Cracking Calcium With the C2+ Lithotripsy Balloon
Can Greater Pulse Availability Translate to Enhanced Procedural Outcome Whilst Maintaining a High Safety Profile?
Can Greater Pulse Availability Translate to Enhanced Procedural Outcome Whilst Maintaining a High Safety Profile?
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Jonathan Hinton, MD1; Gao Ong, MD2; Mae Bethell, MD1; Jennifer Barraclough, MD3; Ganeev Malhotra, MD2; Thomas Johnson, MD3,4; Simon J. Wilson, MD2; James C. Spratt, BSc, MB ChB, MD2; Julian Strange, MD3; Peter O’Kane, MD1
1Dorset Heart Centre, Royal Bournemouth Hospital, Bournemouth
2Intervention and Coronary Artery Disease Group, St Georges University Hospital, London
3Bristol Heart Institute, University Hospital Bristol, Bristol
4University of Bristol, Bristol
United Kingdom
The authors can be contacted via Jonathan Hinton, MD, at jonathan.hinton@uhd.nhs.uk.
Coronary artery calcification is a common challenge in percutaneous coronary intervention (PCI), often leading to stent under-expansion and failure.1-5 Intravascular lithotripsy (IVL) has emerged as a safe and effective tool for calcium modification, with the DISRUPT CAD trials showing favorable outcomes even in complex lesions.6-10 IVL uses acoustic waves to fracture calcium and improve vessel compliance, and its balloon-based delivery system offers a short learning curve and ease of use compared to atherectomy.
While IVL has shown promise in a range of scenarios, including STEMI, eccentric lesions in combination with rotational atherectomy, and stent failure due to calcific under-expansion,12-20 limitations remain, such as balloon crossing profile and the pulse cap of the C2 balloon (80 pulses) (Shockwave Medical). Registry data suggest higher pulse counts may improve outcomes.21 This analysis evaluates patient and procedural characteristics, along with medium-term outcomes, from early experience with the C2+ IVL balloon (Shockwave Medical), which delivers up to 120 pulses.
