When the Guard Gets You With Friendly Fire: Filter Choking and De-Choking During High Plaque Burden Carotid Artery Stenting
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Muhammad Anjum, MBBS, FRCP, FSCAI, FCPS (C), FCPS(IVC); Jalaludin, MBBS, FCPS; Shahid Hameed, MBBS, MRCP; Imran Abid, MBBS, FCPS; Ahmad Noeman, MBBS, FCPS; Muzaffar Ali, MBBS, FCPS
Punjab Institute of Cardiology, Lahore, Pakistan
Disclosures: The authors report no conflict of interest regarding the content herein.
The authors can be contacted via Muhammad Anjum, MBBS, FRCP, FSCAI, FCPS(C), FCPS(IVC), at anjum_nish@yahoo.com.
Abstract
Background: Carotid artery stenosis is a prevalent vascular condition that increases the risk of stroke, particularly in patients with multivessel coronary artery disease. In those undergoing coronary artery bypass grafting (CABG), significant carotid disease elevates cerebrovascular risk and complicates management. Carotid artery stenting is a viable alternative to endarterectomy, provided the operator is proficient in technique and complication management.
Case Presentation: A 70-year-old hypertensive male with NSTEMI underwent coronary angiography, revealing triple-vessel disease sparing the left main. During pre-CABG workup, he was found to have a prior transient ischemic attack and a 95% stenosis of the right internal carotid artery. The heart team recommended carotid revascularization prior to surgery due to intermediate coronary risk and neurological history.
Procedural Complication and Management: Right carotid access was obtained with a 7F multipurpose guide. A FilterWire EZ was deployed distally, followed by placement of a 6 mm × 40 mm self-expanding stent at the internal carotid ostium. Post-deployment angiography revealed no distal flow, despite correct stent position and no thrombus or dissection, suggesting filter occlusion from embolic debris. The patient developed transient neurologic symptoms. Airway support was initiated, and an Export catheter was used for aspiration. Intra-arterial nitrate and tirofiban restored flow and resolved symptoms. Post-dilation with a 4.5 mm non-compliant balloon yielded excellent final angiographic results.
Conclusion: Carotid stenting remains a safe, effective alternative to endarterectomy. Although complications are rare, operator vigilance and readiness for prompt management are essential to procedural success.
Cerebrovascular disease is a leading cause of death and a leading cause of permanent neurological damage and physical disability. A significant atherosclerotic lesion of the internal carotid artery is a risk factor for stroke, accounting for 10–20% of all ischemic strokes or transient ischemic attacks (TIA).1 Symptomatic carotid artery disease is defined as the presence of cerebral symptoms associated with ipsilateral carotid lesions. The presence of concomitant carotid vascular disease can be a confounding factor in patients with complex coronary arterial disease undergoing coronary artery bypass graft surgery (CABG). Carotid artery stenting (CAS) has emerged as an alternative option to carotid endarterectomy (CEA), and has gained in use due to its minimally invasive nature and potential advantages in high-risk patients.2,3 The goal of carotid intervention is to prevent stroke.
