PTAB With the DETOUR™ System: Expanding Treatment Options for Complex PAD Patients
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Hear from Dr. Golzar in the video below.
CLD talks with:
Jaafer A. Golzar, MD, FACC, FSCAI
Director of Endovascular Intervention, Advocate Christ Medical Center; Director of Limb Salvage & Endovascular Intervention, Advocate Trinity Hospital Chicago, Illinois
Can you explain how PTAB with the DETOUR™ System provides an alternative approach for complex PAD patients?
The DETOUR System (Endologix) and percutaneous transmural arterial bypass (PTAB) represents a truly exciting addition to our armamentarium for the treatment of complex peripheral artery disease (PAD) patients. As an interventional cardiologist, one of the primary limitations we face is our inability to perform traditional surgical bypass. The DETOUR System, however, offers a minimally invasive, percutaneous approach that significantly broadens our capabilities in managing these challenging cases. Percutaneous bypass has opened a new realm of possibilities for patient care. It provides a safe, effective, and minimally invasive option that reduces hospital stays and ultimately improves patient outcomes. This approach is particularly valuable for patients who are high-risk candidates for surgery, those who have previously undergone open bypass with subsequent failure, or those with complex anatomical challenges.
There are several patient subsets where this technique is especially beneficial. First, patients with previous bypass grafts that have failed represent a clear opportunity, as they are high-risk candidates for repeat bypass surgery. Second, those who have undergone previous endovascular procedures that were unsuccessful and are now considered high-risk for open surgery are ideal candidates. Additionally, patients with severe calcification, particularly those presenting with de novo lesions in the superficial femoral artery (SFA), pose a significant challenge for standard endovascular approaches due to poor durability. For these patients, percutaneous bypass offers a promising alternative.
I tend to think about long, heavily calcified SFA chronic total occlusions (CTOs) with reasonable runoff as optimal cases for this approach. Of course, the quality of the runoff vessels plays a critical role in determining the success of percutaneous bypass, which we can discuss further. But overall, the DETOUR System provides a valuable new tool for improving outcomes in patients who would otherwise have limited options.
How are these patients coming to you, and how do you identify and assess them for treatment?
As a tertiary care center, we receive patients from all over the country, many of whom have already experienced failure with previous endovascular procedures or bypass surgeries. For these individuals, our intervention often represents a last-ditch effort at limb salvage. Additionally, we see patients presenting with claudication who are suitable candidates for these procedures.
Our evaluation process begins with noninvasive testing, typically through arterial duplex ultrasound or computed tomography (CT) angiography. I prefer CT angiography because it provides a comprehensive view of not only the level of arterial occlusion but also the venous anatomy. This is crucial, because with these procedures, we are intentionally crossing from the artery into the vein and then back into the artery. Therefore, it is essential to confirm the absence of deep vein thrombosis (DVT) and to ensure healthy veins are present before proceeding.
When assessing patients, I look for at least one viable runoff vessel extending all the way down to the foot. During the angiogram itself, we further evaluate the runoff vessel to confirm its suitability.
Another critical aspect of the process is patient education. I make sure to thoroughly explain the procedure, including its relatively recent adoption, success rates, and the fact that traditional open bypass surgery remains a valid option. Patients must understand the importance of close follow-up, which is crucial for maintaining the durability of the intervention.
Follow-up includes ultrasounds at two weeks, three months, six months, and every six months thereafter. This allows us to monitor for potential edge stenosis or disease progression, and intervene early if necessary to ensure the best possible outcomes.
What patient population benefits most from PTAB therapy, and how does it fit within the current treatment algorithm for PAD?
I believe that all the tools we have in our toolbox contribute to improving outcomes for our patients. It is essential to recognize that no single technology, whether orbital atherectomy, laser atherectomy, drug-eluting stents, or other modalities, can be considered a standalone solution. The DETOUR System and PTAB offer another valuable tool in our toolbox, particularly for patients who are high-risk surgical candidates or those who have exhausted other endovascular options.
PTAB therapy is especially advantageous for patients with advanced PAD who have previously undergone failed endovascular interventions or open bypass surgery. It also benefits patients with long, heavily calcified CTOs of the SFA, particularly when there is adequate distal runoff. These are patients for whom conventional endovascular techniques may provide suboptimal results or poor durability.