Method
Study participants and data collection
This is a retrospective analysis of consecutive patients treated with IVL for coronary calcification using the C2+ Shockwave balloon from its implementation in November 2022 through December 2023, with comparison to consecutive patients in the preceding year undergoing C2 Shockwave balloon treatment, taking place across the three hospitals (University Hospital Dorset, University Hospital Bristol & Weston, and St. George’s University Hospital). This analysis received approval from each of the local audit/service evaluation groups. Baseline demographics, comorbidity details, and details of the procedure were taken from the British Cardiovascular Intervention Society database. Target vessel revascularization (TVR) and mortality during the analysis were also recorded.
Procedure
Patients were included in this cohort if the treating interventional cardiologist felt that there was significant calcification requiring modification with IVL. The size of IVL balloon and number of pulses delivered was at the discretion of the supervising interventional cardiologist. IVL was performed using the Shockwave C2 system as per the standard IVL technique using the C2 or C2+ balloon.22
Statistical analysis
Patient demographics and comorbidities are reported per patient, while procedural data are reported per procedure to account for patients who underwent more than one IVL procedure. Continuous variables are shown as medians with interquartile ranges (IQR), and compared between C2 and C2+ groups using the Mann-Whitney U test. Categorical variables are reported as counts and percentages, with group comparisons made using the Chi-squared test.
