Computer-Assisted Vacuum Thrombectomy (CAVT) Designed for Quick, Safe, and Effective Clot Removal
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
CLD talks with:
Stanley K. Zimmerman, MD, FACC, FSCAI
Director, Catheterization Laboratory and Peripheral Vascular Services, Hillcrest Hospital South; Medical Director, Vascular Imaging Laboratory, Oklahoma Heart Institute, Tulsa, Oklahoma
 How do you determine which patients are candidates for mechanical thrombectomy versus thrombolysis?
How do you determine which patients are candidates for mechanical thrombectomy versus thrombolysis?
There are several factors that determine whether the patient is more appropriate candidate for lysis or mechanical thrombectomy, including the condition of the patient, their stability, and their overall risk for systemic lytics. We start by risk-stratifying all our patients on presentation, which is in line with the Pulmonary Embolism Response Team (PERT) Consortium. We use the European risk classes, which are intermediate-high, intermediate-low, high, and low-risk patients. The low-risk patients usually do not receive anything beyond medical management and many of the intermediate-low risk patients are also medically managed with anticoagulation. For intermediate-high risk, high-risk or massive PE patients, the devil is really in the details, because these distinctions can often blur.
Are there specific patient characteristics (eg, age, comorbidities, clot burden) that make you more or less likely to intervene with mechanical thrombectomy?
Clot burden doesn’t always tell the entire picture. Clot does tend to be the most prevalent measure because we can actually see it, but there tend to be other signs in blood chemistries and echocardiograms that offer a better sense of the potential for long-term ramifications from not treating.
Bicarbonate deterioration can be a very prevalent sign of impending problems or deterioration of the right ventricle. Some people use lactate, troponins or BNPs, but these tests are not at all specific for indicating the necessity for treatment.
In our process, we spend time evaluating and weighing all of these factors, and then looking at the patient and their overall condition. Are they symptomatic? Obviously when the patient has a massive pulmonary embolism (PE), they are very sick and you have to do something right away, which makes the choice of treatment much simpler. In older patients with a lot of comorbidities, significant PE can be completely detrimental to their overall health. These patients look sick right away, so details are often easier to tease out because there is no question about what is happening. Younger patients may have a greater reserve that is initially cushioning them, but they can reach that severity index very quickly once the right ventricle becomes completely dysfunctional. You may have a 30-year-old with a PE and they look okay, but all of a sudden a few hours later, they are coding.
Can you explain computer-assisted vacuum thrombectomy (CAVT)?
CAVT is a specific mechanical thrombectomy technology that uses computer algorithms to aid in clot detection and blood loss mitigation. It has evolved from what I would call early mechanical thrombectomy — using a big tube and suction where you just try to get everything out. CAVT is a more sophisticated, refined method of thrombectomy. I am seeing decreased blood loss and more efficient clot removal with CAVT, which can detect whether there is thrombus engaged with the catheter.
Can you explain the CAVT user interface?
There are both visual and audio cues. Using CAVT has become second nature. I am not necessarily standing there watching the clot go in, but moving the catheter and feeling the tactile response. When you do enough of these procedures, you can tell by feel when the catheter has been cleared of clot and it is reinforced with audio feedback from the device.
How does CAVT affect procedure time?
The more familiar you become with the equipment and the technology, and adept at the skillset, the shorter the procedure. Stick to close, my CAVT procedures may now run 20 to 30 minutes. That is a big difference from infusion catheter therapy where you are putting in lytics for four hours.
Can you share more about your standardized protocol?