Case Presentation
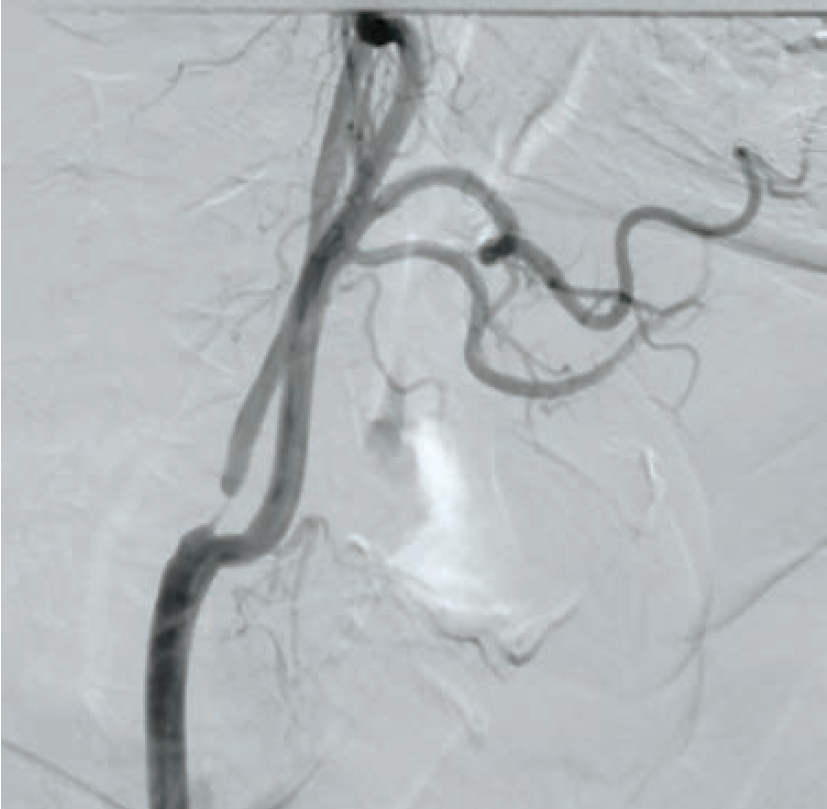
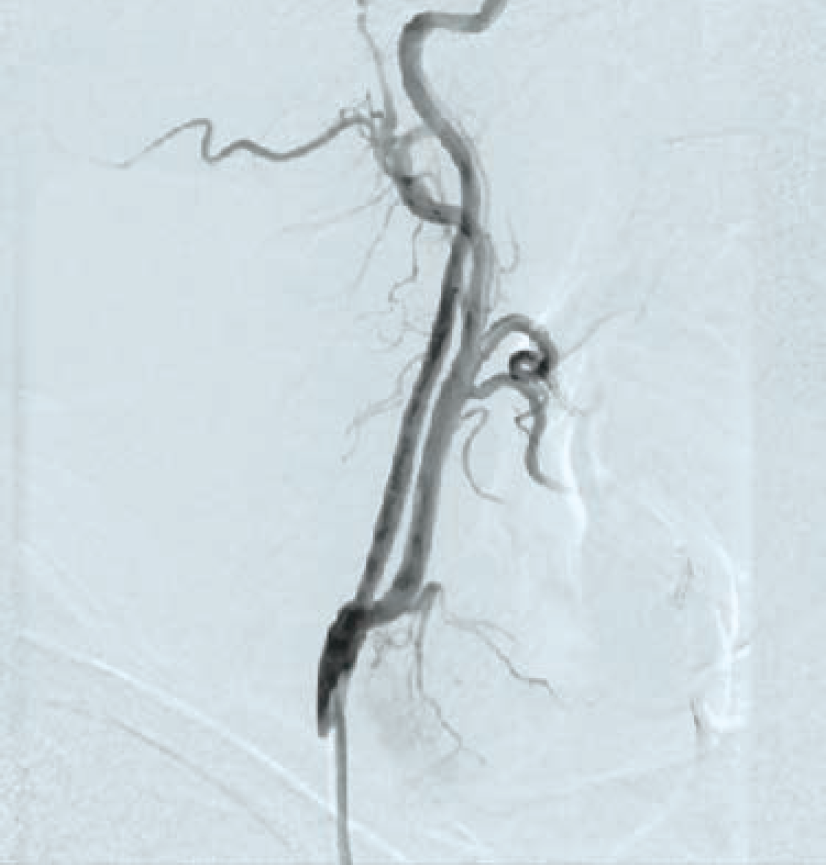
A 70-year-old hypertensive male presented with non-ST elevation myocardial infarction. Electrocardiogram showed ST depression. A complete blood count, complete blood chemistry, and PT/INR were in normal range. Lipid profile showed an LDL level of 147 mg/dl, triglycerides of 260 mg/dl, and HDL of 33 mg/dl. Coronary angiography showed triple-vessel coronary artery disease, sparing the left main stem. The patient was advised to undergo CABG surgery. During the surgical work-up, he was found to have a history of a TIA 3 months prior involving the left side of the body. Carotid Doppler showed a severe 95% ostial stenosis due to mixed plaque in the right internal carotid artery (RICA) and a mild stenosis causing 20% luminal narrowing in the left internal carotid artery. CT brain plain showed no infarction or hemorrhage. A carotid angiography and cerebral DSA showed severe stenosis at the ostium of RICA with no calcification (Figure 1). For the left ICA, both external carotid and vertebral arteries were normal. Cerebral digital subtraction angiography (DSA) showed normal intracranial circulation. A multidisciplinary approach, with a heart team including neurologists, cardiovascular surgeons, and an interventional cardiologist was adopted for this patient during the complete workup. The heart team recommended carotid revascularization prior to surgical coronary revascularization, as the patient was asymptomatic and at an intermediate risk from a coronary viewpoint. After a discussion with the patient and his family about the management options, advantages, and risks, a combined decision for CAS was made, due to its less-invasive nature as compared to CEA.
