Roadmap Imaging in the Endovascular Treatment of Complex Peripheral Vascular Disease
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Ivana Kumar1; Anshita Kumari, MBBS2; Kusum Lata, MD, FACC, FSCAI3
1Research Associate, Sutter Health, Tracy, CA; Quarry Lane School, Dublin, CA
2Kasturba Medical College, Manipal, India; Research Associate, Sutter Health Tracy, CA
3Interventional Cardiology; Board of Trustees, SCAI; Sutter Health, Tracy, CA
Disclosure: The authors report no conflicts of interest regarding the content herein.
The authors can be contacted via Kusum Lata, MD at lata.drkusum@gmail.com.
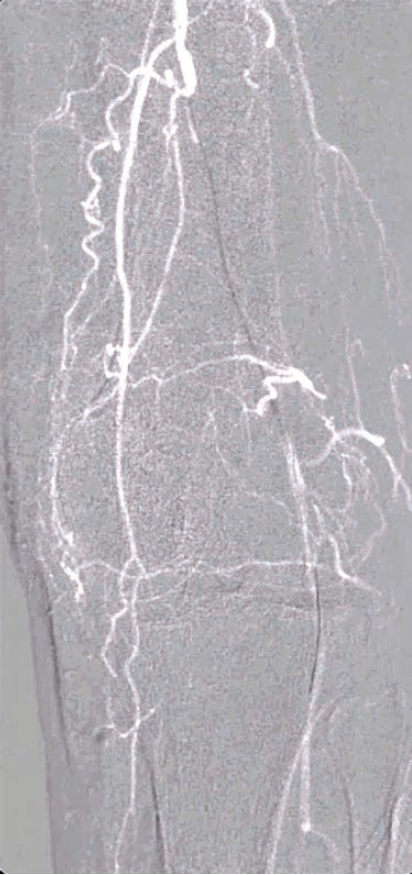
Peripheral vascular disease (PVD), specifically in its more advanced forms such as chronic limb-threatening ischemia (CLTI), presents a great clinical challenge. Endovascular interventions have become the primary approach for revascularization, but these procedures heavily rely on advanced imaging techniques to ensure accuracy, and minimize patient and operator risk. Traditional methods like fluoroscopy, cine angiography, and digital subtraction angiography have long been standard, yet come with significant limitations in terms of radiation exposure, contrast use, and procedural efficiency. One of the most promising advancements in this field is roadmap imaging, a technique that integrates pre-acquired imaging with live fluoroscopy, enhancing precision while simultaneously minimizing the necessity of high-radiation modalities. Roadmap imaging capabilities are available on most advanced cardiac cath lab platforms from GE, Philips, and Siemens Healthineers.
Imaging Modalities in Peripheral Vascular Interventions
Imaging is vital in the management of PVD, guiding catheter navigation, balloon angioplasty, and stent placement. Common imaging techniques include:
1. Fluoroscopy: Provides continuous real-time X-ray imaging with the lowest radiation dose, but lacks the detailed visualization required for complex anatomy, especially in small-caliber vessels or heavily calcified arteries.
2. Cine Angiography: Generates high- quality dynamic imaging over time, offering a more detailed view of arterial anatomy and hemodynamics, but at a cost of a significantly higher radiation dose (at least four to five times that of fluoroscopy1; when fluoro save is used, cine angiography dose can be 10–50 times higher2,3).
3. Digital Subtraction Angiography (DSA): The gold standard for angiographic imaging, particularly in the assessment of complex vascular anatomy. However, DSA requires multiple contrast injections, and exposes both patients and operators to substantial radiation, with about a 30-fold increase in radiation dose to the operating physician compared to low-dose fluoroscopy in some systems and procedures4 (when fluoro save is used, dose can be up to 100 times higher3).
The development of roadmap imaging has further refined the guidance of endovascular interventions. By generating a real-time, detailed overlay of vascular anatomy aligned to live fluoroscopy, roadmap imaging enables more precise and accurate navigation during these procedures, thereby reducing the risk of complications as well as improving patient outcomes.
