Advancing the Cardiac Cath Lab: Strategic Implementation of a National Novel Core Curriculum Didactic Education with Orientation and Competency Standards for Nurses
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Sarah Davis-Arnold, MSN, RN, RCIS, EBP-C, NPD-C1; Jennifer Ballard-Hernandez, DNP, NP, FACC, FAHA, FAANP2; Cher Hagaman, MSN, GNP-BC, CCNS, CCRN, AACC3; Jessica Mullenix, MSN, AGPCNP, CEPS, CCK, FHRS4; Nicole Lewis, MSN, RN5
1Clinical Quality Program Specialist, National Clinical Nurse Advisor, Cardiology, San Francisco, California; 2Cardiology Nurse Practitioner, VA Long Beach Healthcare System, Long Beach, California; 3Heart Failure Nurse Practitioner, VA Long Beach Healthcare System, Long Beach, California; 4Electrophysiology Nurse Practitioner, Durham VA Medical Center, Durham, North Carolina; 5National Cardiology Nurse Manager, LTC Charles S. Kettles VA Medical Center, Ann Arbor, Michigan
The authors can be contacted via Sarah Davis-Arnold, MSN, RN, RCIS, EBP-C, NPD-C, at sdavisarnold@gmail.com.
Abstract
In response to increasing complexity in cardiovascular care and the urgent need for standardized, competency-based training, the authors developed and implemented the Cardiac Catheterization Lab Nursing Orientation and Core Competencies Guidebook. This initiative introduced a novel national curriculum designed to elevate the practice of cardiac