Preventing Radiation Injury
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Morton J. Kern, MD, MSCAI, FACC, FAHA
Clinical Editor; Interventional Cardiologist, Long Beach VA Medical Center, Long Beach, California; Professor of
Medicine, University of California, Irvine Medical Center, Orange, California
Disclosures: Dr. Morton Kern reports he is a consultant for Abiomed, Abbott Vascular, Philips, ACIST Medical, and Opsens Inc.
Dr. Kern can be contacted at mortonkern2007@gmail.com
On X @MortonKern
Every year, new operators, mostly trainees, start working in our cath lab. As part of our annual continuing quality improvement programs and required education, we received an update on national guidance for preventing and managing radiation injury to patients undergoing fluoroscopic procedures. It behooves all working in a radiation environment to recall that cath lab procedures have become more complex and that for coronary, structural, and electrophysiology studies, there is increased radiation exposure to both patients and operators.
By design, the cath lab must use radiation to acquire our diagnostic information and guide the therapeutic tools to produce clinical benefits. It is our hope that the safest use of radiation is our standard of care. To prevent radiation injury, both vigilance and adaptability from cath lab professionals are required. This work carries inherent risks of injury related to ergonomics (managing lead aprons and working positions) as well as radiation exposure and its related medical consequences.
To reduce exposure risk, the cath lab team should build a radiation risk-aware culture that includes regular training, strict adherence to safety guidelines, and the continual assessment of new protective equipment. These actions should be incorporated into the lab routine. Documentation and auditing of cumulative doses provide feedback and allows for ongoing optimization of our actions. Advances in hardware, technology and physician and nurse-driven safety protocols have reduced exposure for both patients and medical staff. Most recently, the introduction of some novel x-ray shielding systems permits operators to do away with heavy lead personal protective aprons.1 However, the patient is still subjected to the routine exposures as discussed below.
As a basic best practice, physicians have applied the dictum for radiation exposure of “as low as reasonably achievable” (ALARA). In the current era, this probably should be restated “as close to zero as possible” (ACZAP), something that can now be achieved using novel radiation protection systems.2 However, the patients are still exposed to the radiation needed to complete the procedure and while the operators may not be exposed to radiation, patients are always at risk.
How Much Radiation is Associated With Cardiac Cath Lab Procedures?
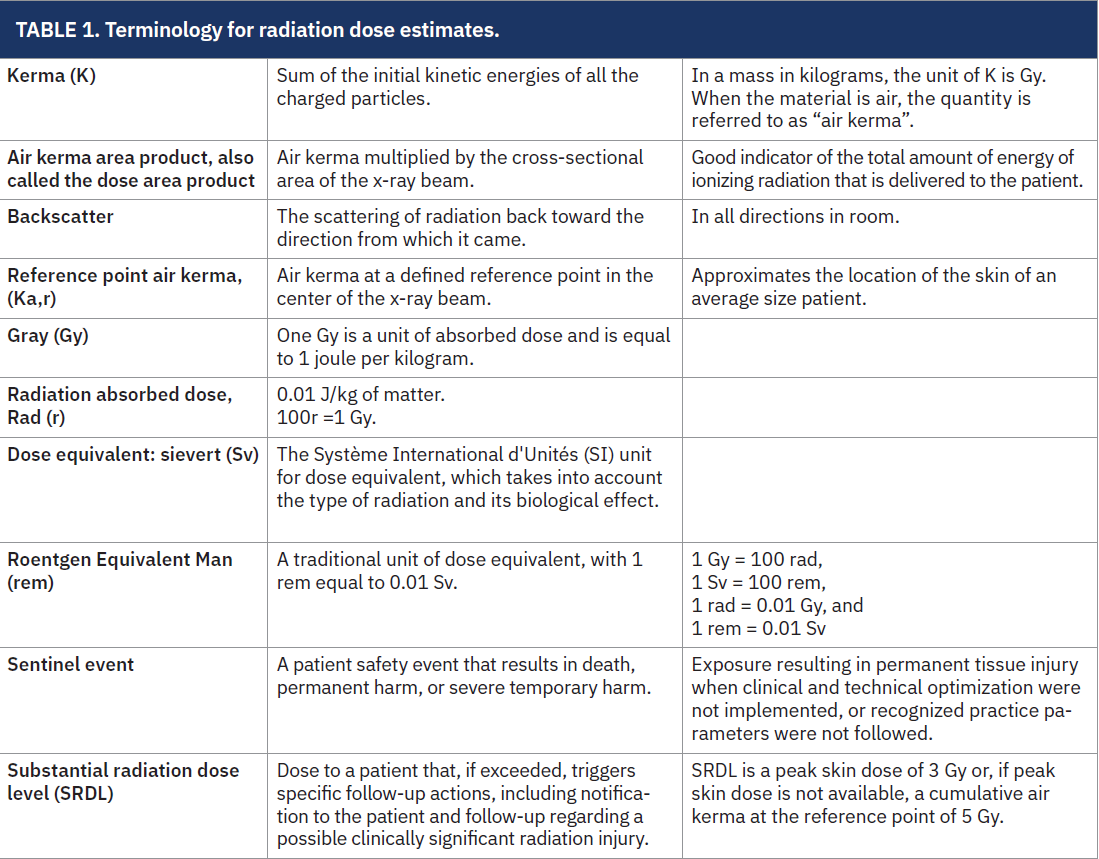
The exact amount of radiation exposure in an x-ray procedure varies depending on the part of the body receiving the x-ray and the procedure requirements. Table 1 provides a list of some common terms for radiation measurements. For a comparison, the average annual radiation dose from natural background sources is 3.0 mSv (300 mrem). A single chest x-ray: 0.02 mSv (2 mrem), dental x-ray (four bitewings): 0.004 mSv (0.4 mrem), limbs and joints: 0.06 mSv (6 mrem), abdomen: 0.7 mSv (70 mrem), mammogram (four images): 0.13 mSv (13 mrem).3