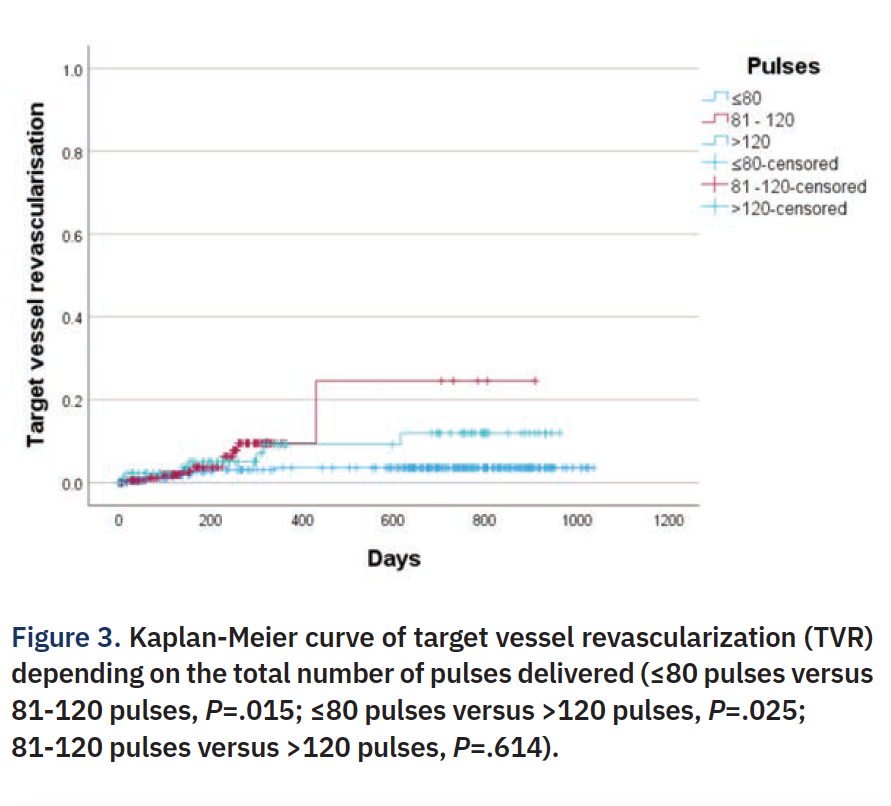
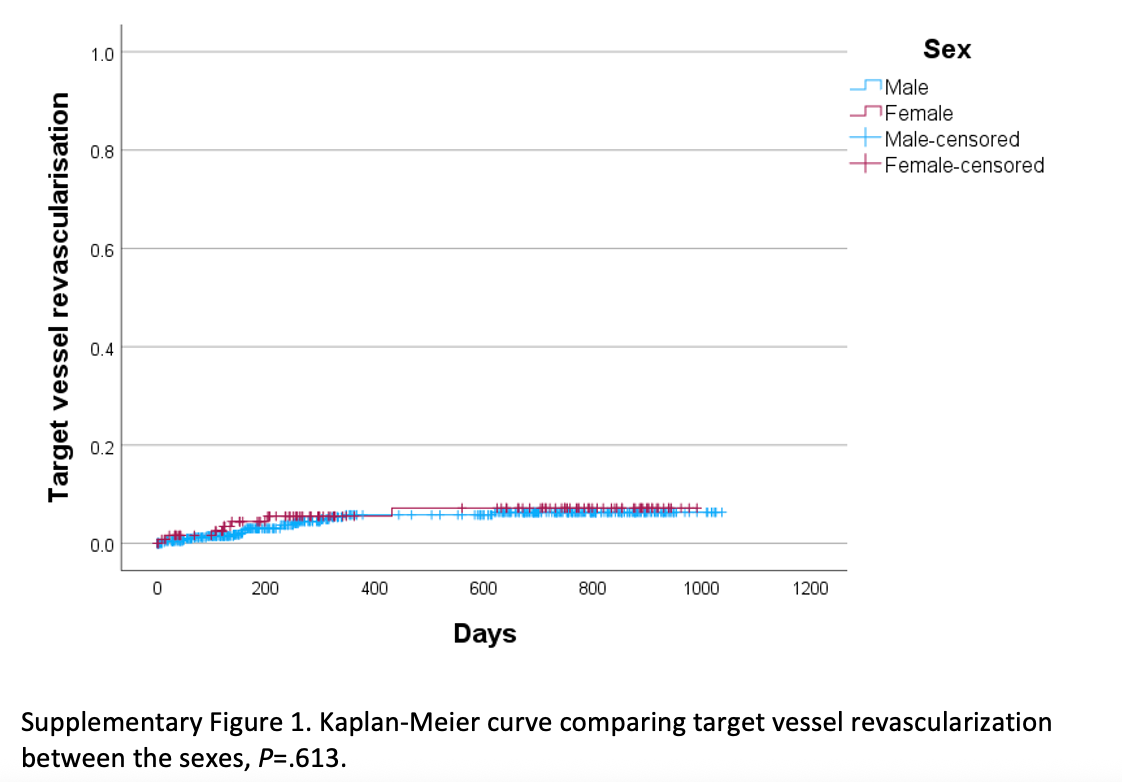
Target vessel revascularization (TVR) is presented per lesion, and mortality is presented per patient, both analyzed using Kaplan-Meier curves. Given prior data linking higher pulse counts with lower TVR, TVR was also analyzed per procedure by grouping total IVL pulses into ≤80 pulses, 81-120 pulses, and >120 pulses as categories. Additional TVR comparisons were made by sex and use of intracoronary imaging.
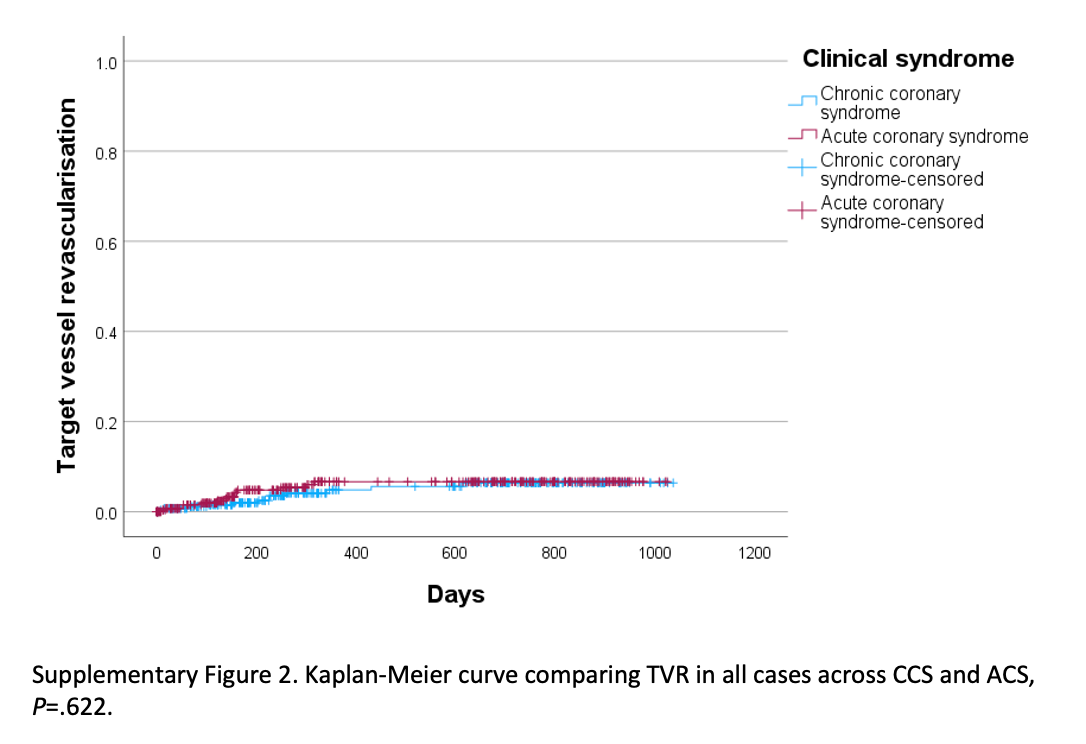
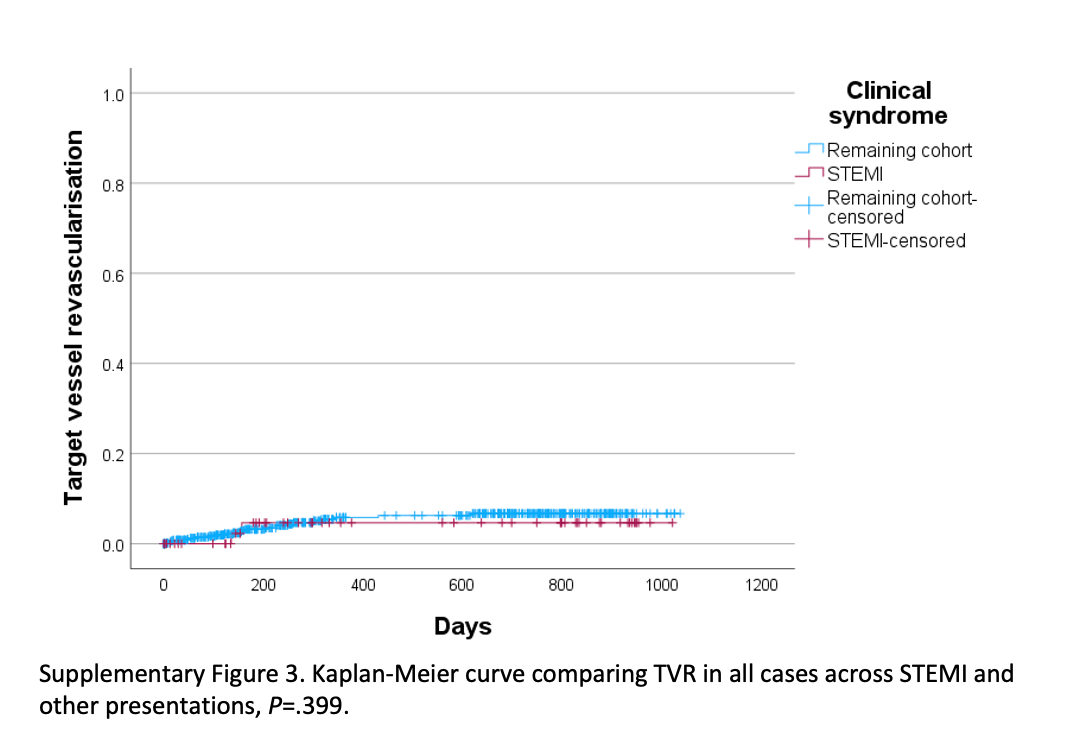
Kaplan-Meier analyses were also used to compare TVR in the entire cohort across several subgroups: acute coronary syndrome (ACS) versus chronic coronary syndrome (CCS, also known as stable ischemic heart disease), ST-elevation myocardial infarction (STEMI) versus non STEMI, IVL with versus without adjunctive atherectomy or cutting balloon, and treatment of in-stent restenosis versus de novo lesions. Log-rank tests were used for all group comparisons. Analyses were conducted using SPSS v29.0 (IBM Corp).
Results
Patients
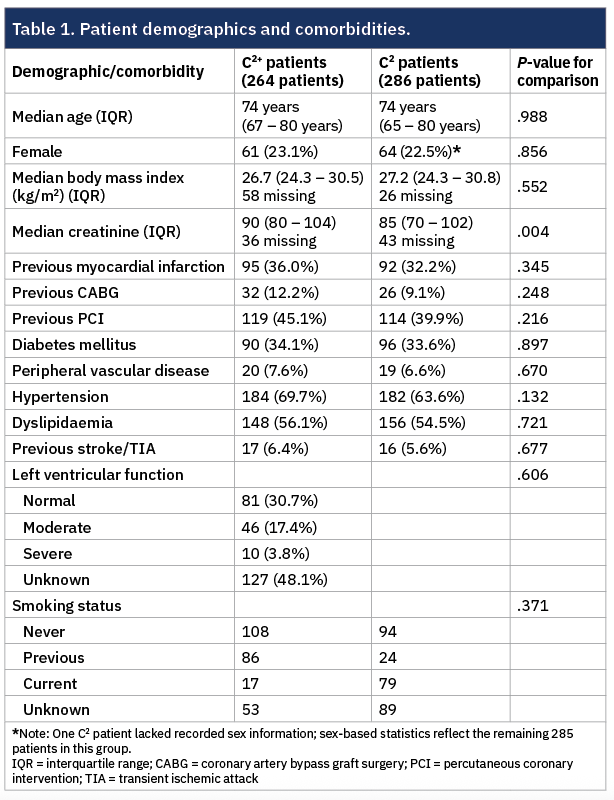
A total of 264 patients were treated with the C2+ IVL balloon, accounting for 274 procedures, while 286 patients received the C2 balloon in the preceding year, totaling 296 procedures. The median age of the overall cohort was 74 years (interquartile range [IQR] 65-80), and 22.7% were female. Baseline characteristics were generally well-matched between groups, with the only significant difference being a higher median creatinine level in the C2+ group (90 µmol/L versus 85 µmol/L, P=.004). Full demographic and comorbidity data are summarized in Table 1.