Roadmap Imaging: Mechanism and Benefits
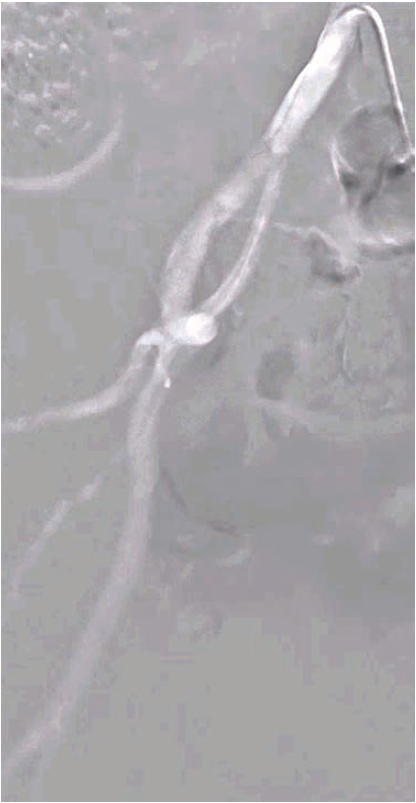
Roadmap imaging represents a sophisticated blend of pre-acquired images (often from computed tomography [CT] angiography or DSA) with real-time fluoroscopy, providing a continuous overlay that allows for precise guidance throughout the procedure. The technology works by creating a “virtual road” overlaid onto live fluoroscopic images, facilitating catheter and device navigation.
Key Advantages
1. Enhanced Precision in Complex Anatomy: The ability to superimpose pre-acquired images over real-time fluoroscopy improves the visualization of vessel course, tortuosity, and calcifications, essential for navigating complex below-knee vessels.
2. Reduced Radiation Exposure: By minimizing the need for repeated contrast injections, cine, and DSA, roadmap imaging significantly reduces the radiation dose to both the patient and the operator. This is especially critical in long, intricate procedures where radiation burden can accumulate rapidly.
3. Minimized Contrast Use: In traditional imaging, repeated contrast injections are required to guide catheter, wire, and device movement, which not only increases the risk of contrast-induced nephropathy but also elevates radiation exposure. Roadmap imaging eliminates the need for continuous contrast injections, enhancing patient safety.
4. Real-Time Guidance: The fusion of live fluoroscopy with static images allows for immediate, real-time adjustments in catheter and wire placement, improving procedural outcomes and efficiency. This is particularly beneficial in below-knee interventions, where vessel access and navigation can be particularly challenging due to tortuosity, small vessel calibers, and collateral circulation.

5. Improved Procedural Efficiency: With the ability to precisely navigate complex vascular paths, roadmap imaging reduces the time spent searching for and confirming the target vessels, thus decreasing overall procedure time and improving the likelihood of successful revascularization.
Clinical Impact in Below-Knee Interventions
Below-knee interventions are among the most challenging in endovascular procedures. The small vessel size, presence of extensive calcification, and complex collateral network make navigation difficult, especially in patients with chronic total occlusions (CTOs). Roadmap imaging provides several distinct benefits in the following situations:

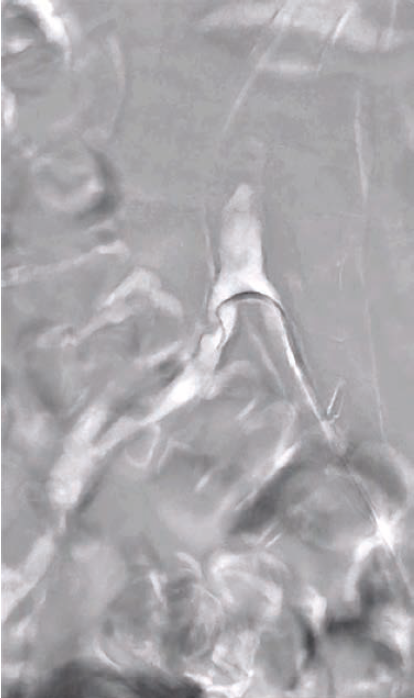
1. Tortuosity and Calcifications: Roadmap imaging allows for accurate identification and navigation around tortuous or calcified segments, which is crucial for reducing the risk of procedural failure or complications, such as arterial perforation or dissection.
