PCI of Medina 0.0.1 Bifurcation Lesion: Orbiting Around the Ostium
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Saroj Kumar Sahoo, MD, DM1; Sindhu Rao Malla, MD2; Ramachandra Barik, MD, DNB3; Debasis Acharya, MD, DM4; Debasis Panda, MD2; Prabhat Kumar Singh, MD2
1Corresponding Author; Assistant Professor, Department of Cardiology
2Cardiology Fellow, Department of Cardiology
3Professor and HOD, Department of Cardiology
4Associate Professor, Department of Cardiology
All India Institute of Medical Sciences (AIIMS) Bhubaneswar, Odisha, India
The authors can be contacted via Saroj Kumar Sahoo, MD, DM, at tem_sarojkumar@aiimsbhubaneswar.edu.in
Abstract
Medina 0.0.1 bifurcation lesions, which only affect the side branch ostium, account for less than 5% of bifurcations. These lesions pose a significant challenge, especially when they involve the unprotected left main coronary artery. We report a successful revascularization of a heavily calcified Medina 0.0.1 bifurcation lesion in a 74-year-old male with multiple co-morbidities who is at high risk for CABG, using orbital atherectomy and a cutting balloon under IVUS guidance.
Coronary bifurcation lesions occur in approximately 20% of cases in modern interventional cardiology practice and are associated with increased rates of major adverse cardiac events.1 Among these, Medina 0.0.1 bifurcation lesions, which only affect the side branch ostium, constitute less than 5%.2 These lesions present a significant challenge, particularly when they involve the unprotected left main coronary artery (LMCA). Herein, we report a successful revascularization of a Medina 0.0.1 bifurcation lesion of a heavily calcified left circumflex (LCx) artery using orbital atherectomy and a cutting balloon for support.
Case Details
A 74-year-old male, a known case of diabetes, hypertension, and chronic kidney disease with a history of coronary artery disease post-percutaneous coronary intervention (PCI) to the LCx with drug-eluting stent seven years prior, presented to the emergency department with complaints of chest pain over the past 2 days. An electrocardiogram showed sinus rhythm with left ventricular hypertrophy and T wave inversions in inferolateral leads. Echocardiography revealed hypokinesia in the right coronary artery (RCA)/LCx territory and an ejection fraction of 40%.
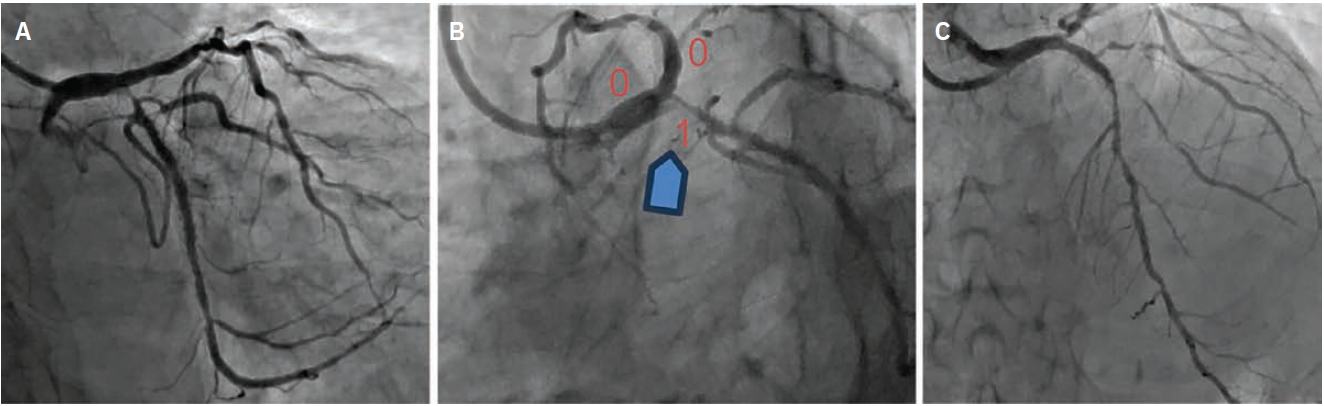
A coronary angiogram showed distal LMCA and mild ostial left anterior descending (LAD) plaque, an ostial LCx 95% stenosis (Medina 0.0.1) (Figure 1A-B, Video 1), and a proximal to mid-LAD long segment lesion with a maximum of 80% stenosis and heavy calcification (Figure 1C). The prior LCx stent had mild in-stent restenosis and the distal RCA had an 80% stenosis with no significant calcification. The patient’s estimated glomerular filtration rate (eGFR) was 17.8 ml/min/1.73m2, SYNTAX score I: 19, SYNTAX score II: PCI – 50.1 (4-year mortality 31.8%), coronary artery bypass graft (CABG) – 40.2 (4-year mortality 15.3%), and EuroSCORE II: 13.8% (high surgical risk). The patient and family members denied CABG. A heart team discussion was conducted. Given the patient’s multiple comorbidities and high surgical risk, after written consent, he was taken for multivessel PCI.