Presentation and procedures (Table 2)
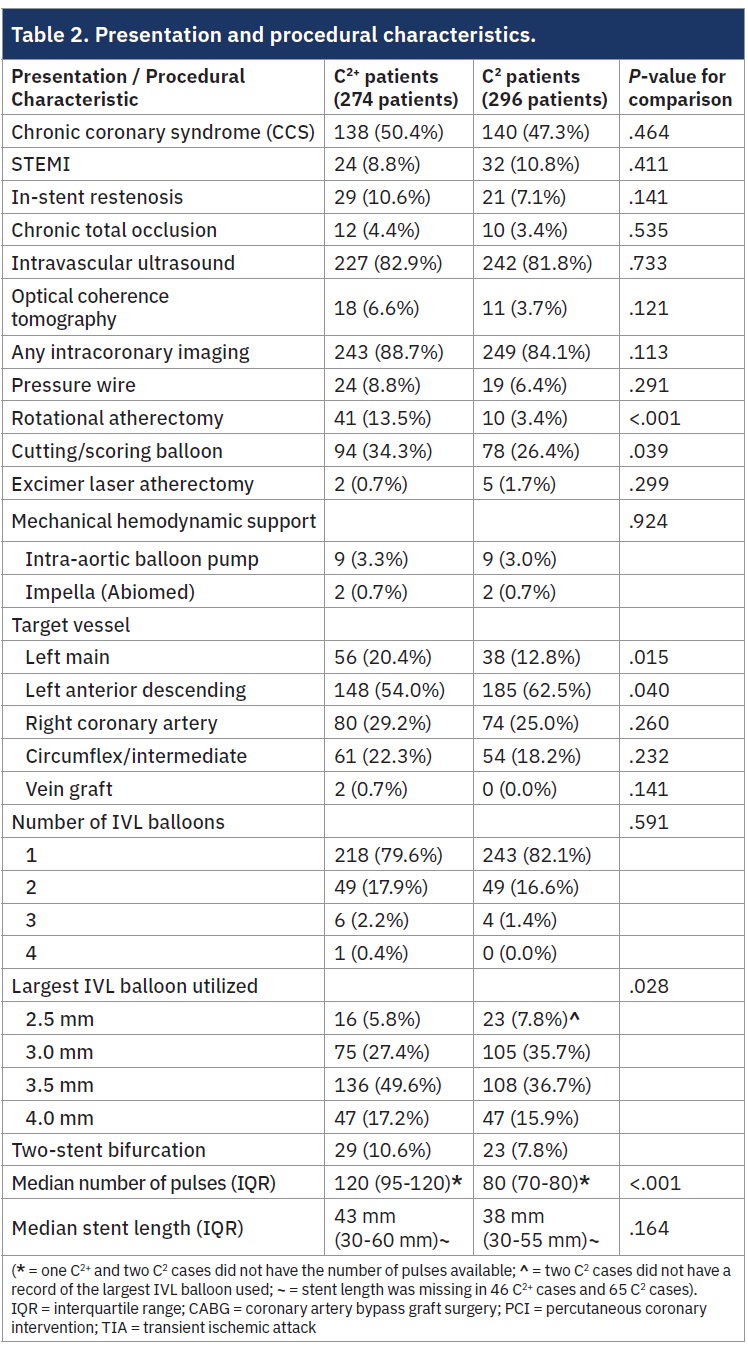
There was a balanced distribution of ACS and CCS presentations, with no significant difference between the C2 and C2+ cohorts. IVL was used in previously stented segments in 8.8% of cases, again with similar rates between groups. Left main PCI was more frequent in the C2+ cohort (20.4% versus 12.8%, P=.015), and use of adjunctive devices such as rotational atherectomy (13.5% versus 3.4%, P<.001) and cutting balloons (34.3% versus 26.4%, P=.039) was also higher in the C2+ group.
Intravascular imaging was widely used (86.3% overall), with no significant difference between groups. The C2+ cohort had significantly higher total IVL pulse counts than the C2 cohort (median 120 versus 80 pulses, P<.001), reflecting the C2+ balloon’s expanded capacity. Although most cases used a single IVL balloon, larger balloon sizes were more frequently used in the C2+ group. There was also a non-significant trend toward longer stent lengths in the C2+ cohort.
Procedural and follow-up outcomes
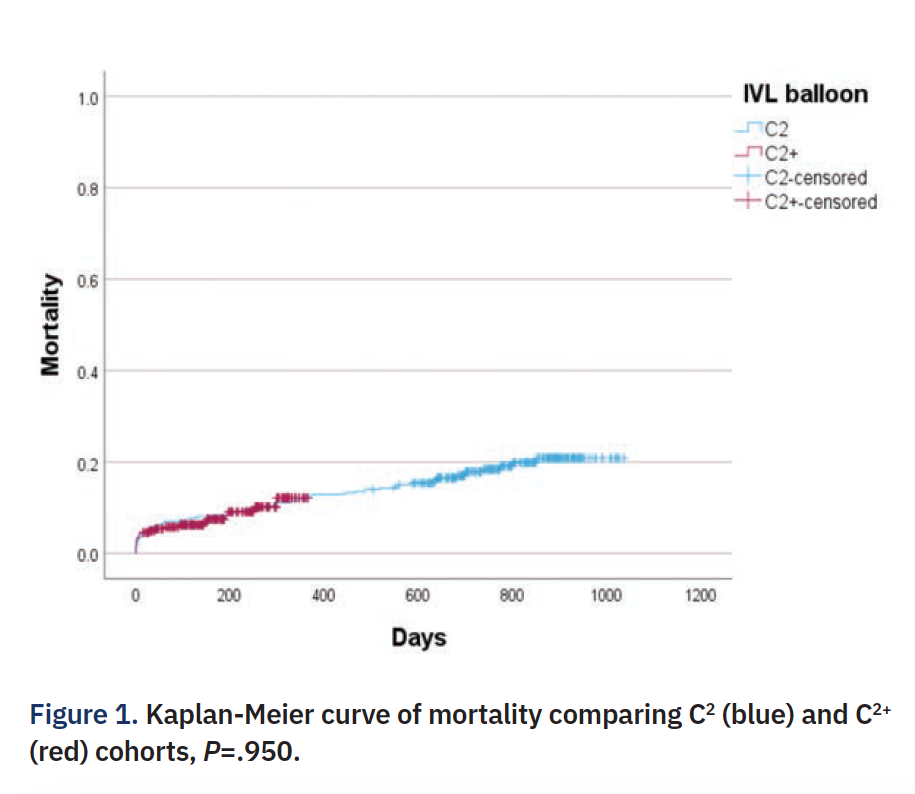
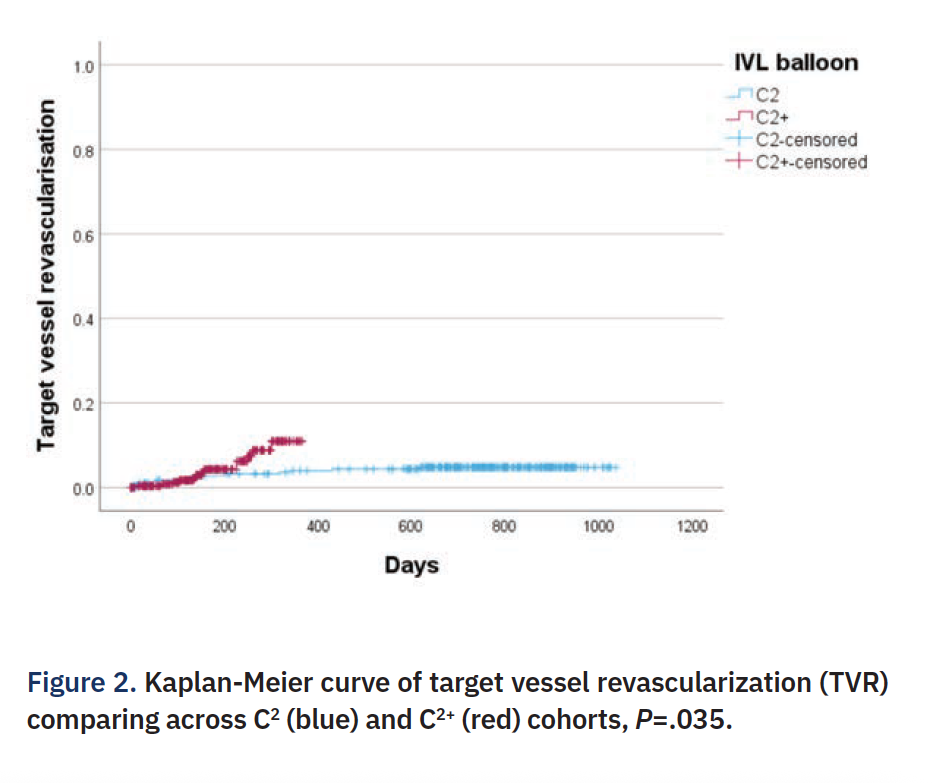
In terms of vessel perforation (as opposed to distal wire perforation), there were three (1.0%) perforations in the C2 cohort and three (1.1%) perforations in the C2+ cohort. In the entire cohort, at a median follow-up of 324 days, there were 76 deaths. Median follow-up in C2+ cohort was 172 days (IQR 101-264 days) and median follow up in C2 cohort was 752 days (IQR 643-859 days), with 54 deaths in C2 cohort and 22 deaths in the C2+ cohort. There was no difference in mortality between the C2 and C2+ cohorts on Kaplan-Meier curve and log rank analysis (Figure 1). There was a significant increase in the frequency of TVR with the use of the C2+ when comparing the C2 and C2+ cohorts, but the split in the curves occurred after around 200 days (Figure 2). When the two cohorts were combined, those patients with ≤80 pulses had significantly lower TVR when compared with those with 81-120 pulses and >120 pulses (Figure 3).
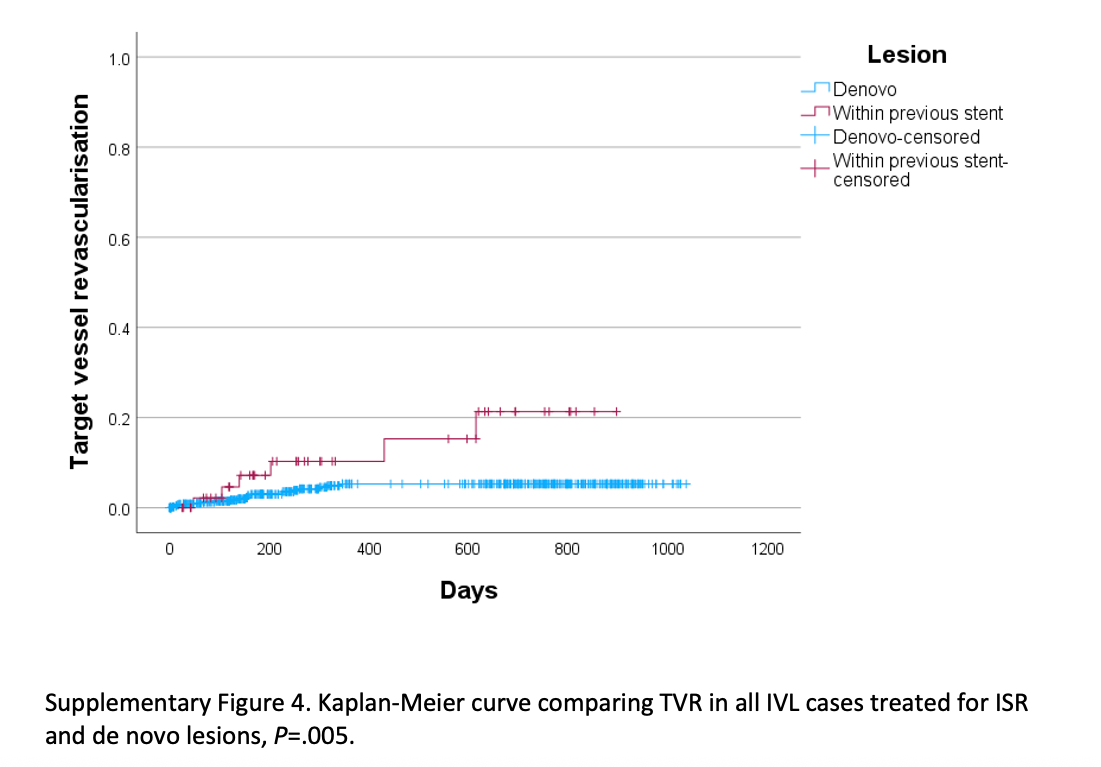
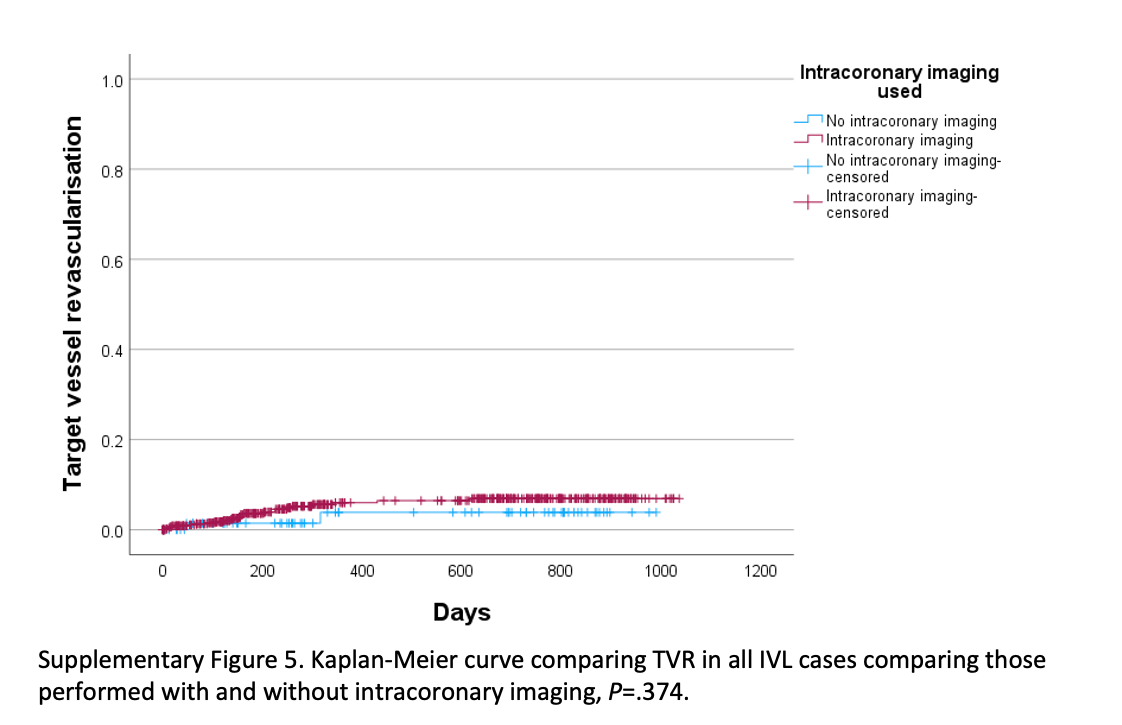