Procedure

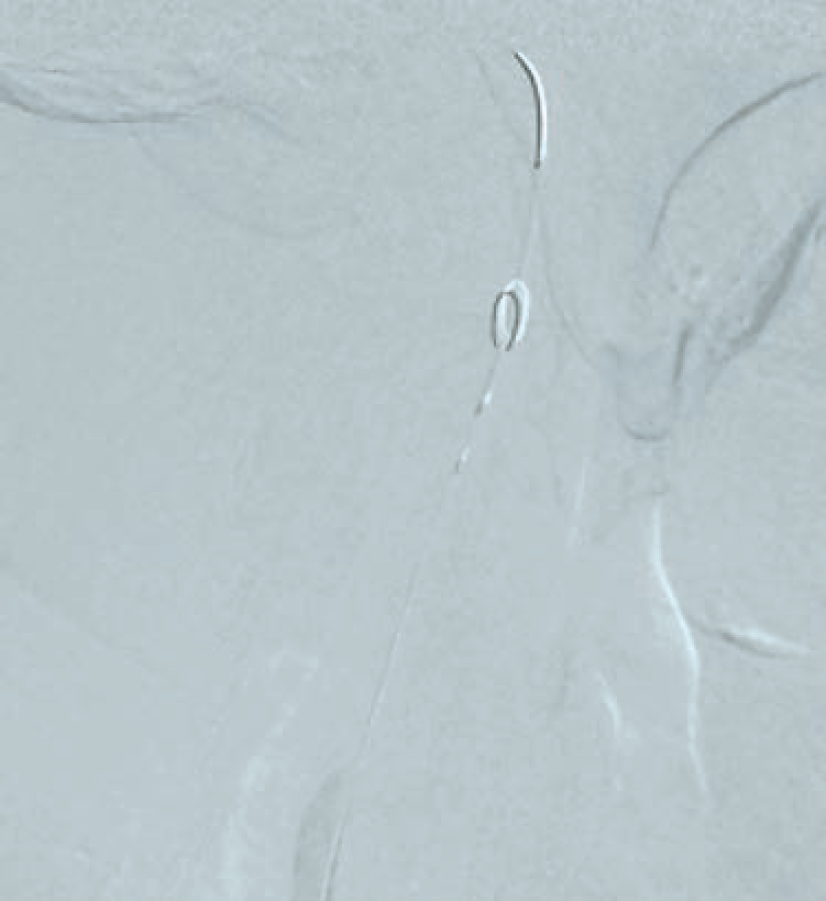
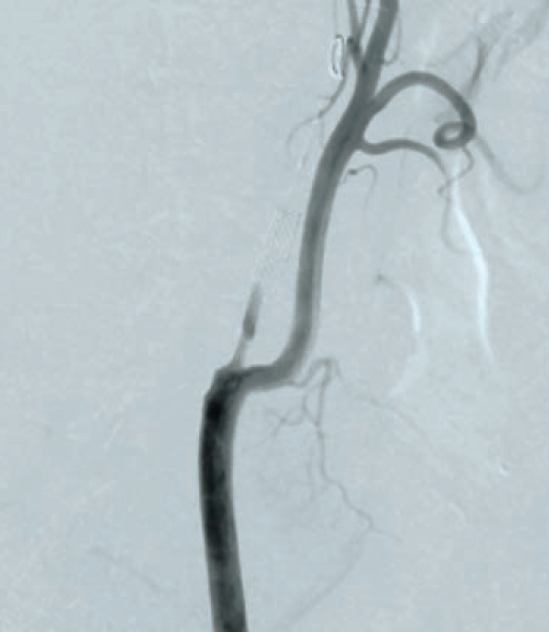
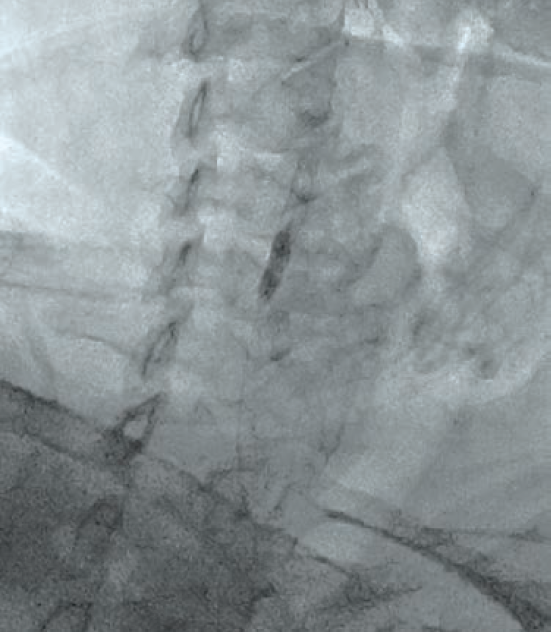
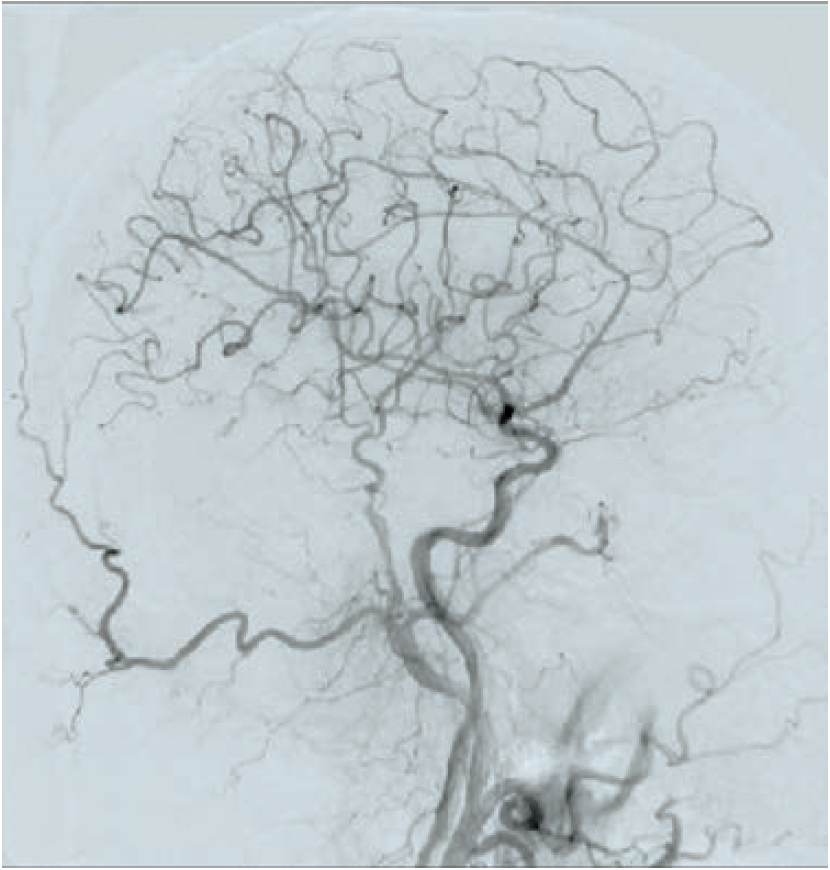
Following aseptic measures and under local anesthesia, a 7 French (Fr) right femoral access was obtained using a routine-length sheath. An .035-inch J-tip guide wire was then parked at the right common carotid artery (RCCA) using a 5 Fr Judkins right catheter, exchanged by a 7 Fr multipurpose guide. This was followed by advancement of a FilterWire EZ (Boston Scientific) across the ostial internal carotid artery stenosis, and deployed in the distal part of the extracranial ICA (Figure 2). After deployment of the FilterWire EZ, a direct stenting strategy was adopted to minimize thromboembolization. A 6 mm x 40 mm self-expanding stent was deployed at the RICA ostium (Figure 3). To our surprise, the view after stent placement showed zero flow into the distal RICA. (Figure 4) The reason appeared to be choking of the filter due to thromboembolization. The filter appeared to be overwhelmed by the volume of the debris captured. A 6 Fr Export catheter (Medtronic) was employed to suction debris from the distal ICA (Figure 5). We also administered pharmacotherapy using intra-arterial nitrate boluses and a weight-based tirofiban bolus. After these measures, there was fair flow into the distal ICA. During the period of no flow, the patient had transient hemispheric ischemic signs and an oropharyngeal airway was required, but his vitals remained stable. These symptoms rapidly resolved after establishment of ICA flow. After establishing blood flow, the proximal half of the stent that remained under-expanded was post dilated using a 4.5 mm noncompliant