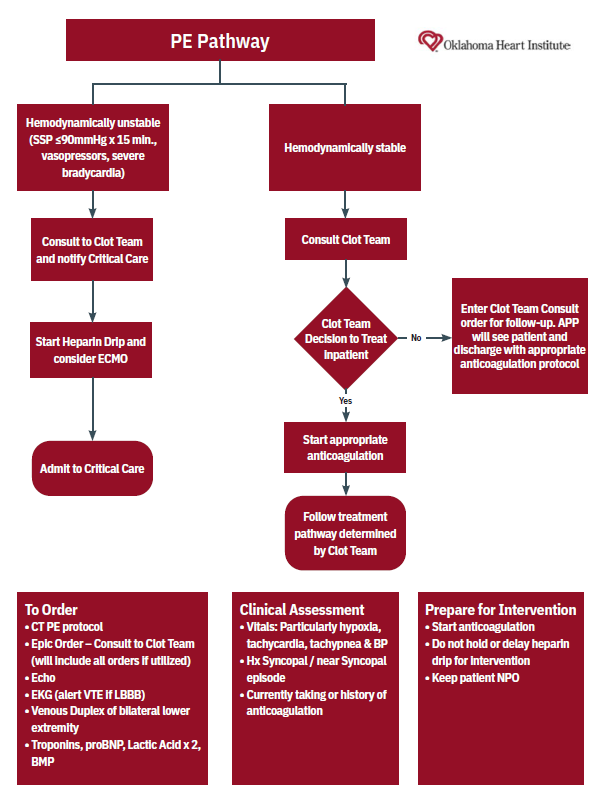
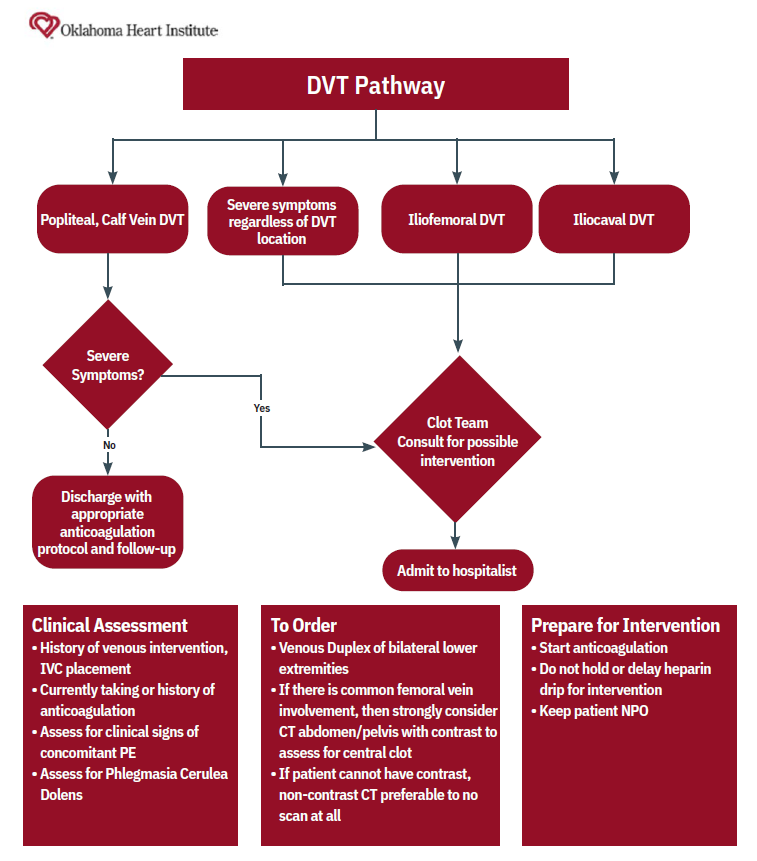
We have been able to standardize our practice and treatment algorithms (Figures 1-2), which makes it easier and simpler to find a way forward when we do have outliers. That process goes forward as a joint venture between our Clot Team and the referring physician. The Clot Team encompasses the evaluation and treatment of all clots. The team is made up of five physicians with 24/7 coverage of all regional hospitals. The referring doctor, typically an emergency department doctor or hospitalist, contacts us to initiate the process, whether it is a challenging case or a quick question.
If you have someone who is stable on medical therapy, how do you make the decision to escalate to intervention?
As a cardiologist, I am used to randomized, controlled trials for almost every single thing I do, but how do you start randomization when so many of us on the front lines have seen the dramatic benefits from thrombectomy? Anecdotally, we can say yes, but it would be nice to have some hard data. Several studies are underway, including STORM-PE, which is evaluating CAVT with anticoagulation vs. anticoagulation alone.1 With the data from these studies, we might be able to determine if there is a benefit in treating certain intermediate risk patients that we are not currently treating with thrombectomy.