There was no difference in TVR between sexes (Supplementary Figure 1). There was no difference in TVR when ACS cases were compared with CCS cases (P=.622) and STEMI cases with the remainder of the cohort (Supplementary Figures 2-3) (P=.706). The TVR frequency was significantly higher in patients treated with IVL within a previously stented segment compared with de novo disease (Supplementary Figure 4) (P=.005). Finally, there was no difference in TVR in cases where IVL was used alone versus in conjunction with rotational/orbital atherectomy, cutting balloons, or intracoronary imaging (Supplementary Figure 5).
Discussion
This is the first analysis comparing the C2+ IVL balloon (120 pulses) with the standard C2 (80 pulses). Use of the C2+ was associated with more complex cases, including higher rates of left main PCI and adjunctive atherectomy, and a higher frequency of target vessel revascularization (TVR). This may reflect selection bias, as operators possibly used C2+ in more complex anatomy, supported by longer stent lengths and greater use of imaging. While both cohorts showed good acute outcomes, the difference in TVR became apparent beyond 200 days, and longer follow-up is warranted.
Compared with the DISRUPT CAD III and IV trials, which enrolled shorter, more focal lesions (≤40 mm),8-10 our study population presented with more complex disease, evident in the longer stents and broader use of adjunctive tools. Intriguingly, while the FRANCE-LILI registry showed reduced TVR with more pulses,21 our analysis showed the opposite. However, the widespread use of intracoronary imaging in our study likely led to higher pulse counts in more advanced disease, making pulse number a surrogate for lesion complexity rather than an independent predictor of outcome.
IVL showed favorable results in ACS and STEMI patients, with similar TVR rates compared to CCS cases. This is notable given the limited data on plaque modification in STEMI due to concerns around embolization with atherectomy.8,9,15,20,23 IVL may provide an accessible, safe alternative in this setting, especially for operators without atherectomy experience.
