Percutaneous Transmural Arterial Bypass (PTAB) for Treatment of Recurring Femoral Artery In-Stent Restenosis Despite Prior Atherectomy and Drug-Coated Balloon Angioplasty
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Mehreen Ali1; Raza Malik2; Asad Rizvi, MD3; Akhil Gade, MD4; Mohammad Alqaim, MD, MS5
 1Second Year Undergraduate (UG 2), University of Texas, Austin; 2University of Texas, Dallas; 3Cardiology Fellow, Cardiovascular Diseases Fellowship Program, Medical City Fort Worth; 4Interventional Cardiology Fellow, Interventional Cardiology Fellowship Program, Medical City Forth Worth; 5Vascular Surgeon, Department of Vascular Surgery, Medical City Fort Worth, Fort Worth, Texas
1Second Year Undergraduate (UG 2), University of Texas, Austin; 2University of Texas, Dallas; 3Cardiology Fellow, Cardiovascular Diseases Fellowship Program, Medical City Fort Worth; 4Interventional Cardiology Fellow, Interventional Cardiology Fellowship Program, Medical City Forth Worth; 5Vascular Surgeon, Department of Vascular Surgery, Medical City Fort Worth, Fort Worth, Texas
Disclosures: The authors report no conflicts of interest regarding the content herein.
The authors can be contacted via Asad Rizvi, MD, at: asad.rizvi@medicalcityhealth.com
Case Presentation
A 72-year-old Caucasian woman presented with severe claudication (Rutherford class 3) of the right lower extremity. She participated in a supervised exercise program and had undergone multiple interventions in the right femoral artery, with restenosis of a Supera stent 6 mm x 120 mm (Abbott) treated with laser atherectomy and drug-coated balloon angioplasty. Her last intervention was approximately 6 months prior to her presentation, with claudication symptoms recurring at 4-5 months post intervention.
She had a past medical history of coronary artery disease status post percutaneous coronary intervention in 2011, chronic obstructive pulmonary disease, head and neck cancer status post radiation and resection, hypertension, and hyperlipidemia. She had a 40-pack per year history of smoking and quit 3 years ago.
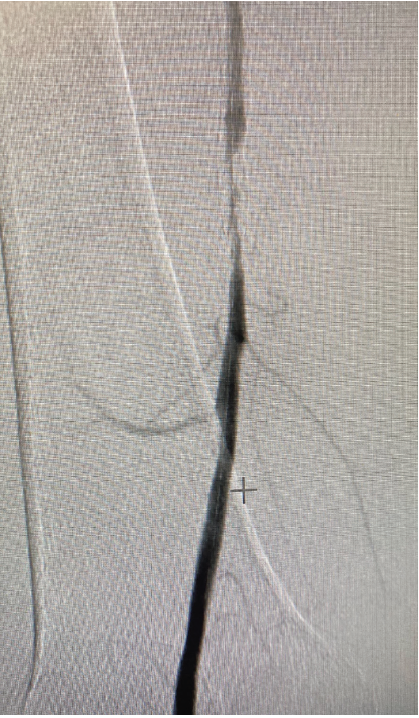
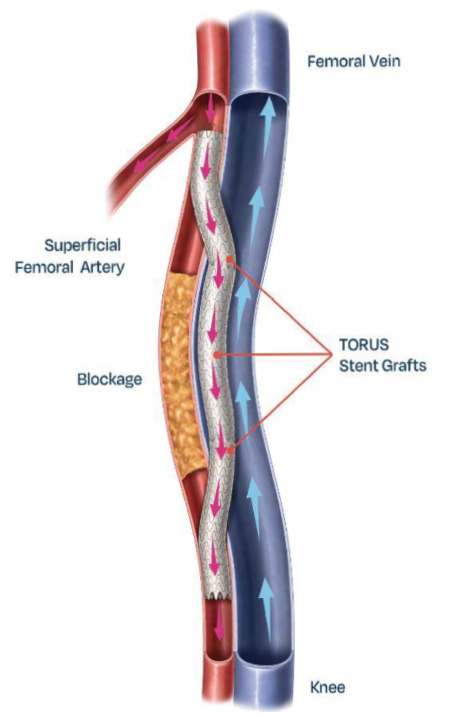
An arterial Doppler and subsequent diagnostic peripheral angiogram showed severe in-stent restenosis of the Supera stent in the right superficial femoral artery (SFA) (Figure 1). The patient was evaluated for surgical femoral popliteal artery bypass surgery versus percutaneous transmural arterial bypass (PTAB) with the DETOUR System (Endologix) (Figure 2). Due to frailty, poor pulmonary function tests, and patient preference for a minimally invasive approach, she was further evaluated for the PTAB procedure.
