Feedback Reports for Improving STEMI Care
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Daniel Moore, RN, BSN, CEN
STEMI Program Nurse Coordinator; RN, Cardiovascular Recovery Unit (CVR),
Asante Rogue Regional Medical Center, Medford, Oregon
Daniel Moore, RN, BSN, CEN, can be contacted at daniel.moore@asante.org

1st row: Daniel Moore, RN, STEMI Program Nurse Coordinator
2nd row: Dr. Kent Dauterman & Dr. Brian Gross, STEMI Program Co-Directors
3rd row: Buck Sarver & Carl Cox, Cath Lab Technologists
4th row: Colin Olson, Cath Lab Manager; Lindsy Gollihar, Cath Lab RN; Sarah Carlyle, DNP, Cardiac Educator, Nursing Professional Development
As a bedside and charge RN working in the emergency department (ED), I spent the first 10 years of my career identifying, caring for, and rushing many STEMI patients to the cath lab. I was directly involved in creating shorter ED dwell times when I saw a new opportunity arise — a ST-elevation myocardial infarction (STEMI) Program Nurse Coordinator position became available in December 2015. I was ready to expand my practice and was fortunate to be selected. Today, I work in both STEMI and cardiovascular recovery roles: I also hold a part-time position in our cardiovascular recovery unit (CVR). I’m proud to say I have never left the bedside in my 20 years as an RN.
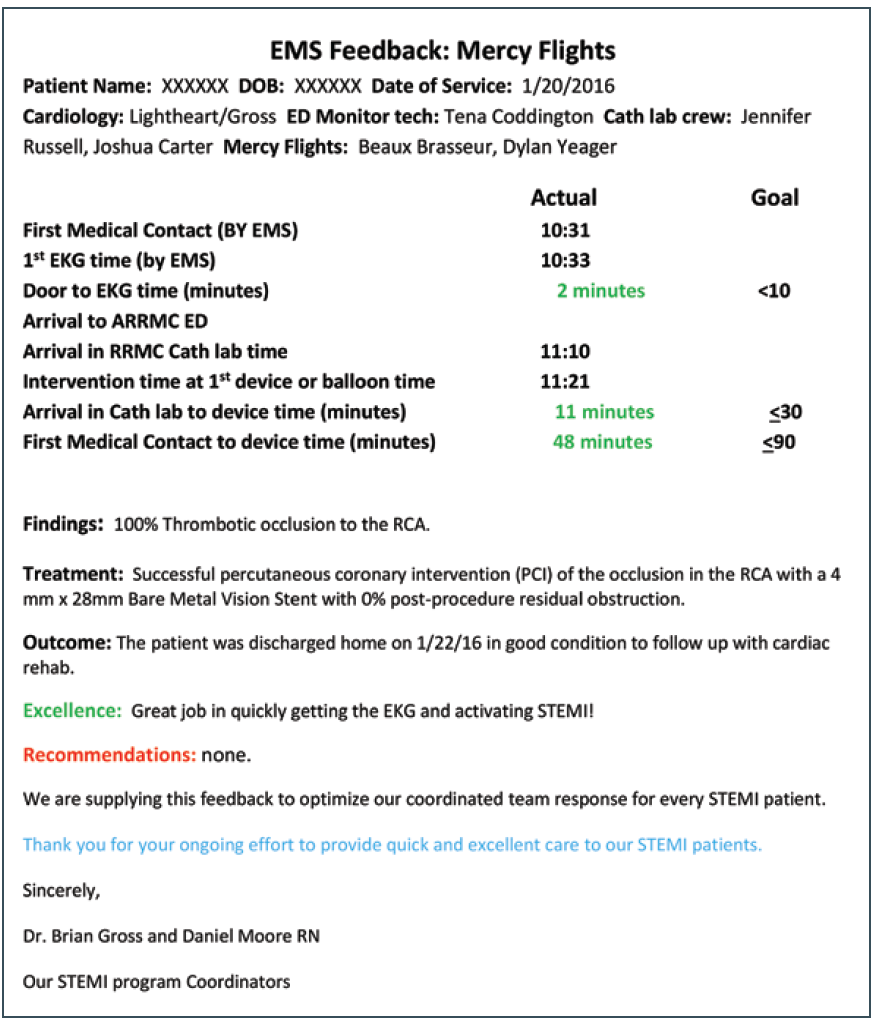
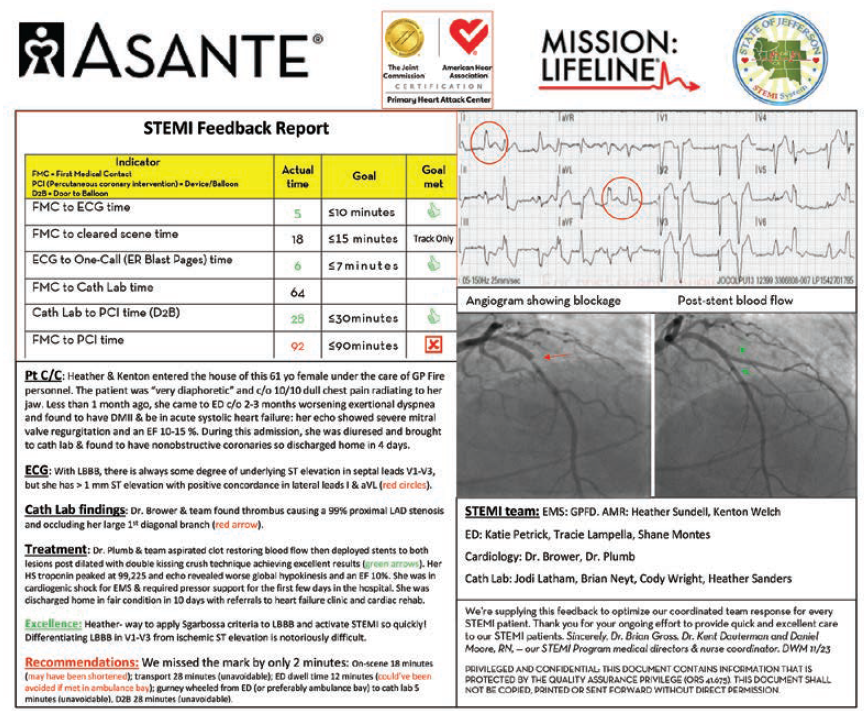
Early on in my STEMI coordinator role, I saw the previous coordinator’s STEMI feedback reports that went to the care team (Figure 1 is an original feedback report I inherited, dated 1-20-16). Fortunately, this coincided with our institution, Asante Rogue Regional Medical Center in Medford, Oregon, acquiring a more user-friendly visual angiogram-recording program by McKesson. It offered the opportunity to provide better visual aids, along with adding the STEMI electrocardiogram (ECG), as reinforcement tools for meeting time goals, teaching opportunities, and to scratch the curiosity itch of the patient outcome. Collaborating with my outstanding medical co-directors, I bounced formatting and content ideas off of them along with researching how other STEMI coordinators provide feedback. Our feedback reports have evolved since 2016 to their current form (examples provided below).
We send these feedback reports to every team member who comes into contact with a STEMI patient, primarily from first medical contact through the cath lab (whether ED or EMS activated). For patients that go for emergent coronary artery bypass graft (CABG) surgery or have a different path post-cath lab, we send the reports to the OR, cardiovascular intensive care unit (CVICU), and Heart Center personnel through discharge. These feedback reports have patient information de-identified to be compliant with HIPAA; they are titled only with a date for our own tracking and filing purposes.
