Hybrid Revascularization of a Thrombosed Bypass Graft with the Artix Thrombectomy System
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
George DeKornfeld, MD
Vascular Surgery, Conemaugh Memorial Medical Center, Johnstown, Pennsylvania
Disclosure: Dr. DeKornfeld reports he is a consultant for Inari Medical.
George DeKornfeld, MD, can be contacted at gdekornf@conemaugh.org
Abstract
Surgical bypass is a primary treatment for acute limb ischemia, and high-risk procedures such as axillofemoral bypasses are necessary when other revascularization options have been exhausted. However, bypass grafts can occlude, necessitating prompt intervention. We report a hybrid procedure using the Artix Thrombectomy System to clear an occluded axillary-profunda bypass graft, followed by profundoplasty to enhance profunda flow and optimize the distal target. Artix removed substantial subacute thrombus. Patch angioplasty was successful. The graft remained patent at 1 month post procedure. This hybrid approach preserved graft integrity and avoided replacement surgery, maintaining future reintervention options in case of re-thrombosis or graft failure.
Introduction
Peripheral artery disease (PAD) affects more than 230 million worldwide.1 When other treatment options fail, bypass grafts become necessary to restore adequate circulation. The axillary-profunda bypass, which creates a conduit between the axillary to profunda femoris arteries, is an uncommon but critical revascularization procedure for patients with limited options.2 However, maintaining long-term patency necessitates ongoing surveillance and potential interventions to prevent recurrent ischemia.
Hybrid revascularization procedures have emerged as a valuable approach in patency maintenance. By combining open surgical techniques with endovascular interventions, a tailored approach can be taken to optimize flow restoration. The rise of hybrid procedures led to the clinical guideline recommendation of completion angiography at the end of each procedure to ensure prompt diagnosis of complications and treatment with endovascular means.3
We present a case in which the Artix Thrombectomy System (Inari Medical) was utilized in a hybrid procedure to revascularize a thrombosed axillary-profunda bypass graft followed by profundoplasty. The Artix system is a dual mechanical and aspiration thrombectomy platform designed to remove acute-to-chronic arterial thromboemboli. It features a thin-walled sheath, an aspiration catheter, a covered funnel catheter for proximal flow restriction, and a mechanical thrombectomy (MT) device