The SFA lesion was approximately 80 mm post atherectomy. The femoral vein was measured by Doppler and found to be >10 mm in diameter. The proximal SFA and popliteal artery were deemed acceptable in diameter (>6 mm) for a transmural bypass.
Intervention and Outcome
After left femoral access with an 8 French (Fr) sheath, an Omni Flush catheter (AngioDynamics) was inserted into the arterial sheath, and a contralateral right lower extremity angiogram was performed with two-vessel runoff visualized. Using a standard technique, ultrasound-guided percutaneous puncture was obtained, and a 6 Fr introducer sheath was placed in the patient’s right posterior tibial vein via a transpedal approach. The leg venogram was performed to evaluate the superficial femoral vein, measured to be 12 mm in diameter. An EN Snare (Merit Medical) was inserted into the venous sheath and advanced to the lesser trochanter level. An Endocross (Endologix) was inserted over an .019-inch wire through the left femoral arterial sheath and advanced into the right SFA to the level of 3-4 mm distal to the SFA and profunda bifurcation. The EN Snare was oriented in projection to superimpose the Endocross with a snare. The Endocross was fired 2 times to create a proximal anastomosis. A 300 cm Choice floppy wire (Boston Scientific) was advanced into the femoral vein, was snared by the EN Snare, and removed from the venous sheath.
The Endocross was then removed and re-prepped. A 4 mm percutaneous transluminal angioplasty (PTA) balloon was used to dilate the arterial and venous anastomosis proximally. The Endocross was advanced over the wire, through the proximal anastomosis into the vein, and was positioned distal to the occlusion. The Endocross was superimposed over the popliteal artery. An angiogram was taken through the sheath to visualize the reconstitution of the blood flow in the popliteal artery. The Endocross was refired 3 times to create a distal anastomosis that obtained access to the popliteal artery. A Choice PT 300 cm wire (Boston Scientific) was advanced into the popliteal artery into the tibial artery distally.
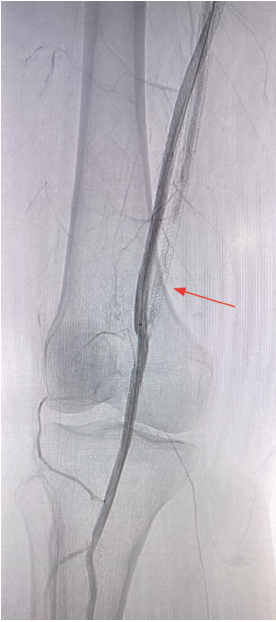
The Endocross was then removed, and a 5 mm PTA balloon was advanced over the Choice PT .014-inch wire across the distal venous and arterial anastomoses. The PTA balloon was used for the dilatation of the distal arteriovenous anastomosis. The PTA balloon was then advanced and the Choice PT .014-inch wire was exchanged for a Supra Core 300 cm wire (Abbott). The first stent graft was placed, extending a minimum of 3 mm into the distal popliteal artery. Three overlapping stent grafts were deployed, extending from the popliteal artery to the proximal SFA, followed by post-dilation extending approximately 2 mm above the proximal edge of the SFA and profunda bifurcation. The stent delivery system was removed. The graft was then post dilated with a 6 mm PTA balloon focusing on the anastomosis. A final angiogram procedure was performed to visualize anterior artery blood flow in the anterior tibial artery. A final venogram was performed and venous flow was visualized. An Angio-Seal (Terumo) was used to close the left femoral artery. Final imaging demonstrated an open percutaneous femoral popliteal bypass (Figure 3, Video). The patient was discharged on Eliquis 2.5 mg with plans for repeat arterial Doppler at one month, 3 months, 6 months, and thereafter in a yearly fashion. At the one-month follow-up, the bypass was found to be widely patent and the patient remained symptom free.
Discussion
Treatment options for patients with peripheral arterial disease who have lifestyle-limiting symptoms despite optimal medical therapy include endovascular approaches, ie, balloon angioplasty, stenting, atherectomy, and open surgical bypass.1 Current guidelines recommend endovascular treatment for short focal stenosis (<10 cm) or occlusion (TASC A and B). Treating long, complex lesions via endovascular techniques can be difficult, leading to reduced patency rates and the necessity of frequent procedures. Therefore, open bypass surgery has been the treatment option for TASC C (unless high risk) and TASC D (long stenosis or occlusion) lesions.2,3
Our patient had undergone multiple endovascular interventions, developing in-stent restenosis that was treated with laser atherectomy and drug-coated balloon angioplasty. Consequently, surgical bypass was the next step in managing her severe disease, but she was deemed a poor surgical candidate due to frailty. Open bypass involves higher perioperative risk and prolonged recovery, particularly in patients with comorbidities.