balloon at 12 atmospheres (Figure 6). Post dilatation, the angiographic view demonstrated good stent expansion and adequate distal flow (Figure 7). The distal protection device was then successfully removed using its retrieval sheath. The final DSA angiogram revealed excellent flow into the distal carotid (Figure 8A) and intracranial vasculature (Figure 8B), confirming no intracranial embolization. The guide was then safely removed over the .035-inch guide wire.
The patient tolerated the procedure well and was shifted to the cardiac care unit, where he remained stable, albeit with some irritability, but without any neurological deficit. After 24 hours of observation, he became fully oriented, the irritability was no longer present, and he was mobilized. The patient was started on dual antiplatelet therapy (DAPT), comprised of aspirin 75 mg once daily and clopidogrel 75 mg once daily. No additional medications were administered during the procedure. He was discharged the next day. The patient was evaluated on follow-up at one week and 6 weeks for neurological impairment and medication adherence, along with carotid ultrasound. The follow-up was uneventful, without any adverse or unanticipated event such as access-site complications, stroke, TIA, hemorrhage, hematoma, artery dissection, allergic reaction, restenosis, or device-related complications. After 6 weeks, he was referred to the surgeon for bypass surgery.

The patient continued his DAPT regimen for a duration of 12 months.* Following this period, he transitioned to single antiplatelet therapy. On subsequent follow-up, he has remained clinically stable and is doing well.
Discussion