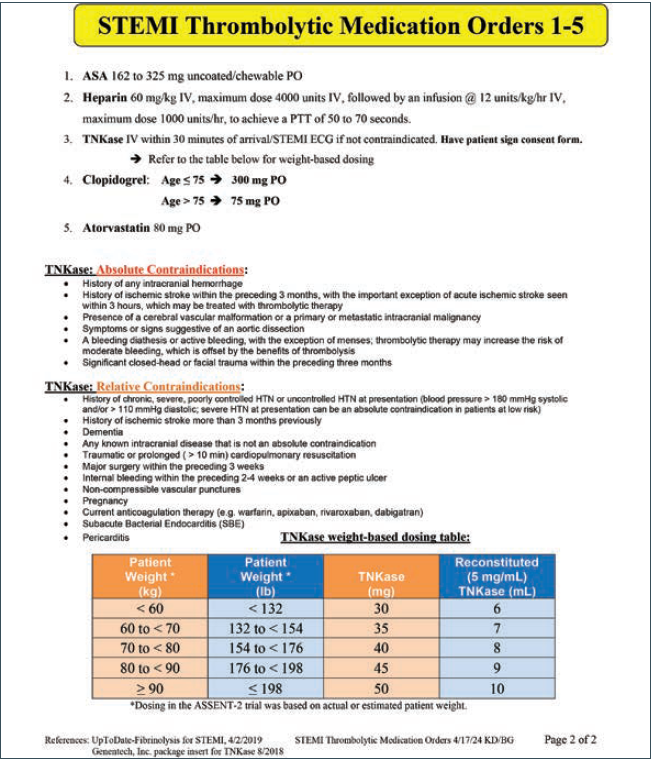
For our four outlying hospitals that are >2 hours away and offer thrombolysis and transfer, our feedback reports focus on the time goals of Door to EKG and Door to Needle (thrombolysis). We also confirm outlying hospital team members administered additional recommended STEMI medications (ASA, heparin, clopidogrel, atorvastatin), and if not, we offer gentle encouragement to refer to their laminated protocol (Figure 2 is our STEMI medications protocol for outlying hospitals that give thrombolysis and we make sure this protocol sheet is available for them).
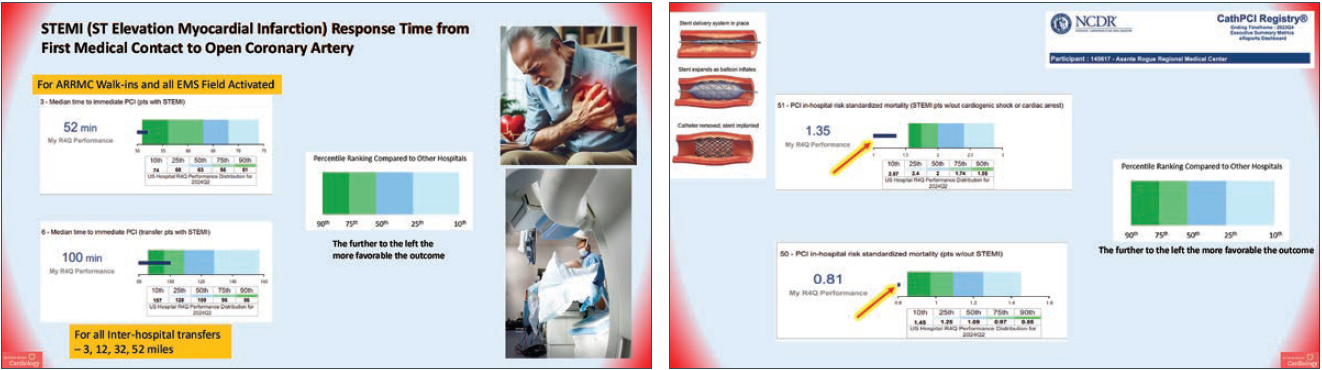
An approach of timely, consistent feedback to patient care personnel fosters team engagement, helping to facilitate great patient outcomes. This is evident in our four consecutive years of achieving American College of Cardiology National Cardiovascular Data Registry (ACC NCDR) Chest Pain Myocardial Infarction (CPMI) Platinum level, with many years of gold and silver level beforehand (our associated NCDR data can be seen in Figure 3), as well as receiving gold for STEMI and non-STEMI from American Heart Association (AHA) Mission: Lifeline STEMI nearly all of the last 8 years. We meet regularly with ED and EMS personnel to greet new people in critical roles and collaborate on new evidence to update our practices. Annually we hold a combined meeting that includes each ED and their primary EMS agency within our primary percutaneous coronary intervention (PPCI) area, sharing the previous years’ data in order to look for trends and opportunities. This approach has created a positive practice environment for patient care staff, who have regularly expressed appreciation for the education and feedback from the STEMI medical co-directors and STEMI coordinator.
Asante Rogue Regional Medical Center had 369 total STEMI activations in 2023 and >400 STEMI activations in 2024. Of the 369 STEMI activations in 2023, 332 were from our PPCI area and 37 from our four outlying hospitals. Out of the 369, 171 underwent PCI, 30 had a CAGB, and 21 were medially managed. The remainder were not STEMI diagnoses. Examples of the feedback reports are below:
2/15/24: This feedback report focused on opportunities for improvement and showed how minutes at each element contributed to the final outcome — in this case, a 2-minute delay led to a failure to meet the 90-minute overall metric (Figure 4 is an EMS feedback report with opportunity for improvement).