The PTAB Procedure. The percutaneous transmural arterial bypass (PTAB) procedure was developed with the goal of providing results comparable to surgical bypass without the complications associated with traditional methods. An endovascular technique is used to bypass the superficial femoral artery (SFA) instead of relying solely on an intra-arterial approach. The procedure utilizes a system that includes a stent graft and crossing device for creating a percutaneous, endovascular femoropopliteal bypass. The stent graft is a self-expanding nitinol frame covered with ePTFE (expanded polytetrafluoroethylene) film and is delivered via a dual guide wire crossing device. This device is designed as a spring-loaded dual guide wire delivery tool equipped with an .025-inch nitinol needle with a 15 mm range of motion.4,5
Clinical Studies. The PTAB procedure has been studied in the DETOUR I and 2 trials. DETOUR I demonstrated that PTAB is a safe and effective option for endovascular femoropopliteal bypass in patients with complex long-segment occlusive disease.4 This trial included patients with challenging characteristics, such as long lesion lengths and severe calcification. Key findings included a 1-year primary patency rate of 81% with no major amputations and a 15% reintervention rate.4 Limitations of the trial include a small sample size and the absence of comparisons to alternative therapies.
DETOUR2 evaluated the safety and effectiveness of PTAB using the DETOUR system for patients with moderate to severe femoropopliteal artery disease.5 The study involved anatomically challenging cases, with a mean superficial femoral artery (SFA) lesion length of around 33 cm, where 96% of lesions were chronic total occlusions (CTOs), 17.3% in-stent restenosis, and 70% severely calcified.5 Results showed a technical success rate of 100% and a procedural success rate of 98.5%.5 Primary safety and effectiveness endpoints were exceeded, with only 7% of patients experiencing major adverse events at 30 days and 72% achieving primary patency at one year.5 These results align with the DETOUR I trial, suggesting PTAB is a promising option for patients with symptomatic SFA lesions longer than 20 cm. In contrast to surgical bypass, PTAB demonstrated low complication rates (anesthesia-related complications, wound infections) with significant improvements in patient outcomes.5 Both studies showed improvement in ankle-brachial index (ABI) and Rutherford class.
DETOUR2 underscores the potential advantages of the PTAB approach over surgical bypass, particularly for complex cases. While there is some concern regarding venous complications related to the use of the Torus stent graft, the study reported a low deep vein thrombosis rate of 4.1% at one year, with no pulmonary embolism.5 However, limitations include the study’s single-arm design, challenges in generalizing results, and the need for further research to validate efficacy compared to alternative treatments. Continued follow-up will provide more long-term data, enhancing understanding of PTAB’s performance relative to surgical bypass and other interventions.
Conclusion
This case illustrates the utility of the PTAB procedure as a feasible, minimally invasive alternative for recurrent in-stent restenosis when surgery is not an option. More definitive outcomes are expected from longer follow-up studies.
References
1. Shabani Varaki E, Gargiulo GD, Penkala S, Breen PP. Peripheral vascular disease assessment in the lower limb: a review of current and emerging non-invasive diagnostic methods. Biomed Eng Online. 2018 May 11;17(1):61. doi:10.1186/s12938-018-0494-4
2. TASC Steering Committee; Jaff MR, White CJ, Hiatt WR, et al. An update on methods for revascularization and expansion of the TASC lesion classification to include below-the-knee arteries: a supplement to the inter-society consensus for the management of peripheral arterial disease (TASC II). Vasc Med. 2015 Oct; 20(5): 465-478. doi:10.1177/1358863X15597877
3. Bailey SR, Beckman JA, Dao TD, et al. ACC/AHA/SCAI/SIR/SVM 2018 Appropriate use criteria for peripheral artery intervention: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Heart Association, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, and Society for Vascular Medicine. J Am Coll Cardiol. 2019 Jan 22; 73(2): 214-237. doi:10.1016/j.jacc.2018.10.002
4. Krievins DK, Halena G, Scheinert D, et al. One-year results from the DETOUR I trial of the PQ Bypass DETOUR System for percutaneous femoropopliteal bypass. J Vasc Surg. 2020 Nov; 72(5): 1648-1658.e2. doi:10.1016/j.jvs.2020.02.043
5. Lyden SP, Soukas PA, De A, et al; DETOUR2 Trial Investigators. DETOUR2 trial outcomes demonstrate clinical utility of percutaneous transmural bypass for the treatment of long segment, complex femoropopliteal disease. J Vasc Surg. 2024 Jun; 79(6): 1420-1427.e2. doi:10.1016/j.jvs.2024.02.004