catheterization lab (CCL) nursing through structured education, interprofessional collaboration, and evidence-based competency standards. Grounded in adult learning theory and experiential learning models, the curriculum comprises of 25 one-hour didactic course modules tailored to nurses and interprofessional staff transitioning into or advancing within CCL roles.
The curriculum was developed by a multidisciplinary panel of subject matter experts across cardiology and nursing, ensuring representation of diverse clinical expertise and practice settings. Evaluation data from more than 25 course modules demonstrated high learner satisfaction (average rating ≥4.02/5.0), self-reported knowledge gains, and increased confidence among participants. Learners consistently rated the material as relevant, well-structured, and conducive to practical application. These findings were complemented by qualitative feedback emphasizing the curriculum’s accessibility and clinical impact.
The Guidebook further defines 12 domains of nursing core competencies specific to CCL practice. It integrates critical concept competency statements that standardize expectations across facilities while allowing for site-specific adaptation through the addition of unit or facility-specific competencies. This dual framework ensures foundational competence in high-risk, high-acuity settings, supports consistent onboarding, and promotes a culture of continuous professional development. The initiative not only enhances individual clinical performance but also strengthens interdisciplinary collaboration, patient safety, and workforce resilience in cardiac procedural care.
List of Figures and Tables Below
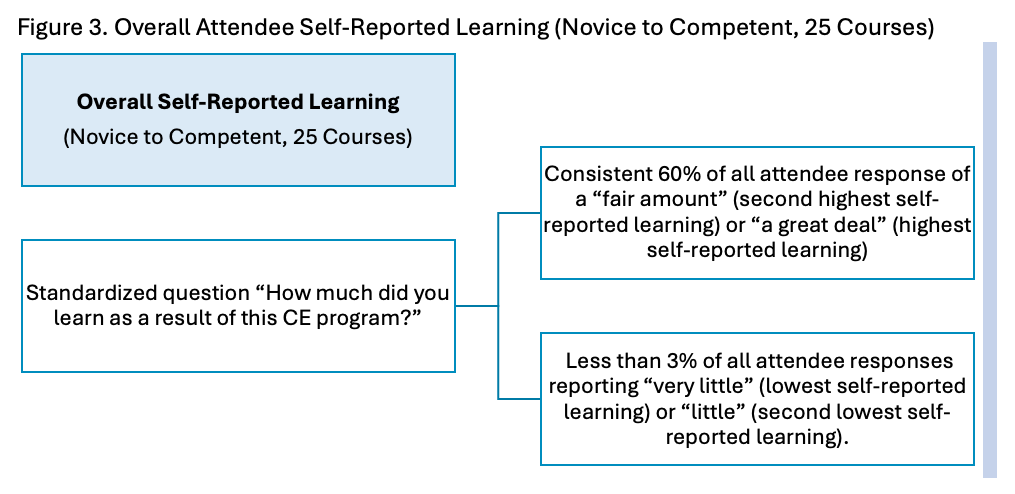
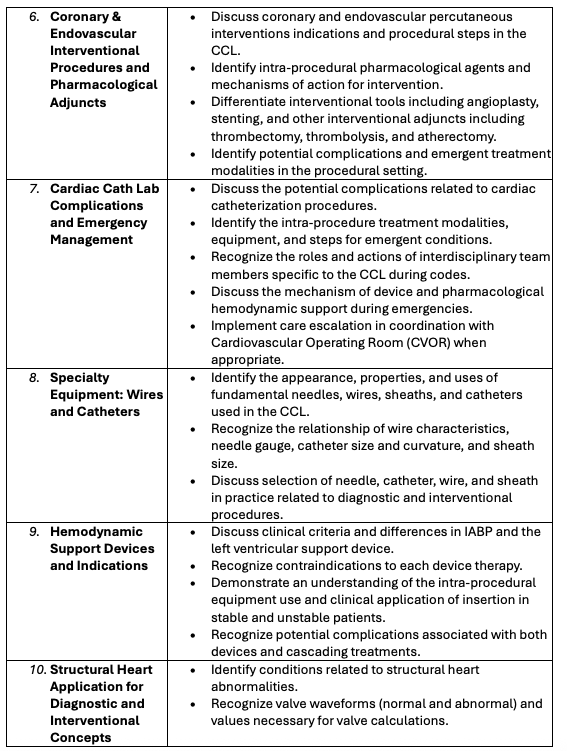
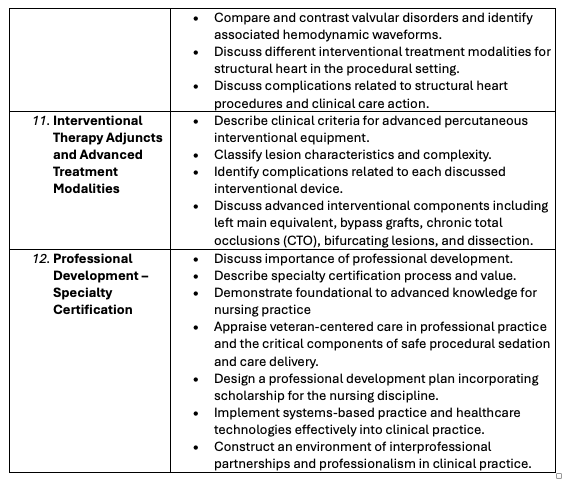
- Novice to Competent CCL Core Curriculum Didactic Courses: Table 1. Outlined courses implemented article.
- Competent to Expert CCL Core Curriculum Didactic Courses: Table 2. Outlined courses for future implementation.
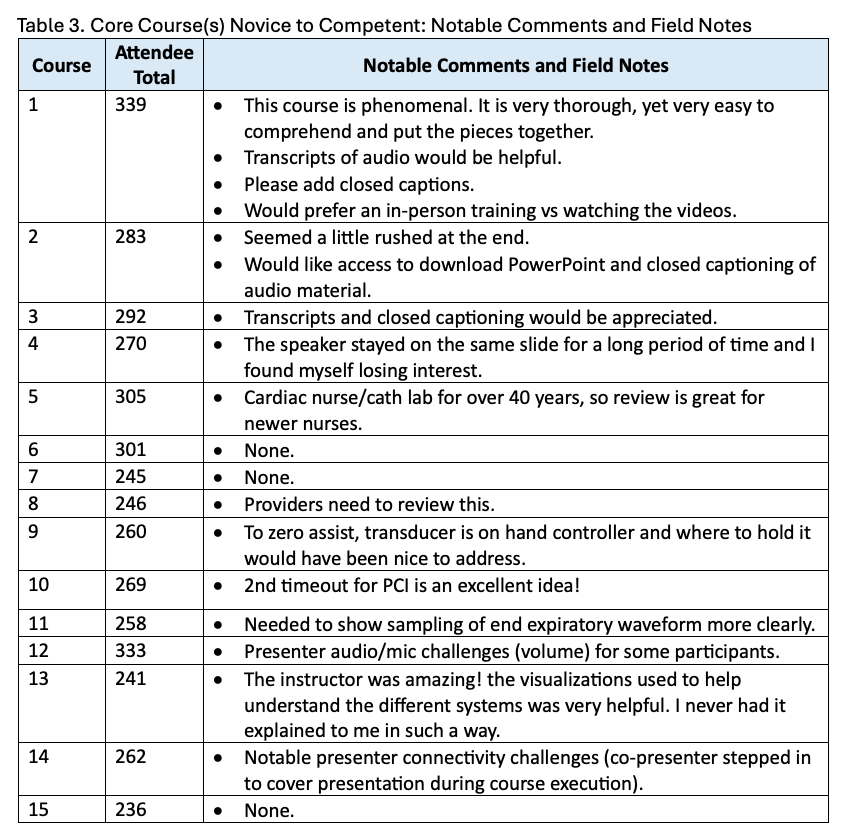
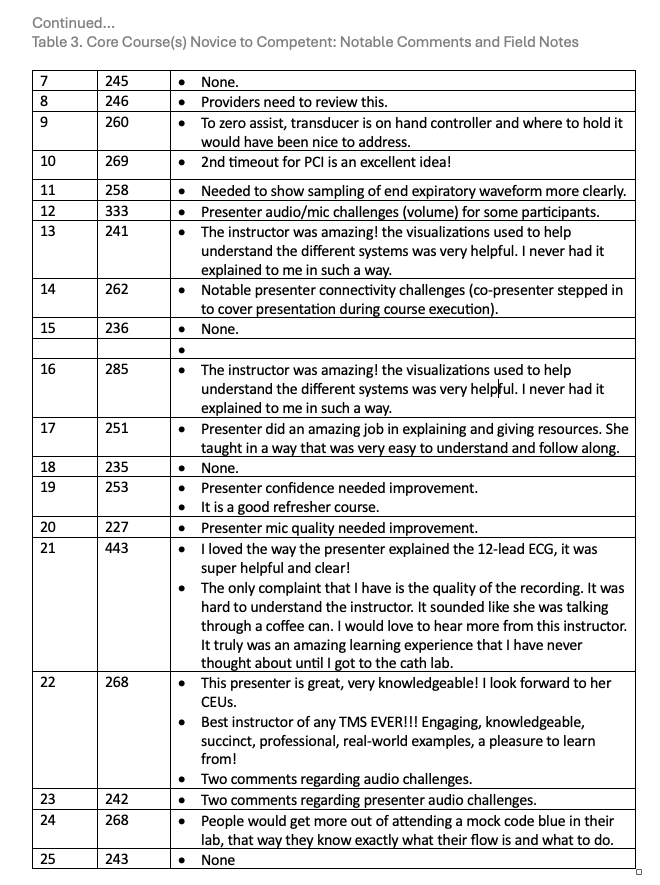
- Core Course(s) Novice to Competent, Notable Comments and Field Notes: Table 3. Notable comments and field notes from each course.
- Core Competencies for Cardiac Catheterization Lab Nursing: Table 4. CCL Core Competencies are used to fortify the basic knowledge and skills required for a nurse professional to be a safe and effective member in the CCL environment. These critical concept competencies require the equipment and facility/unit specific competency development
- LIVE Course Structure Example: Figure 1.
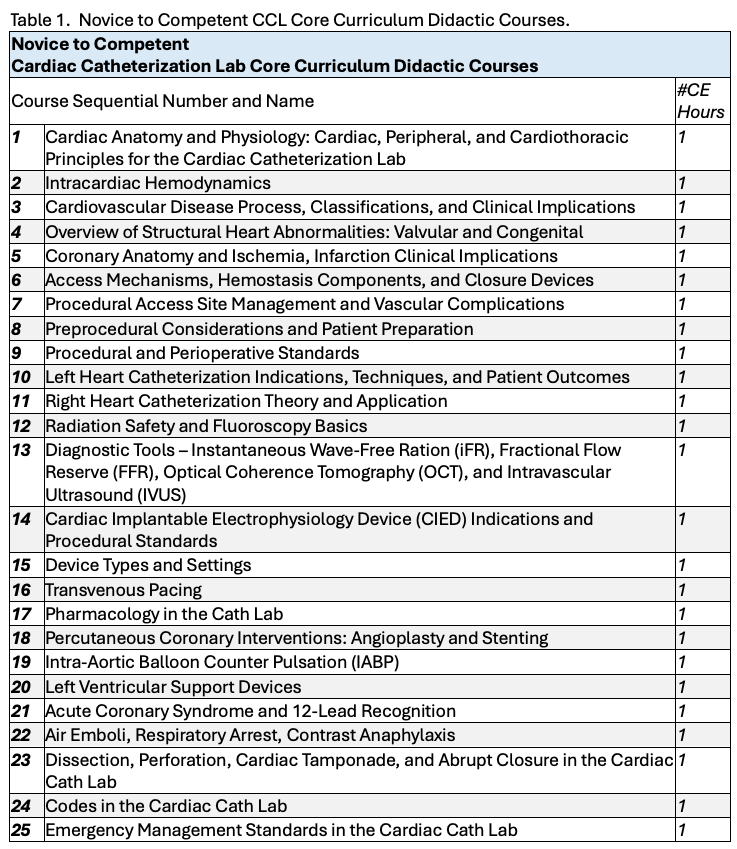
- Standardized Learner Satisfaction Statements (Novice to Competent, 25 Courses): Figure 2.
