Real-World Experience With the Paradise™ Ultrasound Renal Denervation System
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Orestis Pappas, MD, FACC, FSCAI, FSVM
Saint Vincent Hospital and Erie Veterans Affairs Medical Center, Erie, Pennsylvania
Dr. Orestis Pappas, of Erie, Pennsylvania, shares his clinical experience using the Paradise™ Ultrasound Renal Denervation (uRDN) System (Recor Medical) in a series of patients with uncontrolled hypertension under his care. He reflects on his patient outcomes and lessons learned on more than a dozen patients from his clinic.
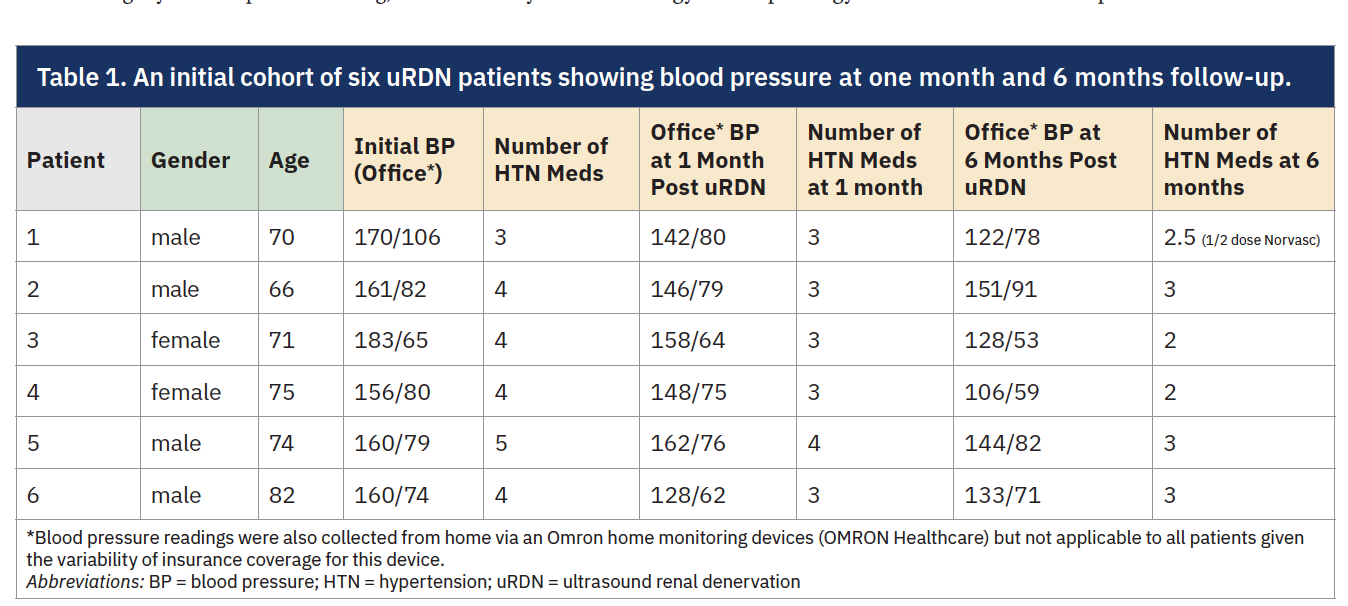
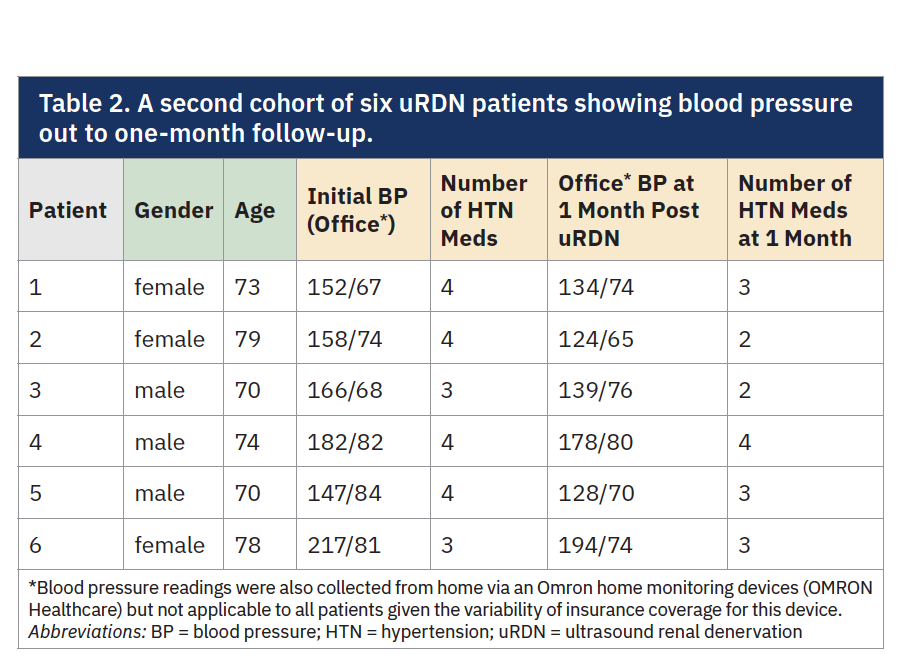
 You have completed at least 12 cases with the Paradise Ultrasound Renal Denervation System (Tables 1-2). What kind of clinical outcomes and blood pressure trends are you seeing in your patients?