with an expandable element to disrupt and remove thrombus. This is the first use case of Artix in an upper extremity proximal anastomosis and as part of a hybrid procedure. The patient consented to the publication of their case details and associated images.
Case Report
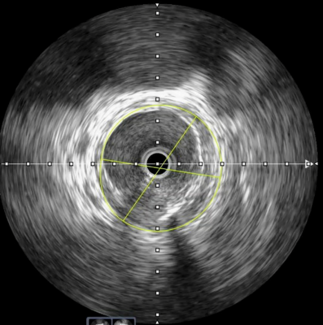
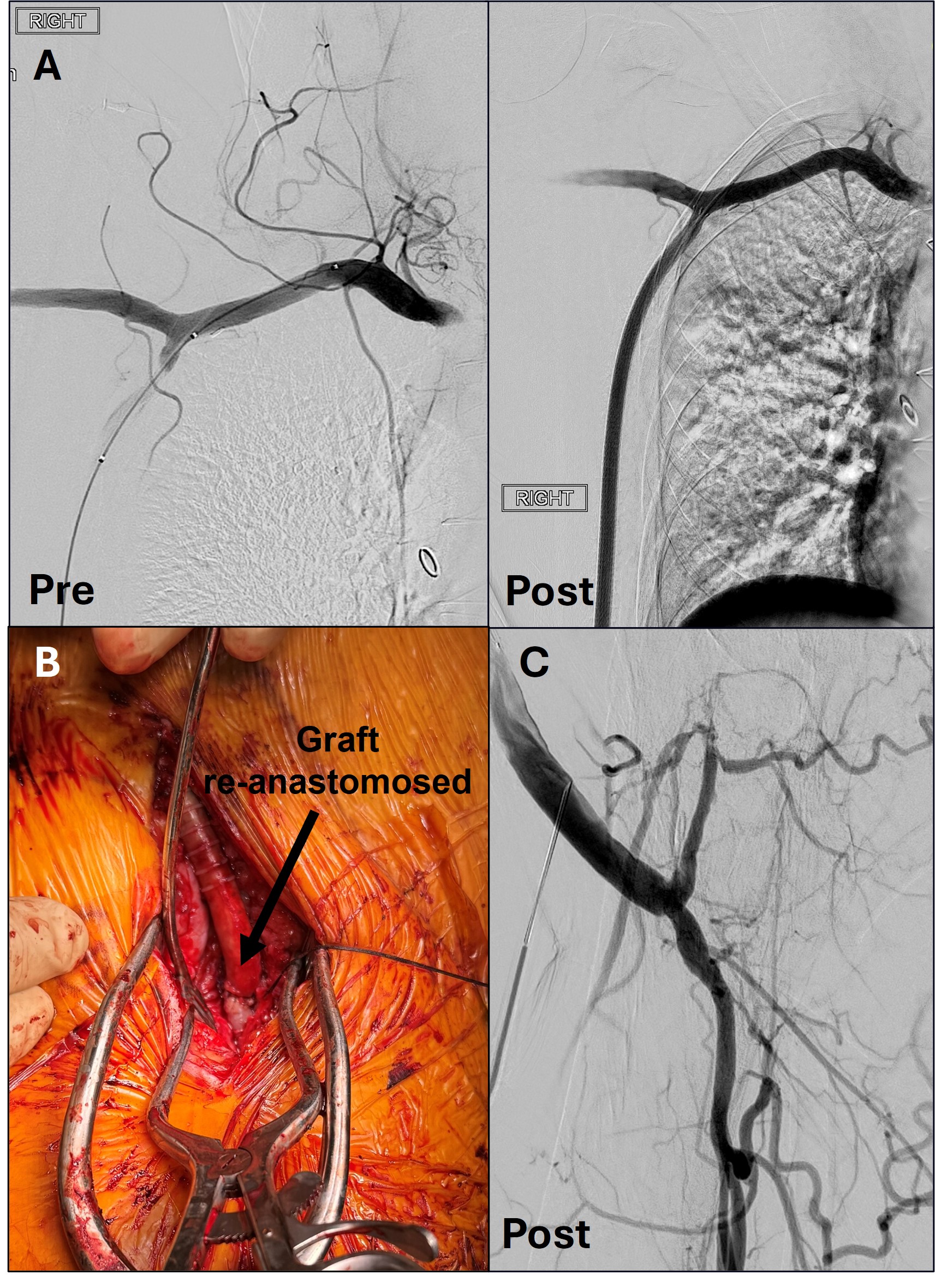
A 63-year-old male with PAD presented with right leg pain, claudication, and paresthesia in his foot. The patient also reported right ankle pain and a burning sensation in his right thigh one month prior. His history included an occluded right iliac stent, a failed right iliofemoral bypass graft, right common femoral endartectomy and profundoplasty, failed right femoral-popliteal bypass graft, and a right axillary-profunda bypass graft placed two years prior due to a hostile groin after femoral-popliteal graft infection. Computed tomography angiography showed a completely thrombosed axillary-profunda graft (Figure 1). A decision was made to revascularize the axillary-profunda graft using Artix followed by profundoplasty.
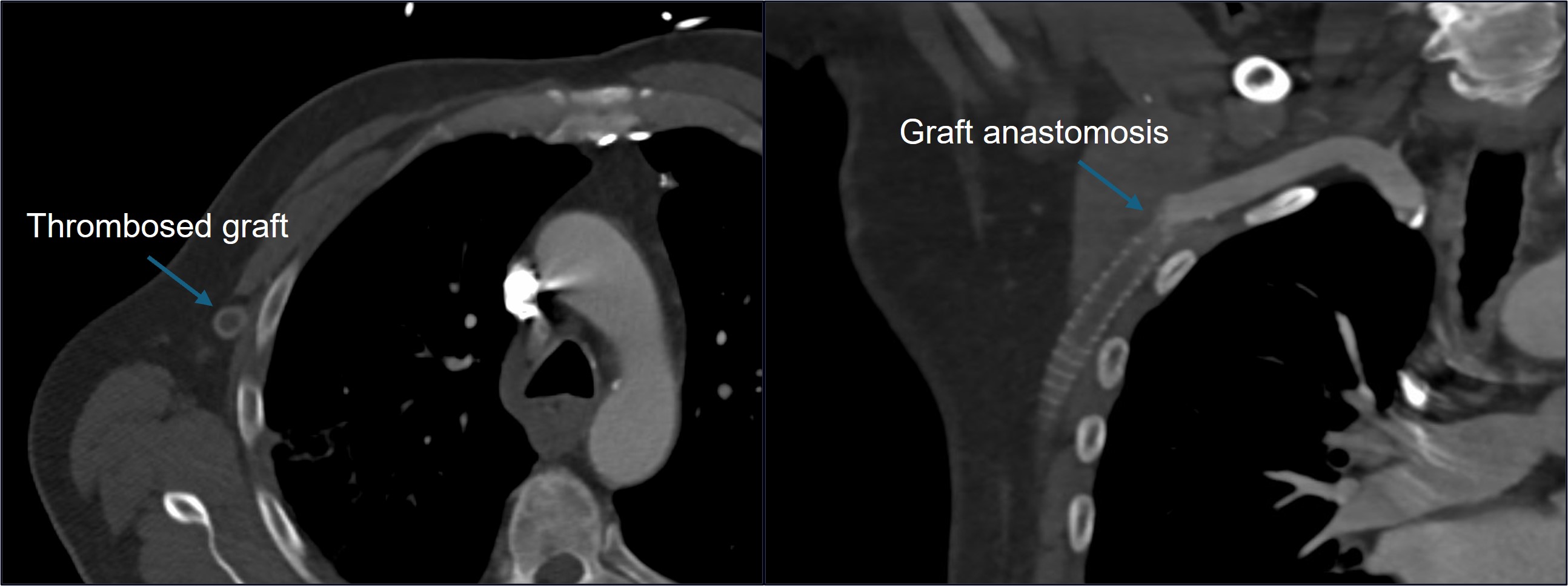