- Overall Attendee Self-Reported Learning, (Novice to Competent, 25 Courses): Figure 3.
Introduction
Amid the constantly evolving healthcare landscape, the role of cardiac catheterization labs (CCLs) in diagnosing and treating cardiovascular diseases has become increasingly dynamic and complex. Within these high-stake environments, the competence and expertise of CCL nurses and interprofessional staff are indispensable factors in ensuring optimal patient outcomes through high-quality, safe nursing care.1-5 Recognizing the critical importance of effective orientation and competency programs, we embarked on a 2022 journey to redefine and elevate the standards of CCL nursing education. This discussion serves as guidance for the path forward — an illustration of the dedication and innovation driving the evolution of CCL nursing practice through the novel Veterans Health Administration (VHA) Cardiac Catheterization Lab Nursing Orientation and Core Competencies Guidebook.
We delve into the depths of a groundbreaking initiative: the development and implementation of a novel Cardiac Cath Lab Core Curriculum for Orientation and Competency Standards tailored specifically for CCL nurses and interprofessional partners. By highlighting the core concepts, actionable strategies, and lessons learned through the operationalization of this curriculum, we aim to empower CCL leaders with the knowledge and insights necessary to nurture excellence in CCL through training, education and competency standards. Through collaboration, evidence-based practices, and a relentless commitment to quality, the core curriculum didactic and guidebook for orientation and competency standards presented herein represents a transformative force in healthcare education.
Background
Traditionally, the transition into a CCL nursing role has presented significant challenges for both new and experienced nurses. Without proper orientation and ongoing competency development, nurses may struggle to meet the demands of their roles, jeopardizing patient safety and quality of care. The Veterans Health Administration (VHA) is comprised of 170 medical centers that serve 9.1 million veterans.6 The current-state organizational analysis revealed an opportunity to strengthen standardized practice and support clinicians. Supporting indications included non-existent specialty standards for competency and orientation for CCL nursing professionals, and inconsistent expectations for both the private and federal sectors concerning nursing education, training, and competence.
The absence of a standardized training curriculum for CCL registered nurses has resulted in significant variability in training, knowledge, and expertise across healthcare settings. Without a unified framework, nurses entering this specialized field receive inconsistent education and hands-on experience, leading to disparities in the quality of patient care. Furthermore, the lack of a professional society dedicated to advocating for CCL nurses exacerbates the issue, leaving them without a unified voice to support their professional development, establish best practices, and address industry-wide challenges.
Within the field of educational theory, the recognition of adult learning theory, transition programs, higher reliability principles, and experiential learning all illustrate how this need is even more imperative, and highlight the increasing importance of addressing the orientation training and competency standardization needs.7-10 These components are required to guide an orientation that will protect and sustain safety, efficiency, and quality for patient outcomes, operational efficacy, and staffing stability in the CCL. These same concepts possess a noteworthy applicability to the practice of interventional procedures.
With increasingly higher patient acuity, case and program complexity, and operational cost, the discussion of why and how to orient individual team members to the CCL is more critical than ever. The 2020 pandemic exposed a delicate and quickly changing staffing ecosystem with experience-complexity gaps related to retirement, stress and burnout, and reallocation of nursing talent due to travel oriented fiscal advancement.11,12 Targeting actionable strategies, we leveraged these components to execute a tangible national strategy to support the largest healthcare system’s delivery of cardiovascular procedural care.13
Methods
Continuing education (CE) is essential for sustaining clinical excellence and reducing complications.14,15 Within the organization, we implemented a structured CE curriculum across 25 education modules that were 1 hour in duration to address “novice to competent” learning with core competencies, evaluated learner outcomes, and identified implications for practice and policy.
The core curriculum development workgroup consisted of a diverse group of subject matter experts in cardiology, selected by the National Field Advisory Committee for Cardiology with the Office of Nursing Service. The group included a dual-certified nursing professional development specialist, CCL experts, and cardiovascular nurse practitioners (NPs) with expertise in acute coronary syndromes, adult congenital heart disease, and heart failure, and CCL nursing leaders. The faculty had a wide range of expertise on cardiac implantable electronic devices, structural heart disease, peripheral vascular conditions, cardiovascular disease and prevention, electrophysiology, critical care cardiology, heart failure, and pre-, peri-, and post operative procedures. Faculty members represented a variety of geographic locations, academic and community-based practice settings, institution sizes, and career stages. Faculty embodied practice acumen and cardiology team model care expert knowledge.