This approach fits into the current treatment algorithm by providing an alternative pathway for patients who would otherwise be deemed inoperable or unsuitable for further endovascular intervention. Rather than reaching a point where we have nothing left to offer, PTAB expands our options and offers hope to patients who might otherwise face amputation.
Can you walk us through the DETOUR procedure?
The DETOUR procedure involves a series of carefully coordinated steps aimed at achieving successful percutaneous transarterial bypass. The procedure begins with the placement of an 8 French (Fr) crossover sheath, followed by establishing pedal venous access. This access can be obtained via the posterior tibial vein, anterior tibial vein, or preferably the dorsal pedis vein. After placing a 6 Fr sheath, an initial angiogram is performed from the pedal vein to confirm the presence of a healthy, robust femoral vein.
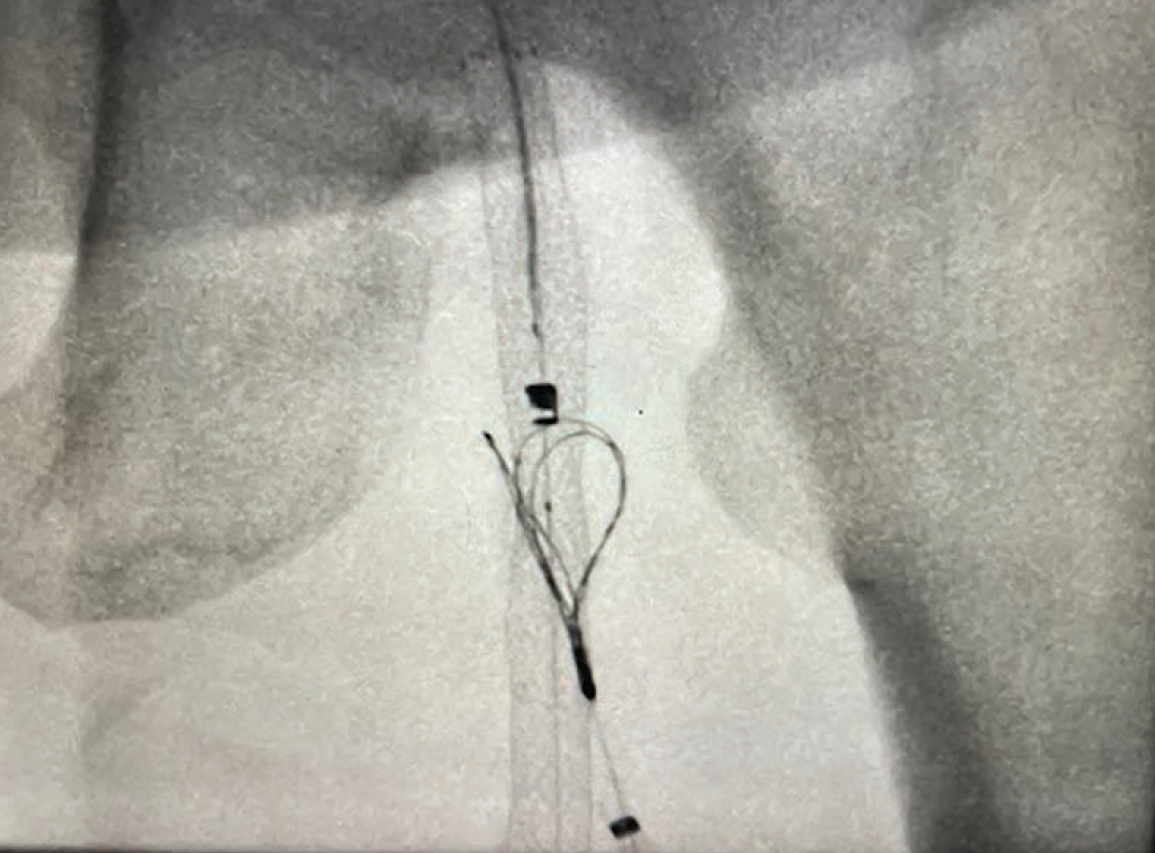
Next, the process involves crossing into the SFA CTO. This may include a stump occlusion, or a proximal or mid occlusion. The specific location of the occlusion is less important than ensuring there is approximately 5 cm of runway before exiting the artery. The ENDOCROSS™ device, a spring-loaded dual guidewire delivery tool with an .025-inch nitinol needle with a 15 mm throw, is then used to exit the artery and enter the vein. It functions similarly to a Pioneer (Philips) or Outback (Cordis), providing an effective exit strategy to facilitate the transition from the artery to the vein.