With the patient in a supine position under general anesthesia, a longitudinal incision of the right groin was performed. Systemic heparin was administered to maintain an activated clotting time of 300 seconds. Next, the profunda was exposed, and an incision was made at the graft anastomosis (Figure 2A). A 0.035-in Quick-Cross support catheter (Philips) loaded with a stiff Glidewire guidewire (Terumo Interventional Systems) was inserted and used to cross the long segment occlusion. After crossing, the guidewire was placed in the right axillary artery, then exchanged for a 0.014-in Mailman guidewire (Boston Scientific). An MT8 thrombectomy device, the mechanical component of the Artix system for vessels 4 mm to 8 mm in diameter, was inserted and advanced into the axillary artery (Figure 2B), where mechanical thrombectomy was performed through the entire graft.
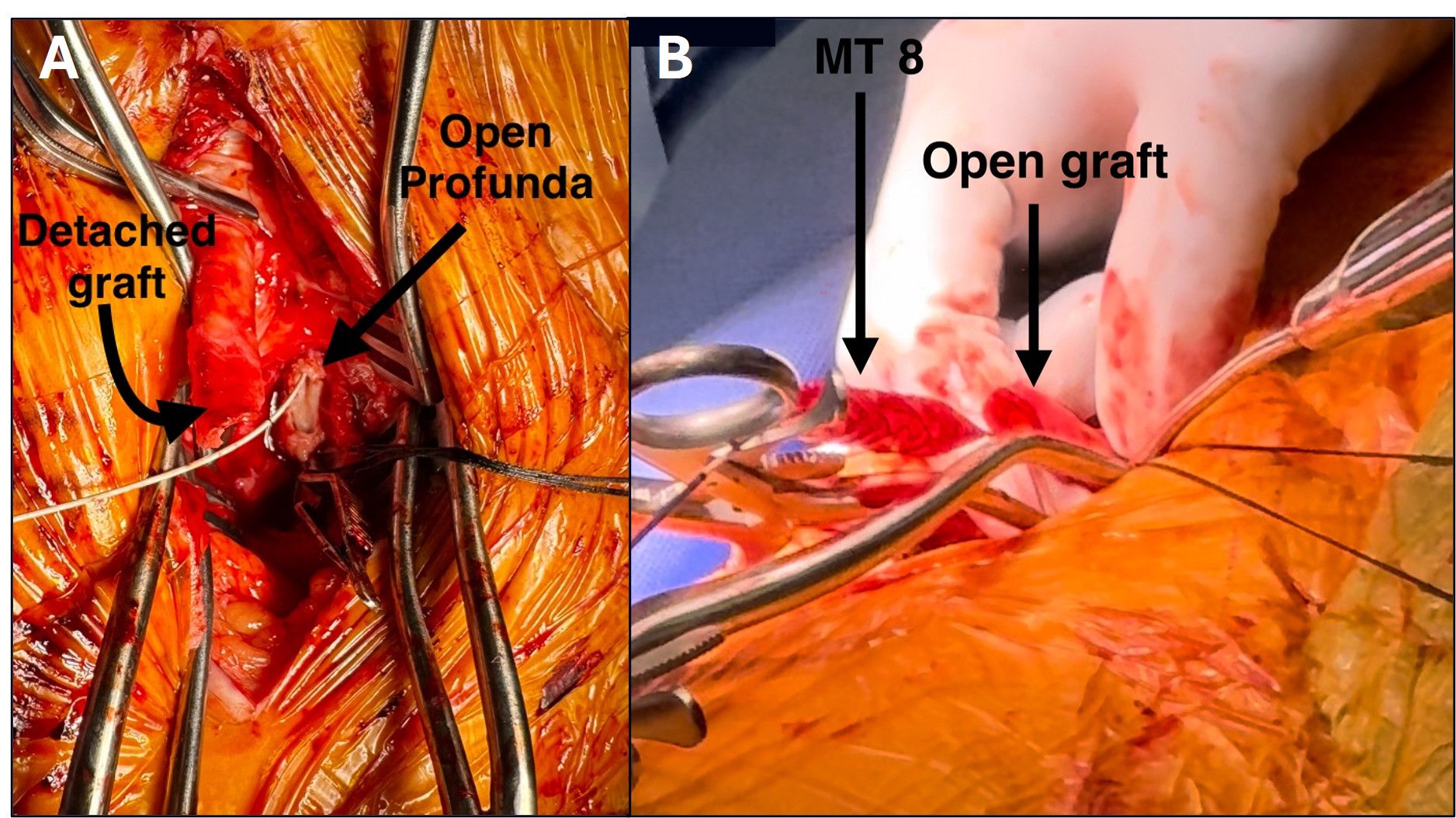
A large amount of subacute-appearing thrombus with an absence of blood flow was removed after the first pass (Figure 3A). After the element was cleared of thrombus with the cleaning accessory (Figure 3B,C), three more thrombectomy passes were performed, removing additional thrombus (Figure 3D).
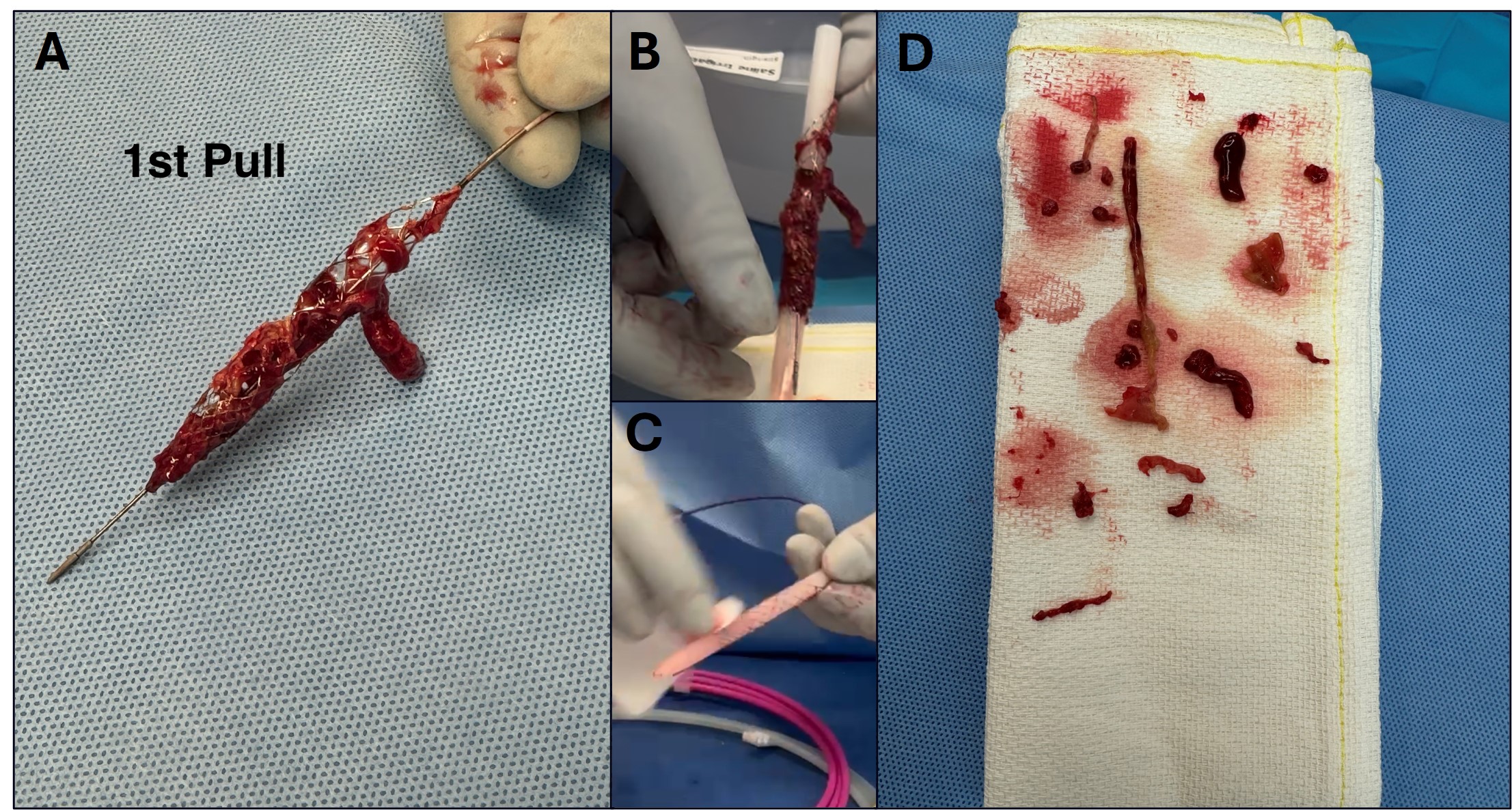
Angioplasty of the graft with a 5 mm x 10 cm balloon was performed. A final pass with Artix yielded no thrombus, robust blood flow, and a strong palpable pulse. Angiography demonstrated a patent graft (Figure 4A).