In addition to the faculty, cardiologists and cardiology specialists as key presenters contributed to the 1-hour learning module presentations, forming an interprofessional partnership in the successful execution of the novice to competent (25 hours of CEs) core curriculum didactic modules. The project is ongoing with expansion of “competent to expert” didactic modules (19 hours of CEs). The integration of didactic courses into orientation and competency programs ensures a standardized approach to education, promoting consistency and quality across healthcare settings. By establishing clear learning objectives and performance expectations, the core curriculum courses help to streamline the onboarding process for new hires and facilitate ongoing professional development for experienced staff.
The CCL core curriculum didactic courses form the cornerstone of the VHA Cardiac Catheterization Lab Nursing Orientation and Core Competencies Guidebook, laying the groundwork for nursing excellence in this specialized field. By investing in comprehensive education and training, healthcare organizations can ensure nursing staff are equipped to improve outcomes for patients with cardiovascular disease.
Refining past conversations (We Need to Start an Educational Conversation: Frameworks for Orientation Success in the Cardiac Catheterization Lab [Part I] and Continuing an Educational Conversation: Functionality and Implementation for Orientation Success in the Cardiac Catheterization Lab [Part II]), our team leveraged those foundational concepts with success. The core didactic courses consist of fundamental courses, layering foundational knowledge from basic cardiovascular anatomy and physiology intertwined with coronary artery disease pathology, up through advanced professional certification concepts (Tables 1-2). This discussion will expand on the results from the execution of the Novice to Competent CCL Core Curriculum Didactic Courses. Competent to Expert courses are being developed and executed.
These courses underpin the novel VHA Cardiac Catheterization Lab Nursing Orientation and Core Competencies Guidebook, a 60+ page orientation and competency standards guide for CCL leaders and professionals. The principal goal for Cardiac Catheterization Lab Core Nursing Competency statements within the Guidebook is to provide a framework for nursing professional development and CCL specialty clinical competency standards for the coordinated recognition and preservation of scope and standards of care delivery within the CCL nursing specialty.
The CCL core competencies provide the critical base for practice and baseline knowledge. The competency standards presented later in this discussion distinguishes the vital knowledge and skills required for CCL nursing professionals working in the CCL specialty, thereby supporting nurses in identifying learning needs and professional development opportunities. Acknowledgement of the specialized competency for CCL procedural care increases the understanding of the depth and role CCL nurses contribute within the specialty procedures cardiovascular team which in turn encourage and improve collaborative, high-quality, patient-centered care delivery.
Results
Participants in the core curriculum course learning were predominantly nurse attendees with less than 10% in each course being other interprofessional partners. Evaluation reports from the learning management system were reviewed, covering course modules 1–25 (Novice to Competent CCL Core Curriculum Didactic Courses). Each included standardized participant satisfaction metrics, self-assessed learning outcomes, and open-ended feedback. Descriptive statistics were used to calculate satisfaction rates, application to job performance, and self-reported learning.
Over the course of the didactic program, attendees consistently reported high levels of satisfaction with their learning experience. Through 1-hour didactic lectures, staff were provided with a dynamic, manageable, and consistent educational experience. The curriculum was designed to cater to staff with limited time for sessions and recorded material ensuring that staff could access after the “LIVE” presentation throughout the program and their learning schedules. Overall predominant feedback indicated that staff found the content relevant, informative, and well-presented, contributing to a positive overall learning environment.
One of the primary goals of the CCL core curriculum was to equip nurses with the knowledge and skills necessary to excel in their roles. The feedback from CCL leaders and staff via emails received following the course revealed significant gains in knowledge acquisition among participants, with nurses demonstrating a deeper understanding of cardiovascular base knowledge, procedural techniques, and patient care principles. Participants reported feeling more confident and competent in their abilities to perform their duties effectively following the completion of the program.
Most notably, the evaluation demonstrated exceptionally high levels of learner satisfaction with the cardiac cath lab core curriculum over the span of all 25 courses, averaging 4.02 (lowest reported average) of learner satisfaction out of a 5.0 rating system using standardized learner satisfaction statements.