Once the artery-to-vein crossing is achieved, the wire is snared from the artery into the vein and then externalized. This externalized wire is essential for the subsequent step of reentering the artery. The newly created anastomosis between the artery and the vein is then predilated to prepare for reentry.
The ENDOCROSS device is reintroduced and then we identify the reentry zone, which is typically located in the P2 or P3 segment of the popliteal artery. Once reentry into the artery is successfully achieved with the ENDOCROSS, the anastomosis is further dilated to ensure adequate flow. Following this step, the Torus stent grafts provided by the DETOUR System are deployed. The stents are placed from the popliteal artery, into the vein, and back into the SFA. It is very important the stents are placed correctly to exclude the entire area of disease, all the way up to the ostium of the SFA. The main failure zone is typically due to either proximal or distal edge stenosis, or progression of disease distally, so to minimize that possibility, the covered stent needs to be placed right at the ostium of the SFA. The entire procedure generally takes about an hour and a half from skin to skin. I prefer to perform the procedure under monitored anesthesia care (MAC) due to the need for pedal access. Most patients are discharged the same day and tend to experience good outcomes post procedure.
What are you looking for once you complete the procedure?
There may be the appearance of sluggish flow through the graft. This phenomenon often results from the de-collateralization of the profunda femoral artery. When there is a CTO of the SFA, blood flow is diverted into the profunda femoral artery, which develops significant and robust collateral circulation over time. When blood flow is redirected from the profunda artery into the newly established graft, it may initially appear sluggish due to competitive flow from the profunda into the graft. However, this sluggishness typically resolves within minutes to hours as the profunda artery gradually decollateralizes.
To accurately assess flow, I like to place a catheter directly into the graft and inject contrast through it. This approach helps exclude the influence of the profunda artery and allows for a clearer evaluation of the graft’s patency and function.
After confirming satisfactory flow through the graft, your attention should turn to the outflow vessels. I do not typically address outflow vessels during the same setting as the revascularization procedure. Instead, I ensure that the outflow vessels are in acceptable condition before proceeding with the revascularization. If staged revascularization of infrapopliteal vessels is needed, it can always be performed at a later date. However, we have not found this to be necessary thus far, as successful outcomes are largely dependent on meticulous pre-procedure planning.
How do you manage these patients post procedure?
We follow the post-procedure management protocols established by Endologix, which involve a regimen of triple therapy during the first month after the procedure. This regimen includes aspirin, clopidogrel, and low-dose rivaroxaban (2.5 mg). After the initial month, aspirin is discontinued, and the patient is maintained on clopidogrel and 2.5 mg of rivaroxaban.
Patients return to the office for follow-up at two weeks post-procedure, during which we perform an arterial duplex ultrasound to ensure the graft appears healthy, there are no signs of edge stenosis, and no critical findings have been missed. We also conduct a venous duplex ultrasound to check for any deep vein thrombosis (DVT). The clinical trial data suggest that the risk of DVT associated with this procedure is very low, approximately 2%.1
During follow-up visits, I assess the patient’s overall condition and provide reassurance if they are experiencing reperfusion edema, which can occur due to the sudden increase in blood flow reaching the foot. This post-revascularization edema is typically benign and improves over time. If the edema is particularly bothersome for the patient, I may recommend the use of low-dose compression stockings, providing 10 to 15 mm of mercury of knee-high compression. However, this has only been necessary in one or two patients who experienced significant discomfort. In all cases, the edema has gradually resolved with time.
What long-term clinical evidence is available to support the efficacy and durability of PTAB therapy with the DETOUR System?
The availability of robust long-term clinical evidence is critical for the widespread adoption and growth of PTAB therapy using the DETOUR System. The clinical trials team has done a phenomenal job of analyzing and mining data even beyond initial publication to build a comprehensive understanding of the procedure’s efficacy and durability.
When examining the primary patency, the data show a primary patency rate of approximately 81% at one year.1 However, from an endovascular standpoint, we often focus on primary patency defined by a peak systolic velocity ratio (PSVR) of 2.5. To truly compare apples to apples, we need to consider patency, which simply determines whether the bypass is open or closed at one year, similar to how we evaluate traditional surgical bypass grafts. Using this approach, the freedom from 100% occlusion at one year rate is an impressive 92.4%.1 This finding is highly encouraging and suggests that percutaneous bypass with the DETOUR System may offer a durable and effective treatment option for patients with complex PAD.