Computed tomography (CT) scans have replaced routine some chest x-rays. Approximate exposures for CT scans3 are listed below:
• Head CT: 2.0 mSv (200 mrem)
• Chest CT: 8.0 mSv (800 mrem)
• Abdomen CT: 10 mSv (1,000 mrem)
• Pelvis CT: 10 mSv (1,000 mrem)
An interventional coronary diagnostic study or percutaneous coronary intervention (PCI) procedure may expose the patient to the radiation equivalent of 75-3,000 chest x-rays.3 For invasive cardiology procedures, approximate exposures are:
• Coronary angiogram: 4.6-15.8 mSv (460-1,580 mrem);
• PCI: 7.5-57 mSv (750-5,700 mrem).3
What Are the Exposure Limits for Radiation in the Workplace?
There is no set limit for radiation exposure that is considered too much, requiring that we balance the risk vs benefit in acquiring information about the patient’s condition.
The specific exposure limits4 that the U.S. Occupational Safety and Health Administration (OSHA) has set for radiation in the workplace under 29 CFR 1910.1096 are:
• Whole-body exposure: The limit is 1.25 rem (12.5 mSv) per calendar quarter for the whole body, including the head and trunk, active blood-forming organs, the lens of the eyes, and the gonads.
• Extremities: For hands, forearms, feet, and ankles, the limit is 18.75 rem (187.5 mSv) per calendar quarter.
• Skin exposure: The limit for the skin on the whole body is 7.5 rem (75 mSv) per calendar quarter.
Based on OSHA’s radiation standards, the annual dose limit for radiation workers in mSv is 50 (5 rem) for the whole body. Additionally, OSHA’s annual limit for extremities is 750 mSv (75 rem), and the annual limit for skin exposure is 300 mSv (30 rem). OSHA’s standard is different from the International Commission on Radiological Protection (ICRP), which recommends an occupational exposure limit of 20 mSv per year, averaged over five years, with no year exceeding 50 mSv.5 Since the ICRP sets its average annual limit lower than OSHA, healthcare facilities may want to consider setting their standards under the OSHA 50 mSv annual standard for the whole body to keep staff members safe.
How Do We Gauge Radiation-Associated Tissue Injury?
Radiation injures biologic tissues by breaking connecting bonds and causing cell death. The tissue reactions occur from 2 major mechanisms:
1) Deterministic effects, which are tissue reactions with dose thresholds that, when exceeded, can cause observable effects like skin reddening (erythema), blistering, and hair loss.
2) Stochastic effects, which are long-term effects such as an increased risk of cancer that are associated with radiation exposure, though the risk is generally low for most procedures.
To determine if there is radiation-induced tissue damage, several methods and indicators are used. Dosimetry is the primary method for assessing radiation exposure and its effects. Dosimetry calculates the amount of radiation energy absorbed by the tissues. The immediate symptoms of radiation injury can include skin burns, vomiting, hair loss, and changes in blood cell counts. Long-term effects may include cancer and genetic mutations. Large doses of ionizing radiation can cause acute illness by reducing blood cell production and damaging the digestive tract.
What Are the Clinical Follow-Up Requirements Needed If Radiation Guidelines Are Exceeded?
