capability by itself.
We make extensive use of 3-dimensional mapping and ICE to guide catheter positioning within the PVs. The catheter is safe and easily maneuverable, provided we maintain a wire outside the system as recommended. In our lab, we follow a slightly modified workflow: while we perform the 4 ostial lesions recommended by the clinical trials, we typically add 6 antral lesions for the superior veins and about 5 to 6 for the inferior veins. In our experience, this approach improves single-pass isolation and enhances durability.
At the end of the case, we generally perform mapping again using the PulseSelect catheter. Early on, we routinely used a dedicated high-density mapping catheter, but over time we have found that it is not necessary in most cases. This has helped standardize our setup and has made the procedure more efficient and effective, with a low complication rate.
How would you describe your experience with catheter and sheath handling, such as maneuverability, stability, and overall ease of use during procedures?
With the Sphere-9 catheter, we are able to use a standard, 8.5F, fixed-curve sheath for many cases because the catheter is highly maneuverable, has a good steering mechanism, and is extremely stable—even with significant cardiac motion. Once positioned, it holds its place well and delivers consistent lesions. Many operators prefer using fixed sheaths for nearly everything, whereas I tend to take a more tailored approach, using fixed sheaths for PVI ± CTI only and reserving steerable sheaths for more complex procedures.
The PulseSelect catheter is also very easy to maneuver. It is one of the safest catheters we use because it is atraumatic, allowing it to be directed in any orientation without concern for injury to cardiac structures. Its optimized sheath minimizes air entrainment, making sheath management less challenging than with some other systems. The catheter’s anterior tilt is particularly helpful—it enables good contact throughout different portions of the PV as the catheter is rotated, providing excellent versatility. One point of caution is to avoid over-rotation, which can occasionally deform the catheter and require withdrawal and reinsertion. However, with growing experience, this occurs far less frequently, and we now rarely encounter this issue.
What insights or practical advice would you share with physicians who are in the process of evaluating or adopting PFA technologies?
My recommendation is to begin by carefully evaluating PFA systems and determining which platform best fits your environment. Then, start with straightforward, well-selected paroxysmal AF cases with favorable anatomy. This will allow operators to focus on mastering catheter behavior, becoming comfortable with ICE imaging, and establishing a consistent workflow before progressing to more complex cases.
One critical lesson we have learned is the importance of investing heavily in team training—not just physician training. Physicians and industry partners should conduct extensive dry runs with the team covering catheter preparation, de-airing techniques, anticoagulation strategy, and anesthesia coordination. When PFA was introduced, we transitioned to a 100% general anesthesia approach with paralysis, which represented a significant shift from prior practice. It is also important to anticipate pauses and have medications such as atropine and nitroglycerin readily available.
Using extensive ICE early in the learning curve is invaluable; you gain tremendous insight by watching catheter movement in real time. Standardizing protocols for transseptal access, catheter preparation, anticoagulation, and safety checks ensures that the entire lab operates as a cohesive unit, reducing variability. Within that standardized framework, physicians can still individualize lesion delivery and system selection. Establishing this balance of standardized and flexible elements is key to achieving consistently strong outcomes.
Tracking your own results is equally important. Monitoring procedure times, fluoroscopy use, complications, and redo rates helps you understand which catheter

systems perform best for your patient population in your hands. Although cost should not be the primary driver, it must be thoughtfully considered. Engaging executive leadership early, clearly articulating the clinical and operational value of emerging technologies, and demonstrating responsible resource stewardship are critical. Ultimately, matching the right technology to the right patient—and evaluating platforms based on overall value rather than disposable cost alone—is fundamental to successful adoption and long-term sustainability.
The transcripts were edited for clarity and length.
Disclosures: Dr Goyal has completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest. He reports consulting fees from Medtronic, Boston Scientific, Abbott, and Biosense Webster, and support for attending meetings and/or travel from Medtronic, Boston Scientific, and Abbott.
This content was published with support from Medtronic.