It is also worth noting that the clinical trial itself was somewhat limited and there was a considerable learning throughout the process. For example, some patients experienced slight proximal graft migration, particularly at the ostium of the SFA. By closely examining these occurrences and understanding their causes, the technique has been significantly improved. Enhanced precision in securing the ostial SFA has directly contributed to better patency rates and improved long-term durability.
From a safety standpoint, PTAB therapy with the DETOUR System offers clear advantages over traditional open bypass surgery. There are no major incisions or concerns about wound infections, as the procedure only requires the placement of an 8 Fr sheath in the contralateral femoral artery. The primary access-related risks are those typical of endovascular procedures, such as retroperitoneal bleed or hematoma formation.
The risk of DVT associated with this procedure is remarkably low, as I mentioned, approximately 2%,1 which is another reassuring aspect. One critical protective factor is ensuring the presence of a robust femoral vein. Specifically, we look for a femoral vein with a diameter of approximately 10 mm. The stents used in the DETOUR procedure generally measure around 6 mm to 6.7 mm in diameter. Therefore, if you have a vein that measures 10 mm in diameter, the stent occupies only about 50% of the vein’s lumen. Maintaining this ratio significantly reduces the risk of DVT. Overall, we have not encountered issues with DVT thus far and it has not been a concern in our practice.
Can you share a patient case where PTAB therapy was performed using the DETOUR System?
One of our early experiences involved a patient who had previously undergone bypass surgery in her left leg. The patient had a failed bypass in her left lower extremity, resulting in critical limb ischemia. Additionally, her right leg had a CTO of the SFA, but the ischemia was less severe, presenting as claudication rather than critical limb ischemia.
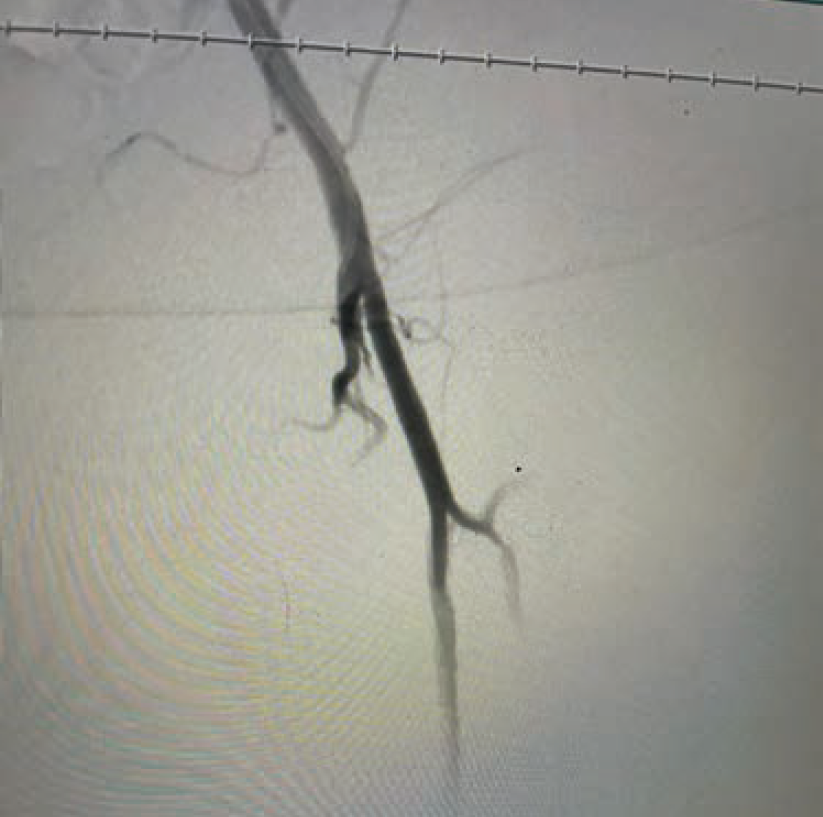
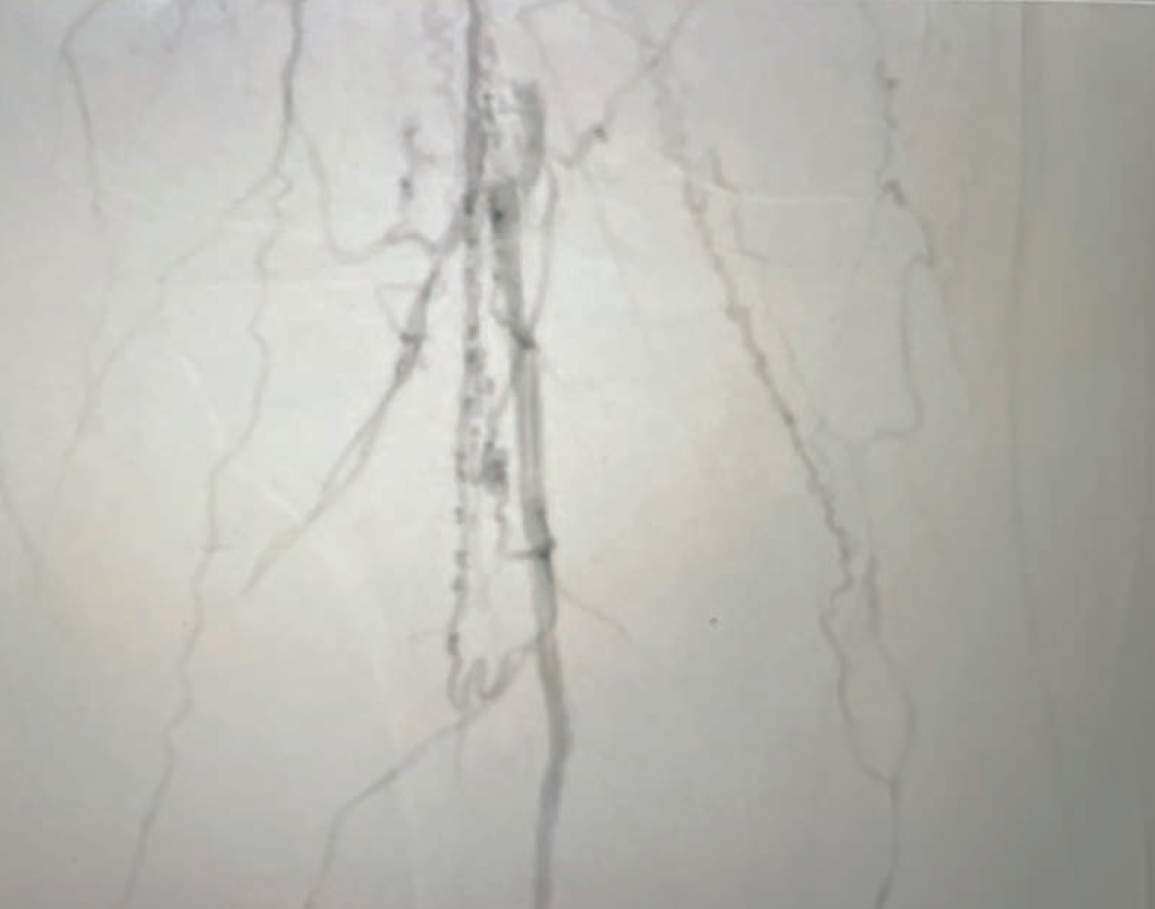
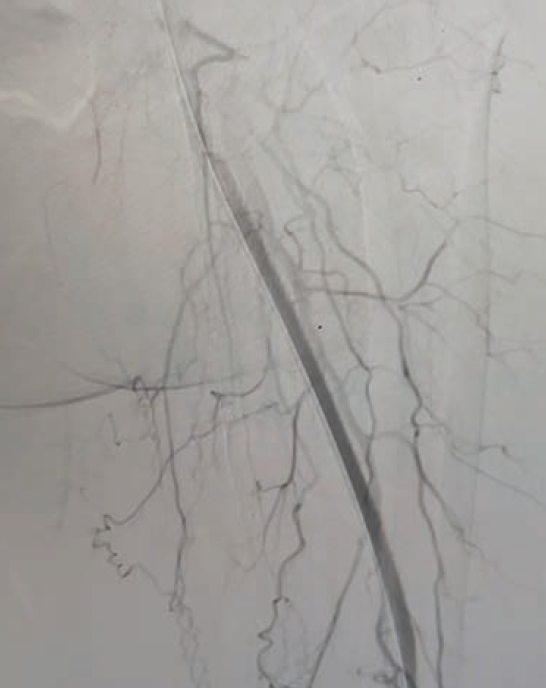
The procedure on her left leg took approximately 120 minutes, and she did exceptionally well (Figures 1A-D). The revascularization was successful and her left leg healed as expected. About a month later, she returned to us and, to our surprise, asked if we could perform the same procedure on her right leg. She was impressed by how much easier the percutaneous bypass was compared to her previous experience with open surgical bypass, which had been a challenging and difficult course for her.