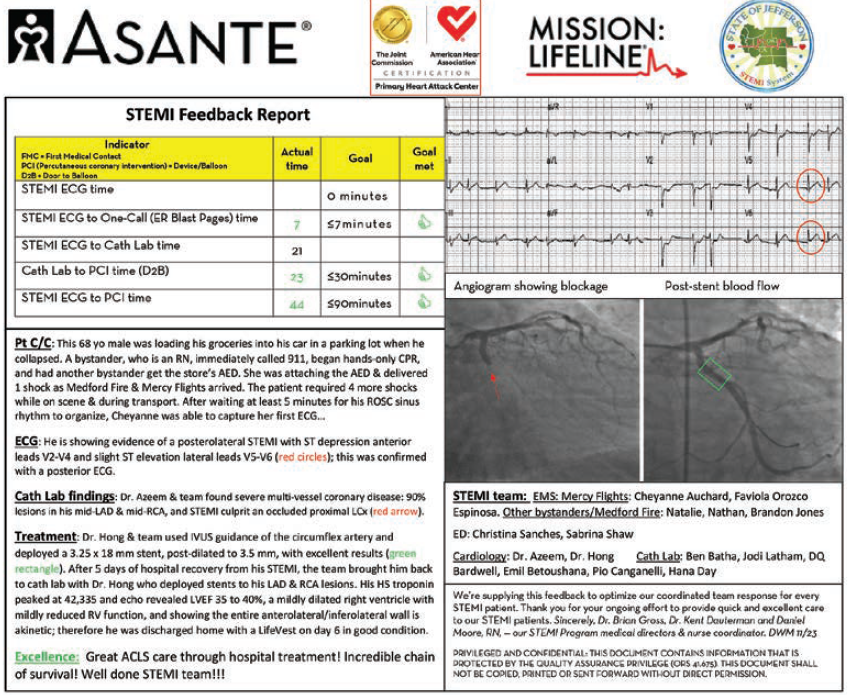
5/3/24: This feedback report focused on the importance of high-quality CPR and early defibrillation with out-of-hospital cardiac arrest (OHCA). This was critical to bypass the ED for stabilization direct to cath lab and onto an incredible door-to-ballon (D2B) time with intact neurological outcome for the patient (Figure 5 is a cardiac arrest in the field, STEMI after return of spontaneous circulation [ROSC], resuscitated with a good outcome).
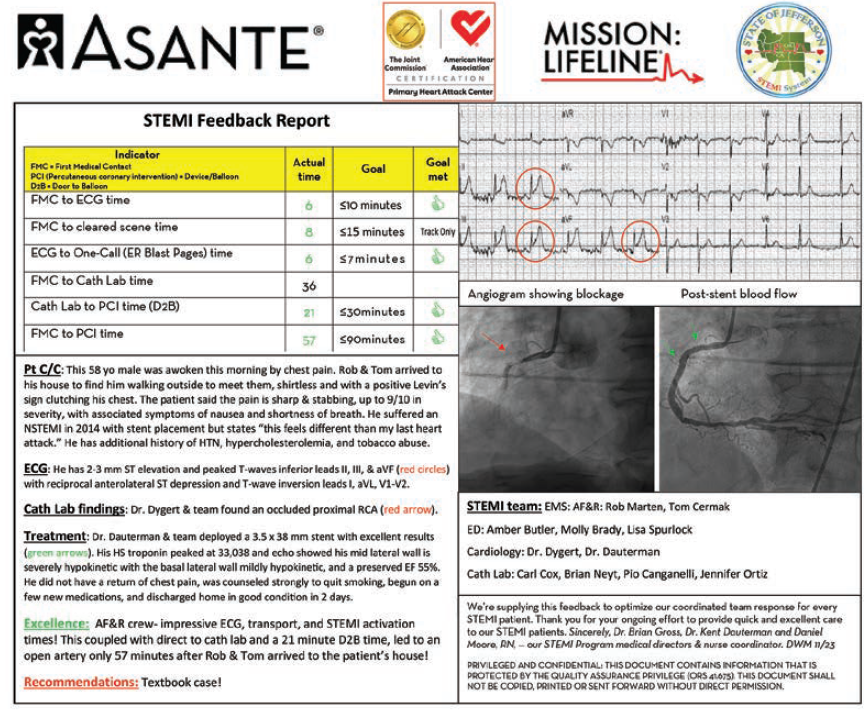
9/3/24: This feedback report focused on the rapid EMS times with early STEMI activation. With only a 22-minute drive to cath lab door, the early page gave the cath team time to get ready so the patient could bypass the ED and go directly to cath lab. These fast times across the board led to our STEMI patient average 2-day hospitalization and in this case, with minimum infarction time (high-sensitivity troponin only to 30k and ejection fraction 55% with a 100% occlusion) (Figure 6 is an EMS feedback report where the team made every time goal).
