Minimizing Points of Failure During Upper Extremity Right Heart Catheterization
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Faris G. Araj, MD
Division of Cardiology, Department of Internal Medicine, The University of Texas Southwestern Medical Center, Dallas, Texas
Disclosures: Dr. Araj reports no conflicts of interest regarding the content herein.
To the Editor:
The article by Marie E. Maranda, RN, regarding ultrasound-guided venous access for arm cases published in the April 2025 issue of Cath Lab Digest was most insightful and helpful.1 To the best that I can tell, it has been close to a decade since CLD has published on the topic of upper extremity right heart catheterization.2
I have always been in awe of how effortless and highly successful a bedside peripherally inserted central catheter (PICC) line placement is without the use of fluoroscopy. It is far more challenging to access a smaller vessel in the arm than a larger vessel in the neck or groin for right heart catheterization, because I was not trained in performing upper arm right heart catheterization during fellowship. I personally find most of the anxiety that surrounds performing a right heart catheterization via the upper extremity stems from 2 main scenarios: (1) Unsuccessful venous access and (2) inability of the pulmonary artery (PA) catheter to enter the right heart.
I have mostly encountered the former when I am trying to wire over a pre-existing IV placed in the pre-procedure area by one of the nursing staff who did not have the experience or expertise level of Ms. Miranda.1 Though I would fairly consider myself a novice in performing right heart catheterization via the upper extremity, I have focused my efforts on maximizing success of the above 2 scenarios of failure. Perhaps others may find this helpful as they too embark on this type of procedure.
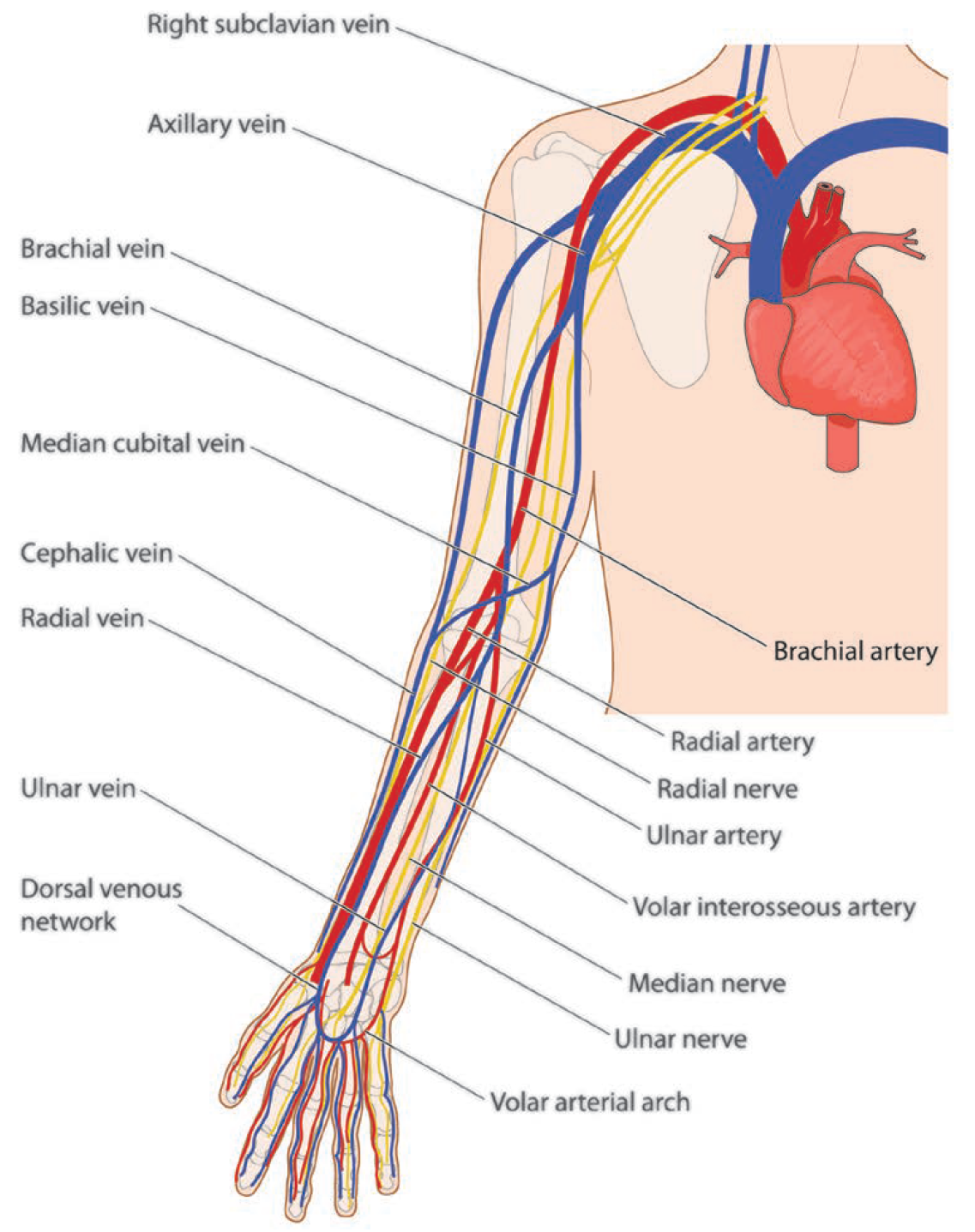
I always perform a screening ultrasound of the upper arm veins before committing to the procedure. Given that the use of the cephalic vein can be more challenging,2 I restrict my access to the more medial vessels either of the brachial or basilic vein, and higher up in the arm, so that less navigation is involved. The screening ultrasound should be performed with a tourniquet on, as it can markedly increase the vein caliber with better visualization. The area is marked and then prepped in a sterile manner. I always ask the staff to kindly prepare the ipsilateral neck or groin in case upper arm right heart catheterization is unsuccessful. The same equipment can be used to perform the procedure at an alternative location.
The radial access kit is my ‘go-to’ for access. If the vein is too deep, then I use a longer micropuncture needle. I ensure that my gloves fit tightly so that I can feel the tactile “pop” as the needle tip enters the vein. For patient comfort, I provide local lidocaine to the access site using an 0.5 to 1 mL insulin syringe. It is paramount to ensure that the vessel of interest is in the center of the ultrasound screen and that my orientation of left to right is predetermined so that there is no guessing as to which way to redirect the needle under real-time ultrasound.