Historically, we have spent decades not doing anything for many of these patients and found out the hard way that the chronic thromboembolic pulmonary disease process is difficult to manage. These are tough patients with progressive shortness of breath and they are hard to treat. We have new medications, but chronic thromboembolic pulmonary disease is still something that we would prefer to avoid for our patients.
What are the key factors that influence your choice of thrombectomy device for a given PE case?
Mechanical thrombectomy is something that we see works and it is relatively safe. At least in our practice, it has led to us using more mechanical devices. In 2020, during Covid, we were inundated with venous thromboembolism patients and the ICUs were busy. The idea of putting an otherwise healthy patient in the ICU with catheters in their neck because they couldn’t go anywhere else didn’t make sense, so we started using more thrombectomy devices. Currently in our hospital system, the majority of our strategy is for catheter-based mechanical thrombectomy. We don’t really use a lot of lytic drip catheters anymore. If we are using thrombolytics, it tends to be more for systemic purposes rather than an infusion for the high-risk patients.
How do you measure procedural success beyond just clot removal — are there specific short- or long-term markers you track?
We register and internally follow all our patients through to 90-day echo assessment, and we use a modified version of the Kansas City Cardiomyopathy Questionnaire (KCCQ) quality of life score in our follow-up. It is also important to talk to the patient and get some sense of how they feel subjectively 24 hours later and 3 months later. The Clot Team has monthly meetings and we evaluate our data. We initially had a heparin-based protocol for all our clots, but switched to an enoxaparin-based protocol after reviewing data, talking to other physicians, and finding out what other centers are doing. It is a large, collaborative effort. The outcomes piece is huge.
What is the makeup of your Clot Team from a specialty perspective?
We have one vascular surgeon and the other four are interventional cardiologists. We do not have a large interventional radiology presence where we practice. The vascular surgeon is one of my partners. We work in the same department of vascular services, which is unique. We found pretty quickly that we needed that collaboration to be successful. We also have a large extracorporeal membrane oxygenation (ECMO) program with our own cardiac critical intensivists. We work closely with them on patients who may have a high deterioration factor and have ECMO as a backup if needed.
What advice would you give to interventionalists who are just starting to incorporate PE thrombectomy into their practice?
You need significant help from clinical staff. The idea that you can just do a thrombectomy and be done is shortsighted. The real reason we are doing this procedure is for long-term patient improvement in health, which necessitates having a team-based approach in place. Sometimes people only think about the procedure, which, yes, is a major portion, but they don’t think about all the rest. That would be my advice: think about all the rest.
This interview is sponsored by Penumbra, Inc.
Reference
1. STORM-PE Trial. https://www.penumbrainc.com/storm-pe-trial/
Dr. Stanley Zimmerman is a consultant for Penumbra, Inc.
Procedural and operative techniques and considerations are illustrative examples from physician experience. Penumbra does not endorse any triage or treatment protocols. Physicians and hospitals must use their medical judgment when selecting triage and treatment protocols and Penumbra disclaims liability or responsibility for the results or consequences of any actions taken in reliance on information in this article. Physicians’ treatment and technique decisions will vary based on their medical judgment. The clinical results presented herein are for informational purposes only and may not be predictive for all patients. Individual results may vary depending on patient-specific attributes and other factors.
Caution: Federal (USA) law restrictions these devices to sale by or on the order of a physician. Prior to use, please refer to the Instructions for Use for complete product indications, contraindications, warnings, precautions, potential adverse events, and detailed instructions for use. Please visit www.peninfo.inc/risk for the complete IFU Summary Statements. Please contact your local Penumbra representative for more information.
Find More:
Cardiovascular Ambulatory Surgery Centers (ASCs) Topic Center
The Latest Clinical & Industry News
Grand Rounds With Morton Kern, MD
Peripheral Artery Disease Topic Center
Podcasts: Cath Lab Conversations