There are multiple therapeutic intervention modalities for management of carotid stenosis. Since 2000, large-scale studies have taken place comparing CAS versus CEA, including the SAPPHIRE, EVA-3S, SPACE, ICSS, and CREST trials.4-8 Carotid vascular disease is not uncommon in patients with multivessel coronary artery disease. The surgical management of coronary artery disease can be confounded in patients with significant carotid vascular disease. CEA carries a high mortality when combined with CABG during the same procedure.9 CEA before CABG puts the patients at a higher risk of myocardial infarction, while CABG before CEA potentially increases the incidence of stroke.9 Revascularization by CAS immediately followed by CABG in high surgical-risk patients is a feasible and promising therapeutic strategy.9,10 In these patients, carotid stenting can be a safe and valuable therapeutic option. Distal protection is strongly indicated (class IIa)11 while performing CAS. A meta-analysis of 24 studies reported that embolic protection device use was related to approximately a 41% decrease in embolic stroke occurrence (relative risk 0.59; P<.001).12 The distal protection device captures the debris that breaks away while intervening in the diseased plaque, preventing embolization into brain circulation. Rarely, the debris can be overwhelming, choking the distal protection device and paradoxically leading to zero flow into ipsilateral hemisphere. Filter choking can be catastrophic if not immediately addressed. After identifying this complication in our case, the use of an Export aspiration catheter effectively lowered the burden of debris in the distal ICA. Of note, a literature search of Medline/PubMed did not find any case report over the past decade that described this complication.