Prior to entering the skin, I have the needle filled to the brim with saline. I find this helpful for 2 reasons: (1) When I see the saline drip out, that is a sign that I am intravascular, because the venous blood has displaced the saline. I notice this faster than waiting for blood to travel from the tip to the end of the needle. (2) The saline acts as somewhat of a magnifying glass, and if the venous pressure is low and the saline does not drip, then I can see the blood much better when looking down the needle. As the needle moves towards the vessel, a slight tilt of the ultrasound probe cephalad can help follow the needle trajectory to ensure the path of entry is aligned with the center of the vessel and if not, to modify accordingly.
To increase my confidence that I can successfully get from the arm to the right heart with the PA catheter, once I am intravascular, I hold the needle steady, advance a 180 cm SV-5 wire (Cordis) gently through the needle and advance up the arm, navigating towards the right heart. This can be done fairly quickly with the use of minimal fluoroscopy. Then, in rapid sequence, the needle is removed and a small incision made to accommodate the 6 French (Fr) Glidesheath (Terumo). Everything is done over the SV-5 wire, which remains held in place with its tip in the superior vena cava (SVC) or right atrium (RA). After the 6 Fr sheath is in, we frontload a 6 Fr PA catheter over the wire with the balloon deflated. This takes the guesswork out of the equation.
Alternatively, once venous access is obtained, a 5 Fr micropuncture sheath can be placed in the vein over a wire and then scouting the path with the 180 cm SV-5 wire to the right heart can be performed. The wire can then be used to support the catheter if needed to go directly to the wedge position, and from that point forward, a right heart pullback can be performed without fluoroscopy.
I have found that by systematically following the above process, I can eliminate possible points of failure and successfully complete the procedure. The only downside that I see to this technique is the upfront added cost of the SV-5 wire.
Acknowledgments: I would like to thank all the wonderful UTSW Cath Lab Staff for their expertise, knowledge, and patience. I am better at what I do because of them.
References
1. Miranda, ME. Ultrasound-guided venous access for arm cases. Cath Lab Digest. 2025 April; 3(4): 24-26. Accessed May 19, 2025. https://www.hmpgloballearningnetwork.com/site/cathlab/ultrasound-guided-venous-access-arm-cases
2. Nanavaty SP, Pancholy SB. Right heart catheterization from an upper extremity. Cath Lab Digest. 2016 Feb; 24(2): 1, 23. Accessed May 19, 2025. https://www.hmpgloballearningnetwork.com/site/cathlab/article/right-heart-catheterization-upper-extremity