Procedure
In the cardiac catheterization laboratory, the distal RCA was stented via right radial access using a 6 French (F) Judkins right (JR) 3.5 guiding catheter. The procedure was uneventful. For the left Medina 0.0.1, we planned for PCI to the mid to distal LAD and an inverted provisional strategy for the LMCA to LCx. Angiographically, the lesion looked calcified in both the LAD and LCx. Intravascular ultrasound (IVUS) and calcium modification devices were prepared (orbital atherectomy and a cutting balloon).
PCI to the left system was performed using a 7F extra backup support (XB) LAD 3.5 guiding catheter. The LAD was crossed with Fielder FC guidewire (Asahi Intecc), and IVUS showed heavy calcium burden from the distal LMCA to mid LAD. Orbital atherectomy was performed with a 1.25 mm burr at 120,000 rpm in the mid LAD and at 80,000 rpm in the distal LAD. Additionally, dilatation was done with a 3 mm x 10 mm cutting balloon. A 3.5 mm x 44 mm stent was then deployed in the mid to distal LAD, followed by post dilatation with a 3.5 mm x 10 mm noncompliant (NC) balloon.
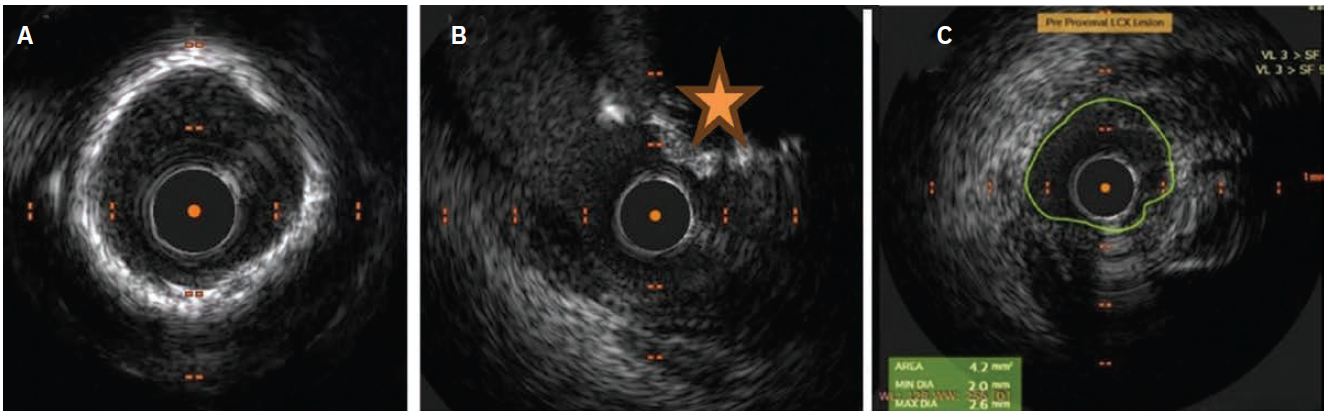
(B) Calcium Nodule-1, (C) Vessel diameter ≤3.5 mm-0.