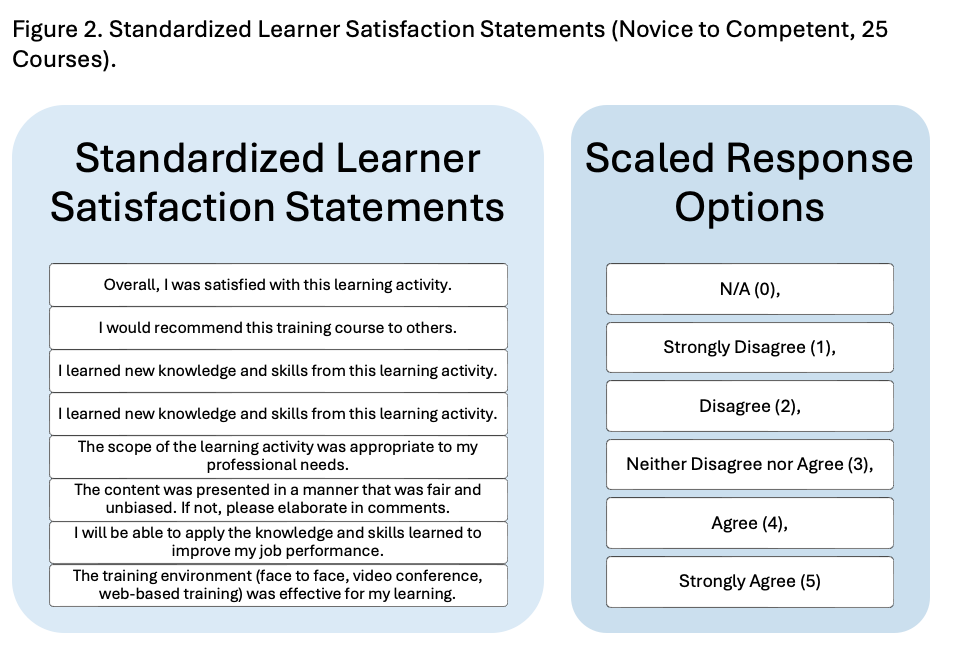
Further, all 25 courses illustrated a consistent 60% of all attendee response of a “fair amount” (second highest self-reported learning) or “a great deal” (highest self-reported learning) to the standardized question “How much did you learn as a result of this CE program?” with less than 3% of all attendee responses reporting “very little” (lowest self-reported learning) or “little” (second lowest self-reported learning) across all courses.
Participants expressed appreciation for the quality and relevance of the educational content, as well as the expertise and support provided by instructors throughout the program. Additionally, attendees reported feeling valued and supported by the organization, which had invested in their professional development through participation in the curriculum. The overwhelmingly positive feedback from participants underscores the success of the program in meeting the needs and expectations of CCL nurses, possibly contributing to high levels of job satisfaction and retention within the nursing workforce. As we have discussed a high value-add learner experience, it is equally important to discuss notable comments and field notes from each course. To succinctly organize each of these, please see the below tables to see how each course possesses notable details.
In summary, the evaluation of the CCL core curriculum revealed a resoundingly positive impact on learner experience, knowledge acquisition, and learner satisfaction. By providing nurses and interprofessional staff with a comprehensive and engaging educational experience, the curriculum provided an avenue for enhanced clinical competence and fostered a culture of learning and professional growth within CCL settings. These findings highlight the importance of investing in robust orientation and competency programs to support the ongoing development of nursing staff and ultimately improve outcomes for patients with cardiovascular disease.
12 Domains of CCL Core Competency, Model for Standardization
The VHA Cardiac Catheterization Lab Nursing Orientation and Core Competencies Guidebook outlines 12 Domains of Nursing Core Competencies for Cardiac Catheterization Lab (CCL). This guidebook has several important implications for the field of CCL nursing, as well as for broader interprofessional and healthcare system practices. Within the VHA CCL Nursing Orientation and Core Competencies Guidebook, each domain contains critical concept competency statements. The critical concept competency is the foundational competency that must be met to support unit specific competencies (for example, industry-specific equipment management or facility-specific CCL emergency process). The CCL Core Competencies listed below are used to fortify the basic knowledge and skills required for a nurse professional to be a safe, effective member in the CCL environment. These critical concept competencies require the equipment and facility/unit-specific competency development, which articulate more detailed requirements for knowledge, skills, attitudes (KSAs) for professionals in the CCL to achieve and sustain.