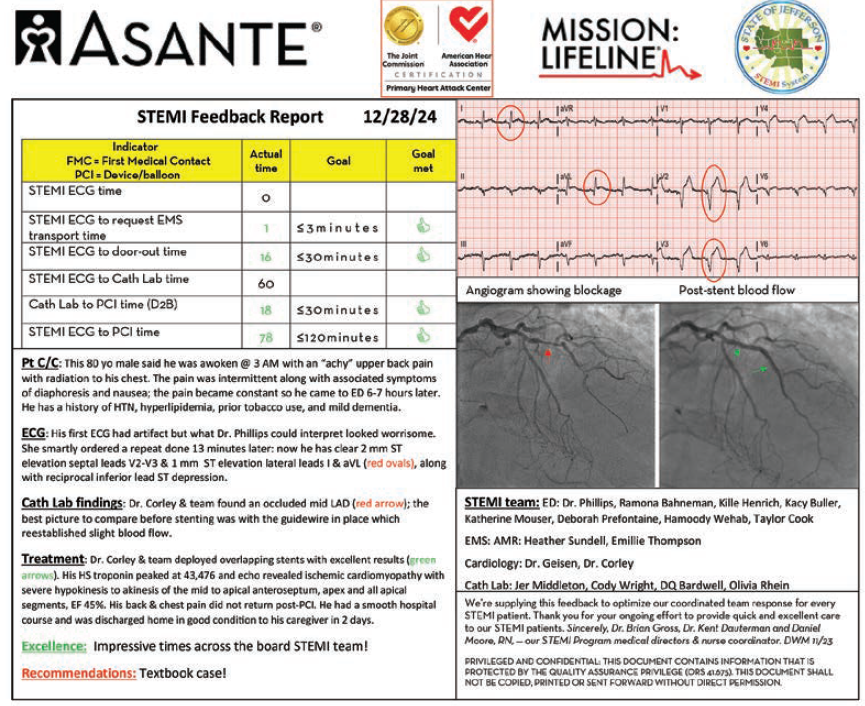
12/28/24: This feedback report highlights the large size of our STEMI system of care, with a 63.5-mile transport. This EMS crew bypassed one of our referral hospitals because they know their protocol so well. This female patient with many co-morbidities arrived in cardiogenic shock and the STEMI team stabilized her quickly, intervened on her right coronary artery, addressed her several other medical and social needs, and still had her discharged home in 2 days (Figure 7 is a feedback report where EMS knew to bypass a non-PCI capable hospital).
Conclusion and Summary
Our consistent and timely feedback to direct-care and leadership staff who take care of our shared STEMI patients has been an effective strategy to consistently achieve the safe patient journeys and great outcomes within our STEMI system of care. I encourage other STEMI system stakeholders to implement similar feedback reports, and hold regular meetings with EMS and hospital clinical staff to educate, increase engagement, and deliver better patient outcomes.
Acknowledgments. I would like to acknowledge Brian W. Gross, MD, FACC, FAHA, and Kent W. Dauterman, MD, FACC, FSCAI, Co-Directors, STEMI System of Care, Asante Rogue Regional Medical Center, for their encouragement and support in writing this article.
Reference
1. NCDR CathPCI Registry, Ending Timeframe: 2024Q2, Executive Summary Metrics. Participant: 145617 – Asante Rogue Regional Medical Center