The LCx was crossed with a Fielder FC guide wire and IVUS showed heavy calcification with calcific nodules. IVUS Calcium Score: 3; (Calcium ≥270 with ≥5 mm:1, 360-degree Calcium:1, Calcium Nodule:1, vessel diameter ≤3.5 mm:0) (Figure 2A-2C). Orbital atherectomy was done with a 1.25 mm burr at 120,000 rpm in the LCx (Video 2) followed by dilatation with a 3.5 mm x 10 mm cutting balloon. LMCA to LCx crossover stenting was done with a 3.5 mm x 28 mm drug-eluting stent, ensuring overlap with the in situ LCx stent, and proximal optimization technique (POT) of the LMCA was done with a 5 mm x 8 mm balloon. A a 4 mm x 10 mm NC balloon was used for post dilatation of the LCx, followed by kissing balloon inflation of the LAD/LCx (Figure 3A-3E).
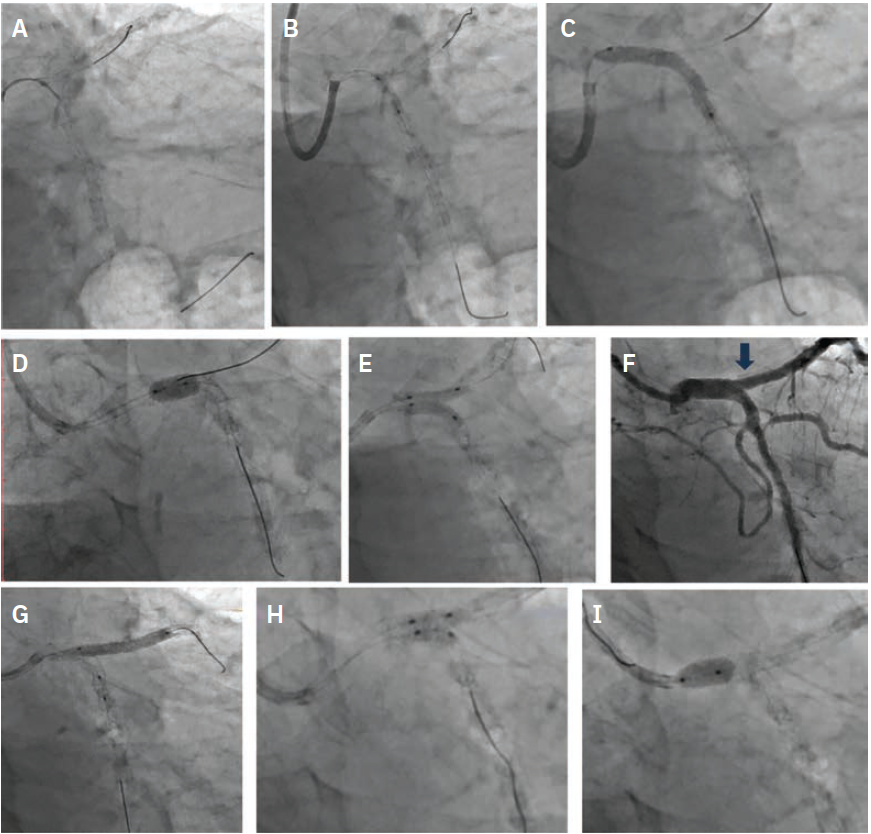
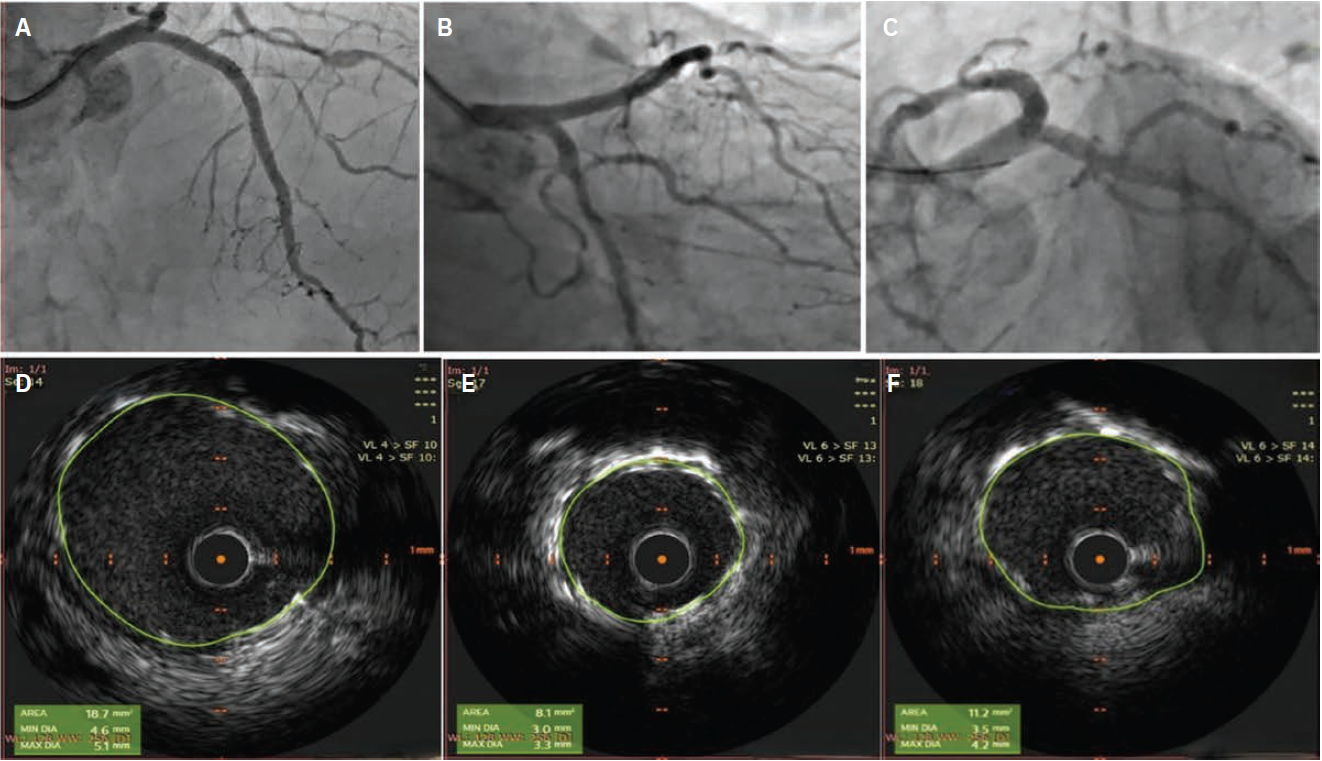
Angiography revealed a type B dissection in the proximal LAD (Video 3), confirmed by IVUS (Figure 3F). Hence, proximal LAD stenting was done using the T and small protrusion (TAP) technique with a final kissing balloon inflation and re-POT (Figure 3G-3I). Final cine showed TIMI grade-III flow in both the LAD and LCx (Figure 4A-4C, Video 4). IVUS showed excellent stent apposition and expansion. The LMCA, LCx, and LAD had a minimum stent area (MSA) of 18.7, 8.1, and 11.2 mm2, respectively (Figure 4D-4F). The patient was discharged two days later in stable condition. At the 3-month follow-up, the patient was doing well, with no further anginal symptoms, and his ejection fraction improved to 48%.
Discussion
Medina 0.0.1 bifurcation lesions lack thorough study, with an optimal treatment strategy still under debate. When performing PCI for a Medina 0.0.1 lesion in the LMCA, the primary concern is the risk of LMCA injury, which can occur during the procedure or later. Management of Medina 0.0.1 bifurcation lesions depends on the risk-benefit ratio, as the side branch supplies a smaller myocardial area, and periprocedural myocardial infarction involving the LMCA can be catastrophic.