You have completed at least 12 cases with the Paradise Ultrasound Renal Denervation System (Tables 1-2). What kind of clinical outcomes and blood pressure trends are you seeing in your patients?
Our outcomes have been a little more dramatic than what was reported in the clinical trials, and that is probably because we are treating a sicker population than the population qualified for the procedure in the clinical trials. We are starting with a higher baseline; therefore, we have a higher drop in the blood pressure. In our first cohort of six patients treated with ultrasound renal denervation, we saw an average systolic drop of 29.5 mmHg, and that reduction has held steady for six months. The median reduction in blood pressure from baseline to 6 months post uRDN across the six patients was:
• Systolic BP: ↓ 37.5 mmHg
• Diastolic BP: ↓ 7.5 mmHg
This reflects a substantial and consistent reduction in systolic pressure with more modest changes in diastolic pressure. A second cohort is now a little over a month out, and we are seeing similar trends. What is also interesting is the stability we’re seeing, meaning fewer spikes and fewer symptomatic surges. Patients report fewer side effects, especially when we can get them off medications such as clonidine. That alone improves quality of life.
Tell us more about how these patients are coming to you. What does your selection and referral process look like?
About three years ago, we built a dedicated hypertension clinic in anticipation of renal denervation gaining approval. We worked closely with cardiology and nephrology to identify patients who were tough to manage, people already on multiple medications and still not controlled. We also made sure the program made sense operationally. We brought in a physician assistant to run the clinic. She reviews patients and then runs them by the cardiologists. Right now, we’re only accepting referrals from cardiology and nephrology, and that helps ensure we’re seeing patients with true resistant hypertension. These patients are already under specialist care and have exhausted most conventional options.
Every patient we consider gets a full workup. That includes renal ultrasound and hormone panels to rule out secondary causes. We also ask them to monitor their blood pressure at home using an ambulatory device for at least a month. That gives us a clear baseline and also shows us they’re engaged in their care. It’s kind of like an unwritten agreement that shows us patients are committing to this process just like we are.
What are the common secondary causes of hypertension that you see in this population?
Obstructive sleep apnea, no question. Renal artery stenosis is next, especially in older patients. We haven’t seen many adrenal tumors or other rare causes. But sleep apnea is a big one, and we work closely with sleep medicine to get those patients on CPAP and compliant.
The other big piece is lifestyle. A lot of this comes down to salt, smoking, alcohol, and lack of exercise. That’s where the mid-level provider makes such a difference, because their 30-minute visits focused just on hypertension allow for education and motivation in a way we can’t do in a regular office visit.
What is involved in the pre-procedure evaluation once you have identified a candidate?
Almost all of these patients have some degree of renal impairment, so we try to avoid contrast whenever we can. If they’ve had a CT scan for another reason, we will use it. Otherwise, everyone gets a renal ultrasound. We are looking for any anatomical variations, and we measure flow velocities to rule out significant stenosis from atherosclerosis or fibromuscular dysplasia. We don’t routinely use a CT scan for planning unless it is already available. That decision really comes down to concerns around kidney function in these patients. The ultrasound tells us what we need in most cases.
Have you adjusted your approach over time when it comes to procedural sedation, imaging, or managing medications?