We proceeded with the procedure on her right leg, and once again, the results were excellent. This case serves as a great example of how PTAB with the DETOUR System can effectively treat bilateral SFA disease, even when the severity of disease differs between the legs. One leg was treated for critical limb ischemia, while the contralateral leg was treated for claudication. Her follow-up appointments have shown remarkable results, with the patient very satisfied with her outcome, and she continues to do well.
What are the biggest challenges in getting more interventional cardiologists and vascular specialists to adopt PTAB, and how can these be addressed?
One of the primary challenges is that it is still a relatively new technology. Our center only began using it in October, so there is a natural learning curve associated with introducing something novel. The initial hesitation often stems from a lack of familiarity with the procedure, particularly the aspects of exiting and reentering the artery. Many physicians may feel uncomfortable with reentry devices such as the Pioneer or Outback systems, especially if they do not frequently use these tools in their practice.
Another challenge is building confidence in the safety and efficacy of the procedure. As physicians, our focus is always on whether a device is safe and whether it effectively improves patient outcomes. The available data, as well as my own clinical experience, support the conclusion that PTAB with the DETOUR System is both safe and effective. The key now is to communicate this evidence to other practitioners and demonstrate how this technology can enhance their ability to treat complex PAD patients. It’s helpful to draw comparisons to other minimally invasive technologies that have gradually gained acceptance, such as transcatheter aortic valve replacement or mitral valve repair procedures. Just as those devices have shifted the treatment paradigm away from open surgery toward less invasive approaches, PTAB offers a similar opportunity within the realm of endovascular therapy. This is important when considering the goals of reducing hospital length of stay, minimizing procedural complications, and ultimately improving patient outcomes.
As more experienced operators continue to demonstrate the safety and effectiveness of this technology, it will gradually gain wider acceptance. The key is to show clinicians how PTAB fits into their existing toolbox as a valuable option for high-risk patients, especially those who have exhausted surgical or endovascular options. The DETOUR System provides an effective and safe alternative for patients who previously had no viable options or who have experienced failures with previous interventions.
This interview is sponsored by Endologix.
Reference
1. Lyden SP. Percutaneous bypass for treatment of long-segment femoropopliteal disease: 12 month results from the DETOUR 2 trial. J Vasc Surg. 2022 Jun;75(6): e337-e338. https://www.jvascsurg.org/article/S0741-5214(22)01274-5/fulltext
Further reading
1. Krievins DK, Halena G, Scheinert D, et al. One-year results from the DETOUR I trial of the PQ Bypass DETOUR System for percutaneous femoropopliteal bypass. J Vasc Surg. 2020 Nov; 72(5): 1648-1658.e2. doi:10.1016/j.jvs.2020.02.043
2. Halena G, Krievins DK, Scheinert D, et al. Percutaneous femoropopliteal bypass: 2-year results of the DETOUR System. J Endovasc Ther. 2022 Feb; 29(1): 84-95. doi:10.1177/15266028211034862
3. Lyden SP, Soukas PA, De A, et al; DETOUR2 Trial Investigators. DETOUR2 trial outcomes demonstrate clinical utility of percutaneous transmural bypass for the treatment of long segment, complex femoropopliteal disease. J Vasc Surg. 2024 Jun; 79(6): 1420-1427.e2. doi:10.1016/j.jvs.2024.02.004
The DETOUR™️ System and associated components, ENDOCROSS™️ Device and TORUS™️ Stent Graft System, are not available in all countries or regions. Please contact your Endologix representative for details regarding product availability. Prior to use, refer to Instructions for Use for more information concerning Indications, Contraindications, Specific Anatomic Considerations, Warnings, Precautions, and Adverse Events. Rx only. ©2025 Endologix LLC. All rights reserved. MM2884-US Rev 01
Find More:
Cardiovascular Ambulatory Surgery Centers (ASCs) Topic Center
The Latest Clinical & Industry News
Grand Rounds With Morton Kern, MD
Peripheral Artery Disease Topic Center
Podcasts: Cath Lab Conversations
Go to Cath Lab Digest's current issue page
Go to the Journal of Invasive Cardiology issue page