2.Subintimal Access: In cases where intraluminal access is not possible, roadmap imaging can help guide operators into the subintimal space, increasing the chances of successful crossing in CTOs.
3. Improved Limb Salvage Rates: Successful revascularization of below-knee vessels, particularly in the setting of CLTI, is paramount for limb salvage. Roadmap imaging contributes to higher technical success rates by optimizing navigation, reducing radiation, and minimizing contrast use, improving clinical outcomes for these high-risk patients.
Challenges and Limitations
Despite its benefits, roadmap imaging entails certain limitations, including:
1. Misregistration: A potential drawback of roadmap imaging is the risk of misregistration, where the pre-acquired image does not align perfectly with the real-time fluoroscopic view. This misalignment can be caused by patient movement, arterial pulsations, or changes in the position of the catheter during the procedure. In below-knee interventions, where the vessels are distal and farther from the heart, such movements are generally less of a concern, but they can still affect image accuracy.
2. Patient Sedation: In complex procedures like those involving below-knee vessels, patients are often moderately sedated. This sedation helps to limit motion, but excessive movement or respiratory artifacts can still challenge the accuracy of roadmap imaging.
3. Technology Availability and Cost: While roadmap imaging is a powerful tool, its availability is restricted to certain advanced imaging platforms, and it can incur higher costs in both equipment and operator training. This may limit access to the technology in certain healthcare settings or regions.
4. Learning Curve: Properly utilizing roadmap imaging requires specialized training and experience. Misuse or lack of familiarity can lead to suboptimal results, making operator proficiency a critical factor in its success.
Conclusion
Roadmap imaging represents a groundbreaking advancement in endovascular interventions, particularly for complex cases of peripheral vascular disease. By providing real-time, high-precision navigation of vascular structures while minimizing radiation and contrast exposure, roadmap technology offers significant clinical benefits. Its ability to enhance procedural accuracy and efficiency is invaluable in challenging cases, especially in below-knee interventions for CTOs and CLTI.
While there are challenges related to misregistration, technology availability, and the need for specialized training, the advantages of roadmap imaging in improving patient safety, clinical outcomes, and procedural success make it an indispensable tool in modern vascular procedures.
References
1. Olcay A, Guler E, Karaca IO, et al. Comparison of fluoro and cine coronary angiography: balancing acceptable outcomes with a reduction in radiation dose. J Invasive Cardiol. 2015 Apr;27(4):199-202. PMID: 25840403.
2. Kern MJ, Seto AH, Forsberg M. Vascular Access. In: Kern M, Sorajja P, Lim M, editors. The Interventional Cardiac Catheterization Handbook. Philadelphia: Elsevier; 2018:51-87.
3. Moscucci M. Grossman & Baim’s Cardiac Catheterization, Angiography, and Intervention. Philadelphia: Wolters Kluwer; 2015.
4. Gyánó M, Berczeli M, Csobay-Novák C, et al. Digital variance angiography allows about 70% decrease of DSA-related radiation exposure in lower limb X-ray angiography. Sci Rep. 2021 Nov 8;11(1):21790. doi:10.1038/s41598-021-01208-3
Bibliography
1. Hennessey B, Danenberg H, De Vroey F, et al. Dynamic Coronary Roadmap versus standard angiography for percutaneous coronary intervention: the randomised, multicentre DCR4Contrast trial. EuroIntervention. 2024 Feb 5; 20(3): e198-e206. doi:10.4244/EIJ-D-23-00460.
2. Posa A, Tanzilli A, Barbieri P, et al. Digital subtraction angiography (DSA) technical and diagnostic aspects in the study of lower limb arteries. Radiation. 2022; 2(4): 376-386. https://doi.org/10.3390/radiation2040028