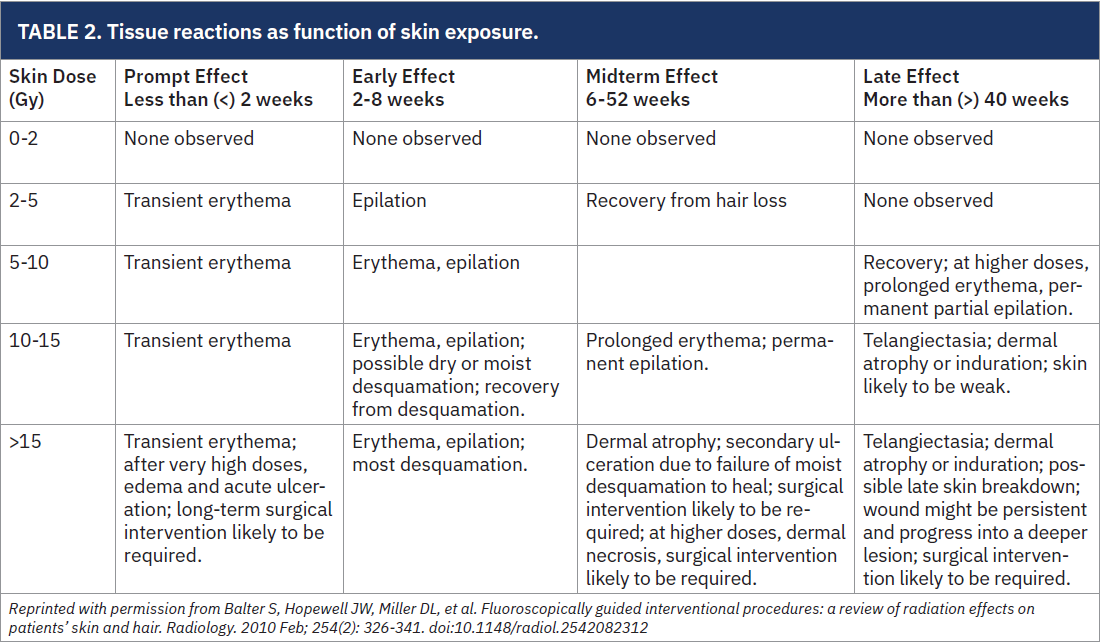
Table 2 describes tissue reactions as function of skin exposure.6 If an estimated peak skin dose has exceeded the Substantial Radiation Dose Level (SRDL), several steps should be considered. For skin doses of 2-5 gray (Gy), some patients may experience transient erythema or transient epilation within weeks. These injuries will typically not need follow-up or medical intervention. A discussion with the patient should address the possible skin effects and the expected location and duration.
For peak skin doses between 2 and 3 Gy, the patient should be instructed to report the development of any skin reaction to the exposed area. This discussion should be documented in the health electronic record.
For peak skin doses between 3 and 5 Gy, a follow-up assessment must be performed to look for potential skin issues. In general, the assessment may be conducted face to face, via telehealth, or by telephone.
For peak skin doses in the range of 5-15 Gy, the patient may complain of itching, partial or permanent epilation and prolonged erythema, and ultimately, skin telangiectasia and atrophy. For doses in this range, the physician must counsel the patient and set a follow-up examination approximately 4 to 8 weeks post procedure.
For skin doses >15 Gy, the most clinically significant long-term effect is ischemia with persistent ulceration and infection. Such injuries often will need full-thickness skin grafting. These patients will demonstrate dry or moist peeling of the skin about 4-8 weeks after the procedure. Provisions must be made for follow-up and monitoring of patients who potentially may have clinically significant long-term radiation effects on the skin and subcutaneous tissues.
From Tamirisa KP, Alasnag M, Calvert P, et al; ACC Women in Cardiology Advocacy Work Group. Radiation exposure, training, and safety in cardiology. JACC Adv. 2024 Feb 29; 3(4): 100863. doi:10.1016/j.jacadv.2024.100863
Copyright © 2024, The Authors. Published by Elsevier on Behalf of The American College of Cardiology Foundation. This is an Open Access Article under the CC BY License (http://creativecommons.org/licenses/by/4.0/).
How Do We Estimate Skin Dose?
Currently, there are no technical means to precisely calculate the dose at the skin site that receives the highest exposure. Some newer fluoroscopes display an estimate of peak skin dose. The cumulative air kerma commonly overestimates peak skin dose and is known to be a rough estimate (Table 2 provides definitions of terms regarding radiation measurements6).