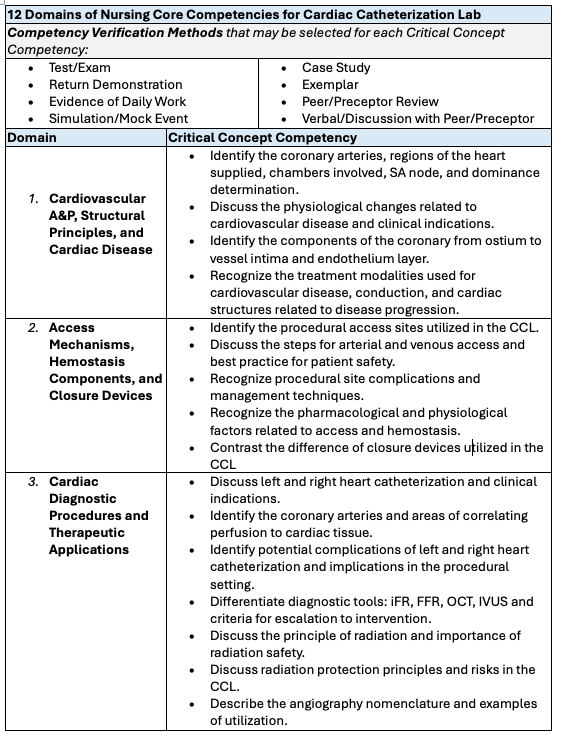
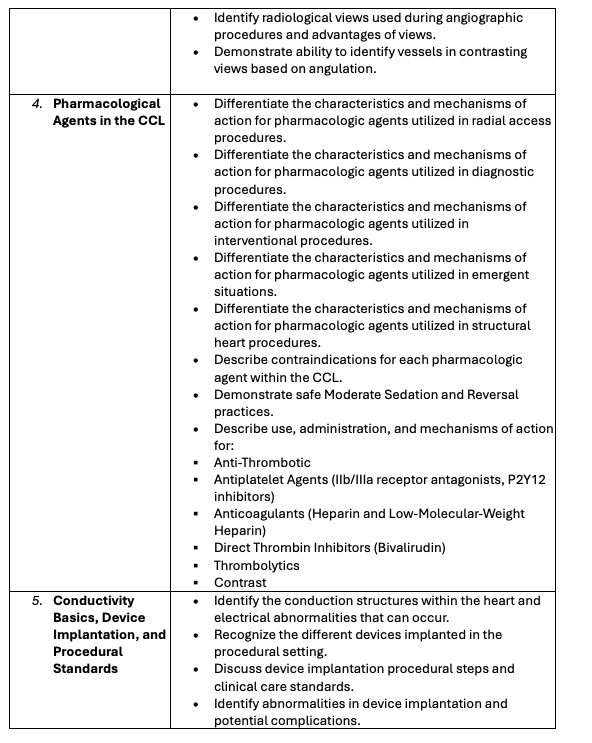
Standardization of practice across facilities through the core competency domains ensures consistency in nursing practice across CCLs, especially within large healthcare systems like the VHA. This minimizes variation in care delivery and promotes safe, high-quality outcomes. Standardization of foundational competencies provides an easier benchmark for performance and facilitates smoother adaptations when facing the evolving complexity of equipment and procedures performed in the specialty setting.
Second, establishing a stronger focus on foundational competency provides essential safety and effectiveness principles all nurses must master, irrespective of location or equipment differences. The essential safety implication ensures that all CCL nurses, even before learning facility-specific practices, understand life-saving protocols, patient monitoring, sterile techniques, and other non-negotiables. The need for both foundational competency domains and unit-specific competencies encourages ongoing professional development, bridging education and practice. As technology, techniques, and patient populations evolve, this approach fosters a growth mindset and prepares nurses to adapt to new challenges in interventional cardiology.
Lastly, clearly defined competencies enable CCL nurses to function more effectively in high-pressure interdisciplinary teams. CCL nurses often collaborate with several interprofessional partners in each procedural case. Competency clarity improves role understanding, communication, and team performance in critical situations. Further, new nurses or those transitioning into the CCL role have a clear, structured orientation path, reducing variability in onboarding experiences, resulting in faster, more efficient onboarding and improvement of staffing flexibility that helps mitigate the effects of workforce shortages. Nurses trained in these domains are more likely to apply evidence-based decision-making, because the competencies include critical thinking, safety, and clinical judgment.
Future Research and Implications
The development and implementation of the VHA Cardiac Catheterization Lab Nursing Orientation and Core Competencies Guidebook represent a substantial advancement in standardizing education and competency expectations across CCLs. However, future research is needed to longitudinally evaluate the impact of this curriculum on clinical outcomes, team efficiency, patient safety metrics, and workforce retention. Studies should also explore the scalability and adaptability of this model across non-federal healthcare settings and diverse practice environments.
The authors recognize that implementing a lengthy orientation program for CCL nurses presents several challenges for healthcare organizations. Extended training periods can delay nurse integration, potentially affecting staffing levels and workflow efficiency. However, the risks associated with inadequate training far outweigh these concerns, as patient safety remains the top priority. Additionally, prolonged orientation programs can be costly, demanding significant financial and personnel resources for instruction, materials, and mentorship. A rigid, extended program may also fail to accommodate varying experience levels, leading to frustration among seasoned nurses who feel their time is not being utilized effectively. Striking a balance between comprehensive training and efficiency is essential to ensure nurses are well-prepared while minimizing operational disruptions, an approach strongly supported by the Core Curriculum.