An important concept for Medina 0.0.1 lesions is main branch protrusion and ostial miss. Ostial lesions are commonly characterized as being fibrotic, calcified, and relatively expansion-resistant. They are associated with higher rates of target lesion revascularization (TLR) and procedural complications such as dissections, vessel closure, and myocardial infarction.3
A recent study of 273 patients undergoing PCI for Medina 0.0.1 lesions showed higher levels of major adverse cardiac events (MACE) and TLR in the long term, with an incidence of 16.9% and 13.4%, respectively.4 Calcification is one of the strongest predictors of poor short- and long-term PCI outcomes. The extent of coronary calcification significantly impacts procedural safety and effectiveness, primarily by increasing the likelihood of suboptimal stent expansion. This, in turn, is closely associated with a higher risk of target lesion failure, particularly in-stent restenosis and stent thrombosis.5
Lesion preparation is crucial due to the high calcium burden in bifurcation lesions, especially in elderly patients with comorbidities. Debulking devices like orbital atherectomy facilitate effective lesion preparation, ensuring proper stent placement and reducing complications. Orbital atherectomy uses differential sanding and pulsatile forces to fracture calcified lesions while maintaining blood flow with minimal heat damage, enhancing PCI benefits and long-term outcomes.6 The multicenter BIFURCAT study7 comparing 1- and 2-stent strategies in Medina 0.0.1 lesions found similar MACE risk between both approaches, with no significant demographic differences. Notably, the 2-stent group had higher LMCA involvement and calcification. The study noted worse one-year PCI outcomes for Medina 0.0.1 lesions compared to other bifurcation types.