Further complicating the estimate of skin dose is the use of multiple x-ray beam angles, which cause radiation to be distributed over multiple skin entry sites. The possibility of the overlapping of two separate adjacent fluoroscopic fields, where skin dose of the overlapping area may receive the sum of the doses of the projections, must be considered.
Assume peak skin dose is reasonably represented by the displayed cumulative air kerma. For a highly conservative calculation, peak skin dose can be estimated as 1.4 times the actual cumulative air kerma (AK) of the most-exposed skin.6
The Bottom Line
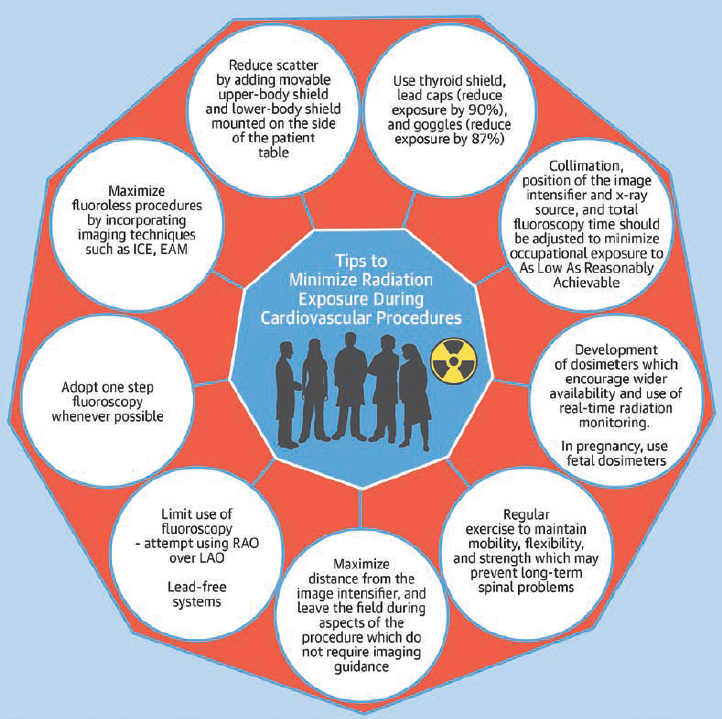
Radiation exposure, training, and safety in cardiology are increasingly relevant today due to the range of catheterization lab procedures and exposure to radiation from invasive and non-invasive imaging (nuclear) procedures.7 Figure 1 lists several helpful tips on reducing radiation exposure.7 Reviewing the safety protocols, integrity of lead aprons, and installation of novel protective shielding will reduce the team’s exposure and make for a safer working environment. For those new to the cath lab, let’s share the knowledge.
References
1. Roguin A, Wu P, Cohoon T, Gul F, Nasr G, Premyodhin N, Kern MJ. Update on radiation safety in the cath lab - moving toward a “lead-free” environment. J Soc Cardiovasc Angiogr Interv. 2023 Jun 2; 2(4): 101040. doi:10.1016/j.jscai.2023.101040
2. Writing Committee Members; Hirshfeld JW Jr, Ferrari VA, Bengel FM, et al; ACC Task Force on Expert Consensus Decision Pathways; Januzzi JL Jr, Afonso LC, Everett B, et al. 2018 ACC/HRS/NASCI/SCAI/SCCT Expert Consensus Document on Optimal Use of Ionizing Radiation in Cardiovascular Imaging-Best Practices for Safety and Effectiveness, Part 1: Radiation Physics and Radiation Biology: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways Developed in Collaboration With Mended Hearts. Catheter Cardiovasc Interv. 2018 Aug 1; 92(2): 203-221. doi:10.1002/ccd.27660
3. Ionizing Radiation Exposure of the Population of the United States. National Council on Radiation Protection & Measurements (NCRP), Report No. 160. Accessed August 18, 2025. https://ncrponline.org/publications/reports/ncrp-report-160/
4. 1910.1096 - Ionizing radiation. Occupational Safety and Health Administration (OSHA). U.S. Department of Labor. Accessed August 18, 2025. https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.1096
5. International Commission on Radiological Protection (ICRP). Accessed August 18, 2025. https://www.icrp.org/
6. Balter S, Hopewell JW, Miller DL, et al. Fluoroscopically guided interventional procedures: a review of radiation effects on patients’ skin and hair. Radiology. 2010 Feb; 254(2): 326-341. doi:10.1148/radiol.2542082312
7. Tamirisa KP, Alasnag M, Calvert P, et al; ACC Women in Cardiology Advocacy Work Group. Radiation exposure, training, and safety in cardiology. JACC Adv. 2024 Feb 29; 3(4): 100863. doi:10.1016/j.jacadv.2024.100863