Despite more pulses with the C2+, operators used more adjunctive tools, suggesting evolving practice toward hybrid strategies such as “rotashock.” While promising, evidence supporting the added benefit of multimodality plaque modification, especially involving IVL, remains limited.24-27
We also observed frequent IVL use for stent under-expansion. Although this subgroup had higher TVR, as expected for restenosis cases, the one-year TVR rate (22.2%) was in line with other cohorts.12,18,20,28-31 These findings support the real-world safety and utility of IVL in previously stented segments.
Lastly, the perforation rate in this analysis was slightly higher (1.0% with C2 and 1.1% with C2+) compared with the Disrupt CAD III and IV trials, which reported perforation rates of 0.3% and 0.0%, respectively.8,9 This difference is likely attributable to the more complex lesions and use of larger balloons in our study, rather than any specific safety concern with the C2+ device.
Limitations
This analysis has several limitations. First, although data were collected from three sites, all were early adopters of the C2+ balloon with established calcium modification programs, limiting generalizability, especially in settings with low use of intracoronary imaging. Second, this was a retrospective analysis based on data from the British Cardiovascular Intervention Society database, which lacks formal adjudication. Additionally, TVR events may be underreported if patients sought care outside the contributing institutions. Lastly, the C2+ cohort had a median follow-up of only 172 days, reducing the power to assess medium-term outcomes compared to the C2 cohort.
Conclusion
The C2+ IVL balloon’s greater pulse availability has been shown to be as safe as the C2 IVL balloon and similarly, is suitable for a broad range of presentations and calcific lesion subsets. The use of the C2+ IVL balloon is associated with good clinical outcomes in a complex, real-world cohort of patients with severe calcification. However, from this retrospective analysis, efficacy does not appear to correlate with the number of pulses used at a lesion level.