Definitely. At first, we had anesthesia involved, thinking renal denervation would be a more uncomfortable procedure. But anesthesia resources are limited, and after a few cases, we realized it wasn’t necessary.* Our nurses use a sedation protocol that combines the usual fentanyl and midazolam with a 0.5 mg dose of IV hydromorphone just before sonication. That has been a game-changer. It keeps the patient comfortable during the bursts of ultrasound, which are less than 10 seconds, and we haven’t had to stop a procedure or give additional meds. It is more demanding for the nurse managing sedation, because the patient has to be in a deeper state than with a diagnostic cath, but it is still very doable. Patients tolerate it well and there haven’t been any complaints of discomfort. We discharge patients on their existing medications and use the home blood pressure readings to guide any adjustments. The hypertension clinic handles those follow-ups.
Are there anatomies or clinical situations where you think the Paradise uRDN system works especially well?
Yes, I would say particularly when the renal arteries have a lot of branching. The Paradise uRDN system requires only 2-3 balloon inflations per artery (per IFU), as long as you have about 2.5 cm of usable vessel in the main renal artery. You usually don’t need to go into the branches [Note: anatomies may vary]. That makes the procedure quicker, with less contrast use, less painful for the patient, and easier overall. In roughly half of our cases, we can even use the same balloon on both sides.
Are there any cost considerations if you use more than one balloon?
As far as cost goes, it is bundled per case, not per balloon. If we end up using two or even three balloons — for example, if there is an accessory renal artery — the cost is the same. That makes planning a lot easier. We can make decisions based on the patient’s anatomy without having to worry about cost implications.
Can you address ease of use for this device?
From both an operator and staff standpoint, the Paradise uRDN system is quite easy to use. There is nothing to assemble. It comes ready, just like any other catheter we use in the lab. The balloon is extremely soft and ultra-compliant, which makes it very forgiving. If you match the balloon size 1:1 with the vessel, it is even smoother. We have tried both the 7 French (Fr) and the 8 Fr catheters.
What has your learning curve been like?
As with everything in the beginning, you need to take your time, both as an operator and as staff, until you get familiar with the necessary hand-eye coordination and in conjunction with the different anatomies in the renal arteries. I also needed to train two different teams of staff for scheduling purposes. After the third case, the entire team was comfortable. We do prepare carefully. The night before, we review the cases and make sure everyone knows the plan, including what wires to use, what guides, and any anatomy issues from prior imaging. It makes a big difference the next day.
Which guides do you typically use?
It depends on the anatomy, but we usually work with Judkins right (JR) 4, right coronary bypass (RCB), or internal mammary artery (IMA) guides. If we don’t have a CT scan ahead of time, we will do an abdominal aortogram with a pigtail to find the takeoffs. If it’s a sharp angle, we go with an IMA. If it’s more straightforward, we use a JR4 or RCB.
What are your thoughts on the safety profile of the Paradise uRDN after your experience?
Safety is excellent. The way the system is designed, the balloon touches the vessel wall, but the ultrasound emitter sits a few millimeters inside that. It is engineered to target the nerve layer and avoid damaging the artery; coolant fluid circulating inside the balloon keeps the inner vessel wall temperature low to help protect it from thermal injury during ablation.1 It’s smart technology. We always take a picture after the procedure, and thus far, we have not seen any vasospasm, dissection, or any complications requiring further intervention.
What technical tips would you offer for the first few cases?
Give the hydromorphone before sonication to keep the patient comfortable. Take the time to go over the case with your team the night before. Make sure you measure the renal artery accurately so you are correctly matching the balloon sizing in a 1:1 fashion, which helps with apposition and helps ensure the energy is delivered appropriately.
How do you set expectations for patients going into this procedure?
We tell patients it is a same-day procedure and they will go home in about four hours, similar to a standard femoral access cath. But we also make it very clear that renal denervation is not a cure. It’s not one-and-done. They still need to take their meds and stick with lifestyle changes. If we are able to scale back their medications over time, that is a win, but it is not guaranteed. The goal of the procedure is to help reduce their blood pressure.
References
1. Pathak A, Coleman L, Roth A, et al. Renal sympathetic nerve denervation using intraluminal ultrasound within a cooling balloon preserves the arterial wall and reduces sympathetic nerve activity. EuroIntervention. 2015 Aug; 11(4): 477-484. doi:10.4244/EIJV11I4A96
This article is sponsored by Recor Medical.
Dr. Pappas is a paid consultant of Recor Medical, Inc., and has been compensated for his time and expertise in participating in this content. The views expressed in the article are his own and based on his own personal experience with the Paradise System. Results may vary.
Paradise is a registered trademark of Recor Medical, Inc.