A key strategy for bifurcation stenting with a single stent is the inverted provisional technique, first described by Brunel et al.8 It involves crossover stenting from the main vessel to the side branch, followed by kissing balloon inflation and final optimization. This ensures complete ostial coverage of the side branch and is safe if the main vessel is compromised, since deploying a second stent is straightforward. This technique is best used when the main and side vessels are similar in size. Brunel et al evaluated the safety of the inverted provisional technique in 40 patients, finding 100% procedural success, low TLR rates, and high short-term safety. However, this study did not compare the technique with other methods. In our case, although we planned for the use of an inverted provisional technique, we had to perform additional stenting in the proximal LAD due to a type B dissection after kissing balloon inflation.
Conclusion
Medina 0.0.1 lesions, though rare, pose distinct challenges such as main vessel injury, protrusion, and ostial miss. Treatment strategies must be tailored to each patient’s clinical presentation, with patient selection for invasive procedures prioritized over revascularization strategy. Preparing the lesion properly is crucial and early planning for debulking using intravascular imaging is recommended. The prognosis after PCI for Medina 0.0.1 lesions is poorer than other bifurcation subtypes. More robust studies are needed to determine the best treatment options for these lesions.
References
1. Panayotov P, Mileva N, Vassilev D. Current challenges in coronary bifurcation interventions. Medicina (Kaunas). 2024 Sep 3; 60(9): 1439. doi:10.3390/medicina60091439
2. Conrotto F, Bruno F. Medina 0.0.1. bifurcations: Let’s keep it simple. Int J Cardiol. 2025 Mar 1; 422: 132908. doi:10.1016/j.ijcard.2024.132908
3. Jokhi P, Curzen N. Percutaneous coronary intervention of ostial lesions. EuroIntervention. 2009 Sep; 5(4): 511-514. doi:10.4244/eijv5i4a81.
4. Maurina M, Riche M, Oliva O, et al. Decoding medina 0.0.1 bifurcation: Are all codes equal? Results from a multicentric registry. Int J Cardiol. 2025 Feb 15; 421: 132863. doi:10.1016/j.ijcard.2024.132863
5. Rola P, Włodarczak S, Furtan Ł, et al. First experience with orbital atherectomy in calcified unprotected left main percutaneous coronary intervention. Postepy Kardiol Interwencyjnej. 2023 Mar; 19(1): 64-66. doi:10.5114/aic.2022.121990
6. Shlofmitz E, Martinsen BJ, Lee M, et al. Orbital atherectomy for the treatment of severely calcified coronary lesions: evidence, technique, and best practices. Expert Rev Med Devices. 2017 Nov; 14(11): 867-879. doi:10.1080/17434440.2017.1384695
7. Choi KH, Bruno F, Cho YK, et al. Comparison of outcomes between 1- and 2-stent techniques for Medina classification 0.0.1 coronary bifurcation lesions. JACC Cardiovasc Interv. 2023 Sep 11; 16(17): 2083-2093. doi:10.1016/j.jcin.2023.06.013
8. Brunel P, Martin G, Bressollette E, et al. “Inverted” provisional T stenting, a new technique for Medina 0,0,1 coronary bifurcation lesions: feasibility and follow-up. EuroIntervention. 2010 Feb; 5(7): 814-820. doi:10.4244/eijv5i7a136
Find More:
Renal Denervation Topic Center
Cardiovascular Ambulatory Surgery Centers (ASCs) Topic Center
Grand Rounds With Morton Kern, MD
Peripheral Artery Disease Topic Center
Podcasts: Cath Lab Conversations