References
1. Guedeney P, Claessen BE, Mehran R, Mintz GS, Liu M, Sorrentino S, et al. Coronary calcification and long-term outcomes according to drug-eluting stent generation. JACC Cardiovasc Interv. 2020; 13(12): 1417-1428. https://www.jacc.org/doi/10.1016/j.jcin.2020.03.053
2. Tada T, Miura K, Ikuta A, Ohya M, Shimada T, Osakada K, et al. Prevalence, predictors, and outcomes of in-stent restenosis with calcified nodules. EuroIntervention. 2022; 17(16): 1352-1361. https://eurointervention.pcronline.com/article/prevalence-predictors-and-outcomes-of-in-stent-restenosis-with-calcified-nodules
3. Choi SY, Maehara A, Cristea E, Witzenbichler B, Guagliumi G, Brodie B, et al. Usefulness of minimum stent cross sectional area as a predictor of angiographic restenosis after primary percutaneous coronary intervention in acute myocardial infarction (from the HORIZONS-AMI Trial IVUS substudy). Am J Cardiol. 2012; 109(4): 455-460. https://www.sciencedirect.com/science/article/abs/pii/S0002914911030323
4. Kawashima H, Serruys PW, Hara H, Ono M, Gao C, Wang R, et al. 10-Year all-cause mortality following percutaneous or surgical revascularization in patients with heavy calcification. JACC Cardiovasc Interv. 2022; 15(2): 193-204. https://www.jacc.org/doi/10.1016/j.jcin.2021.10.026
5. Copeland-Halperin RS, Baber U, Aquino M, Rajamanickam A, Roy S, Hasan C, et al. Prevalence, correlates, and impact of coronary calcification on adverse events following PCI with newer-generation DES: Findings from a large multiethnic registry. Catheter Cardiovasc Interv. 2018; 91(5): 859-866. https://onlinelibrary.wiley.com/doi/10.1002/ccd.27204
6. Brinton TJ, Ali ZA, Hill JM, Meredith IT, Maehara A, Illindala U, et al. Feasibility of Shockwave coronary intravascular lithotripsy for the treatment of calcified coronary stenoses. Circulation. 2019; 139(6): 834-836. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.118.036531
7. Ali ZA, Nef H, Escaned J, Werner N, Banning AP, Hill JM, et al. Safety and effectiveness of coronary intravascular lithotripsy for treatment of severely calcified coronary stenoses: The Disrupt CAD II Study. Circ Cardiovasc Interv. 2019; 12(10): e008434. https://www.ahajournals.org/doi/10.1161/CIRCINTERVENTIONS.119.008434
8. Hill JM, Kereiakes DJ, Shlofmitz RA, Klein AJ, Riley RF, Price MJ, et al. Intravascular lithotripsy for treatment of severely calcified coronary artery disease. J Am Coll Cardiol. 2020; 76(22): 2635-2646. https://www.jacc.org/doi/10.1016/j.jacc.2020.09.603
9. Saito S, Yamazaki S, Takahashi A, Namiki A, Kawasaki T, Otsuji S, et al. Intravascular lithotripsy for vessel preparation in severely calcified coronary arteries prior to stent placement: Primary outcomes from the Japanese Disrupt CAD IV Study. Circ J. 2021; 85(6): 826-833. https://www.jstage.jst.go.jp/article/circj/85/6/85_CJ-20-1174/_article
10. Saito S, Yamazaki S, Takahashi A, Namiki A, Kawasaki T, Otsuji S, et al. Intravascular lithotripsy for vessel preparation in calcified coronary arteries prior to stent placement: Japanese Disrupt CAD IV Study 1-year results. Circ Rep. 2022; 4(9): 399-404. https://www.jstage.jst.go.jp/article/circrep/4/9/4_CR-22-0068/_article
11. McInerney A, Travieso A, Cubero H, Jerónimo-Baza A, Jimenez-Quevedo P, Tirado-Conte G, et al. Mid-term angiographic and intracoronary imaging results following intracoronary lithotripsy in calcified coronary artery disease: Results from two tertiary referral centres. Cardiovasc Revasc Med. 2023; 52: 59-66. https://www.sciencedirect.com/science/article/abs/pii/S1553838923000726
12. Hinton J, Mariathas M, Chan E, Patel A, Singh S, Konstantinou K, et al. Novel application of intravascular lithotripsy in stent under-expansion: A single-center experience. Catheter Cardiovasc Interv. 2023 Feb; 101(2): 243-249. https://onlinelibrary.wiley.com/doi/abs/10.1002/ccd.30516
13. Ali ZA, Kereiakes DJ, Hill JM, Saito S, Di Mario C, Honton B, et al. Impact of calcium eccentricity on the safety and effectiveness of coronary intravascular lithotripsy: Pooled analysis from the Disrupt CAD studies. Circ Cardiovasc Interv. 2023; 16(10): e012898. https://www.ahajournals.org/doi/10.1161/CIRCINTERVENTIONS.123.012898
14. Honton B, Lipiecki J, Monségu J, Leroy F, Benamer H, Commeau P, et al. Mid-term outcome of de novo lesions vs. in-stent restenosis treated by intravascular lithotripsy procedures: Insights from the French Shock Initiative. Int J Cardiol. 2022; 365: 106-111. https://www.sciencedirect.com/science/article/abs/pii/S0167527322010919
15. Cosgrove C, Hanratty CG, Hill JM, Mahadevan K, Mailey J, McEntegart M, et al. Intravascular lithotripsy for treatment of calcific coronary lesions in ST elevation myocardial infarction. Catheter Cardiovasc Interv. 2022; 99(2): 322-328. https://openaccess.sgul.ac.uk/id/eprint/113302/1/ccd.29801.pdf
16. Cubero-Gallego H, Gonzalo N, Tizon-Marcos H, Salvatella N, Garcia-Guimaraes M, Negrete A, et al. Primary angioplasty of calcified coronary lesions using coronary lithotripsy in acute ST-segment elevation myocardial infarction. J Invasive Cardiol. 2021; 33(12): E970-E973. https://www.hmpgloballearningnetwork.com/site/jic/brief-communication/primary-angioplasty-calcified-coronary-lesions-using-coronary