Conclusion
Complications during carotid intervention are uncommon, but one should know and be prepared to handle a complication should one occur. Herein, we have described a rare case of distal embolic protection filter choking and de-choking while performing carotid artery stenting. The case was managed safely and successfully, and the patient went home without any neurological deficit.
*The DAPT regimen after carotid stenting in this case included: (1) aspirin 75mg once a day, which the patient was already taking before the procedure. It was continued without interruption until the last follow-up; (2) Clopidogrel 75mg once a day, which the patient took the day before carotid stenting and then continued post procedure for next 5 weeks and 2 days. Clopidogrel was then held for a period of 5 days, pre-CABG, and continued post CABG for 12 months.
References
1. Fairhead JF, Rothwell PM. The need for urgency in identification and treatment of symptomatic carotid stenosis is already established. Cerebrovasc Dis. 2005; 19(6): 355-358. doi:10.1159/000085201
2. De Rango P, Parlani G, Verzini F, et al. Long-term prevention of stroke: a modern comparison of current carotid stenting and carotid endarterectomy. J Am Coll Cardiol. 2011 Feb 8; 57(6):664-671. doi:10.1016/j.jacc.2010.09.041
3. Carotid artery stenting: rationale, indications, technique and results. In: Roubin GS, Iyer SS, Vitek JJ, et al, eds. Peripheral vascular stenting for cardiologists. 1st ed. Martin Dunitz Ltd; 1999: 67-118.
4. Yadav JS, Wholey MH, Kuntz RE, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med. 2004; 351:1493-1501. doi:10.1056/NEJMoa040127
5. Mas JL, Trinquart L, Leys D, et al. Endarterectomy Versus Angioplasty in Patients with Symptomatic Severe Carotid Stenosis (EVA-3S) trial: results up to 4 years from a randomised, multicentre trial. Lancet Neurol. 2008; 7:885-892. doi:10.1016/S1474-4422(08)70195-9
6. Eckstein HH, Ringleb P, Allenberg JR, et al. Results of the Stent-Protected Angioplasty versus Carotid Endarterectomy (SPACE) study to treat symptomatic stenoses at 2 years: a multinational, prospective, randomised trial. Lancet Neurol. 2008; 7:893-902. doi:10.1016/S1474-4422(08)70196-0
7. Komotar RJ, Starke RM, Connolly ES. Carotid endarterectomy vs endovascular stenting: recent results from ICSS and CREST. Neurosurgery. 2010; 66:N12-N13. doi:10.1227/01.neu.0000375271.39513.b2
8. George JC, White CJ. Carotid artery stenting lessons from CREST (Carotid Revascularization Endarterectomy Versus Stenting Trial). JACC Cardiovasc Interv. 2010; 3:988-990. doi:10.1016/j.jcin.2010.08.001
9. Abou-Assi S, Hanak CR, Khalifeh A, et al. Concomitant carotid and coronary artery disease management: a review of the literature. Ann Vasc Surg. 2025 Apr; 113: 319-326. doi:10.1016/j.avsg.2024.09.038
10. Versaci F, Del Giudice C, Scafuri A, et al. Sequential hybrid carotid and coronary artery revascularization: immediate and mid-term results. Ann Thorac Surg. 2007 Nov; 84(5): 1508-1513; discussion 1513-1514. doi:10.1016/j.athoracsur.2007.05.048
11. Aboyans V, Ricco JB, Bartelink MEL, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Rev Esp Cardiol (Engl Ed). 2018 Feb; 71(2): 111. doi:10.1016/j.rec.2017.12.014
12. Garg N, Karagiorgos N, Pisimisis GT, et al. Cerebral protection devices reduce periprocedural strokes during carotid angioplasty and stenting: a systematic review of the current literature. J Endovasc Ther. 2009 Aug; 16(4): 412-427. doi:10.1583/09-2713.1