Further inquiry into interprofessional training integration, simulation-based competency assessments, and the use of emerging technologies such as virtual reality or artificial intelligence in cath lab education may yield valuable insights for evolving clinical education models. Additionally, qualitative research capturing the lived experiences of nurses undergoing the orientation can illuminate barriers, facilitators, and potential refinements to the program. The positive initial outcomes from this novel initiative underscore the need for ongoing investment in structured professional development frameworks to sustain excellence, build resilient interdisciplinary teams, and respond to increasing procedural complexity in cardiovascular care.
Acknowledgements.
Special gratitude to our now retired key faculty (Cathy Clark MS, RN, RCIS and Cynthia Wilson, RN) for their tireless dedication.
Special acknowledgements to the outstanding Core Curriculum SME presenters that dedicated their time and expertise to make this curriculum possible.
References
1. Yaqoob Mohammed Al Jabri F, Kvist T, Azimirad M, Turunen H. A systematic review of healthcare professionals' core competency instruments. Nurs Health Sci. 2021 Mar; 23(1):87-102. doi:10.1111/nhs.12804
2. Writing Committee; Bass TA, Abbott JD, Mahmud E, et al. 2023 ACC/AHA/SCAI Advanced Training Statement on Interventional Cardiology (Coronary, Peripheral Vascular, and Structural Heart Interventions): A Report of the ACC Competency Management Committee. J Soc Cardiovasc Angiogr Interv. 2023 Feb 16; 2(2): 100575. doi:10.1016/j.jscai.2022.100575
3. Liu Y, Aungsuroch Y. Current Literature Review of Registered Nurses' Competency in the Global Community. J Nurs Scholarsh. 2018 Mar; 50(2): 191-199. doi:10.1111/jnu.12361
4. Mrayyan MT, Abunab HY, Abu Khait A, Rababa MJ, Al-Rawashdeh S, Algunmeeyn A, Abu Saraya A. Competency in nursing practice: a concept analysis. BMJ Open. 2023 Jun 1; 13(6): e067352. doi:10.1136/bmjopen-2022-067352
5. Naidu SS, Abbott JD, Bagai J, et al. SCAI expert consensus update on best practices in the cardiac catheterization laboratory: This statement was endorsed by the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS) in April 2021. Catheter Cardiovasc Interv. 2021 Aug 1; 98(2): 255-276. doi:10.1002/ccd.29744
6. Administration, V.H. About VHA. 2023; Available from: https://www.va.gov/health/aboutvha.asp.
7. Dickerson, P., Core Curriculum for Nursing Professional Development. 5th ed. 2017: Association for Nursing Professional Development (ANPD).
8. Duchscher JB, Windey M. Stages of Transition and Transition Shock. J Nurses Prof Dev. 2018 Jul/Aug; 34(4): 228-232. doi: 10.1097/NND.0000000000000461
9. Duchscher JE. Transition shock: the initial stage of role adaptation for newly graduated registered nurses. J Adv Nurs. 2009 May; 65(5): 1103-1113. doi:10.1111/j.1365-2648.2008.04898.x
10. Murray M, Sundin D, Cope V. Benner's model and Duchscher's theory: Providing the framework for understanding new graduate nurses' transition to practice. Nurse Educ Pract. 2019 Jan; 34: 199-203. doi:10.1016/j.nepr.2018.12.003
11. Kadavath S, Mohan J, Ashraf S, et al. Cardiac Catheterization Laboratory Volume Changes During COVID-19-Findings from a Cardiovascular Fellows Consortium. Am J Cardiol. 2020 Sep 1; 130: 168-169. doi:10.1016/j.amjcard.2020.06.009
12. Riley RF, Alasnag M, Batchelor WB, et al. The Ongoing National Medical Staffing Crisis: Impacts on Care Delivery for Interventional Cardiologists. J Soc Cardiovasc Angiogr Interv. 2022 May-Jun; 1(3): 100307. doi:10.1016/j.jscai.2022.100307
13. Le DE, Arora BL, Kelly FR, et al; ACC Federal Cardiology Leadership Council. The Quality of Veterans Healthcare Administration Cardiovascular Care. JACC Adv. 2025 Feb; 4(2): 101533. doi:10.1016/j.jacadv.2024.101533
14. (US), I.o.M., Institute of Medicine (US) Committee on Planning a Continuing Health Professional Education Institute. Redesigning Continuing Education in the Health Professions. 2010, Washington (DC): National Academies Press (US).
15. Zarei M, Mojarrab S, Bazrafkan L, Shokrpour N. The role of continuing medical education programs in promoting iranian nurses, competency toward non-communicable diseases, a qualitative content analysis study. BMC Med Educ. 2022 Oct 24; 22(1): 731. doi:10.1186/s12909-022-03804-x