17. Cubero-Gallego H, Calvo-Fernandez A, Tizon-Marcos H, Aparisi A, Gomez-Lara J, Amat-Santos I, et al. Real-world multicenter coronary lithotripsy registry: Long-term clinical follow-up. J Invasive Cardiol. 2022; 34(10): E701-E708. https://europepmc.org/article/med/36075883
18. Yeoh J, Cottens D, Cosgrove C, Mallek K, Strange J, Anderson R, et al. Management of stent underexpansion using intravascular lithotripsy—Defining the utility of a novel device. Catheter Cardiovasc Interv. 2021; 97(1): 22-29. https://onlinelibrary.wiley.com/doi/abs/10.1002/ccd.28715
19. Cosgrove CS, Wilson SJ, Bogle R, Hanratty CG, Williams R, Walsh SJ, et al. Intravascular lithotripsy for lesion preparation in patients with calcific distal left main disease. EuroIntervention. 2020; 16(1): 76-79. https://eurointervention.pcronline.com/article/intravascular-lithotripsy-for-the-treatment-of-calcific-distal-left-main-disease
20. Rodriguez-Leor O, Cid-Alvarez AB, Lopez-Benito M, Gonzalo N, Vilalta V, Diarte de Miguel JA, et al. A prospective, multicenter, real-world registry of coronary lithotripsy in calcified coronary arteries: The REPLICA-EPIC18 Study. JACC Cardiovasc Interv. 2024; 17(6): 756-767. https://www.jacc.org/doi/10.1016/j.jcin.2023.12.018
21. Honton B. French National FRANCE LILI registry on all comers’ patients treated by IVL. PCR online: Europa Group; 2023. https://media.pcronline.com/diapos/EuroPCR2024/116-20240516_1236_Room_241_Honton_Benjamin_1111100_(10531)/Honton_Benjamin_20240516_1215_Room_241.pdf
22. Daemen J, Forero MNT. The coronary intravascular lithotripsy system. Interv Cardiol. 2019; 14(3): 174-181. https://www.icrjournal.com/articles/coronary-intravascular-lithotripsy-system
23. Généreux P, Madhavan MV, Mintz GS, Maehara A, Palmerini T, Lasalle L, et al. Ischemic outcomes after coronary intervention of calcified vessels in acute coronary syndromes: Pooled analysis from the HORIZONS-AMI and ACUITY Trials. J Am Coll Cardiol. 2014; 63(18): 1845-1854. https://www.jacc.org/doi/10.1016/j.jacc.2014.01.034
24. Sharma SK, Mehran R, Vogel B, Hooda A, Sartori S, Hanstein R, et al. Rotational atherectomy combined with cutting balloon to optimise stent expansion in calcified lesions: The ROTA-CUT randomised trial. EuroIntervention. 2024; 20(1): 75-84. https://eurointervention.pcronline.com/article/rotational-atherectomy-with-cutting-balloon-to-optimize-stent-expansion-in-calcified-lesions-the-rotacut-randomized-trial
25. Furuichi S, Tobaru T, Asano R, Watanabe Y, Takamisawa I, Seki A, et al. Rotational atherectomy followed by cutting-balloon plaque modification for drug-eluting stent implantation in calcified coronary lesions. J Invasive Cardiol. 2012 May;24(5):191-195. https://www.hmpgloballearningnetwork.com/site/jic/articles/rotational-atherectomy-followed-cutting-balloon-plaque-modification-drug-eluting-stent--impl
26. Allali A, Toelg R, Abdel-Wahab M, Hemetsberger R, Kastrati A, Mankerious N, et al. Combined rotational atherectomy and cutting balloon angioplasty prior to drug-eluting stent implantation in severely calcified coronary lesions: The PREPARE-CALC-COMBO study. Catheter Cardiovasc Interv. 2022; 100(6): 979-989. https://onlinelibrary.wiley.com/doi/full/10.1002/ccd.30423
27. Li Q, He Y, Chen L, Chen M. Intensive plaque modification with rotational atherectomy and cutting balloon before drug-eluting stent implantation for patients with severely calcified coronary lesions: A pilot clinical study. BMC Cardiovasc Disord. 2016; 16: 112. https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-016-0273-8
28. Coughlan JJ, Aytekin A, Lahu S, Scalamogna M, Wiebe J, Pinieck S, et al. Derivation and validation of the ISAR score to predict the risk of repeat percutaneous coronary intervention for recurrent drug-eluting stent restenosis. EuroIntervention. 2023; 18(16): e1328-e1338. https://eurointervention.pcronline.com/article/derivation-and-validation-of-the-isar-score-to-predict-the-risk-of-repeat-percutaneous-coronary-intervention-for-recurrent-drug-eluting-stent-restenosis
29. Tovar Forero MN, Sardella G, Salvi N, Cortese B, di Palma G, Werner N, et al. Coronary lithotripsy for the treatment of underexpanded stents: The international multicentre CRUNCH registry. EuroIntervention. 2022 Sep 20; 18(7): 574-581. https://eurointervention.pcronline.com/article/coronary-lithotripsy-for-the-treatment-of-underexpanded-stents-the-international-multicentre-crunch-registry
30. Ielasi A, Moscarella E, Testa L, Gioffrè G, Morabito G, Cortese B, et al. Intravascular lithotripsy for the management of undilatable coronary stent: The SMILE Registry. Cardiovasc Revasc Med. 2020; 21(12): 1555-1559. https://www.sciencedirect.com/science/article/abs/pii/S155383892030292X?via%3Dihub
31. Wańha W, Tomaniak M, Wańczura P, Bil J, Januszek R, Wolny R, et al. Intravascular lithotripsy for the treatment of stent underexpansion: The multicenter IVL-DRAGON Registry. J Clin Med. 2022; 11(7): 1779. https://www.jacc.org/doi/10.1016/S0735-1097%2822%2901594-7