To ensure the best odds of graft preservation given limited long-term options, 6 Viabahn stents (Gore Medical) were placed from the proximal anastomosis with adequate overlap down to the distal aspect of the graft. Next, patch angioplasty was performed on the mid profunda to improve outflow, and the newly patent graft was reattached to the profunda (Figure 4B). Completion angiography revealed a widely patent graft and profunda (Figure 4C). Doppler ultrasound confirmed flow restoration. Hemostasis was achieved, and the groin wound was closed.
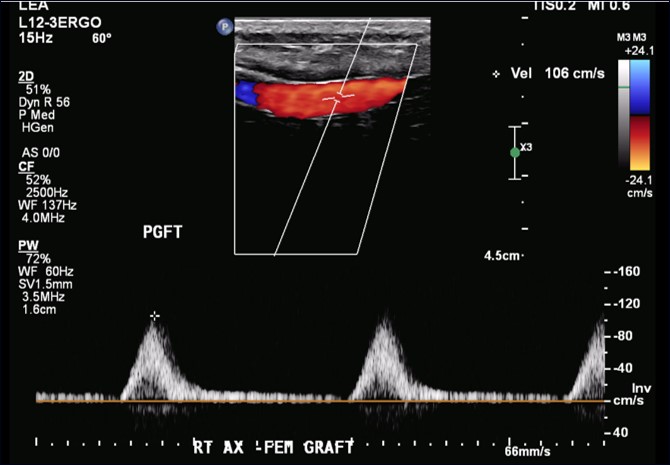
The Artix device time was 25 minutes. The patient tolerated the procedure well without complications and was discharged 2 days later. Follow up 1-month arterial duplex demonstrated graft patency, and the patient had no new symptoms of limb ischemia (Figure 5).
Discussion
This case demonstrates successful hybrid revascularization of an occluded axillary-profunda bypass graft. Mechanical thrombectomy with Artix restored flow by resolving the large thrombus burden, circumventing the need for graft replacement surgery. Patch profundoplasty was performed to treat a chronic focal distal anastomotic stenosis for improved outflow. The short single-session procedure was completed without complications.
The graft had likely occluded one month prior to presentation, based on the patient’s earlier symptoms of right ankle sprain and paresthesia, and the chronicity of the extracted thrombus. The age of the occlusion rendered thrombolytic therapy ineffective due to its chronic nature.4 Additionally, the profunda was the primary pathway for flow to the lower limb, since the superficial femoral and common femoral arteries were chronically occluded. However, the profunda was chronically diseased, and a hybrid approach was pursued.
To salvage the graft, Artix was selected over traditional Fogarty balloon thromboembolectomy because its self-expanding element could achieve full apposition of the graft wall to engage wall-adherent thrombus. The element was critical in this case given the extent of the thrombus and the device’s ability to capture a significant amount with each pass. Artix removed extensive subacute thrombus on the initial pass and the remaining thrombus in three additional passes (Figure 3). The mixed age of the thrombus extracted is consistent with reports that Artix can effectively remove thrombus of varying size and chronicity in lower-extremity occlusions.5
The design of the device — including its working length — made it optimal for navigating through the entire graft, with the durability to withstand the mechanical stresses encountered during thrombus retrieval. These design elements reduced the need for additional interventions, shortened procedure time, and decreased the risk of graft damage or incomplete thrombus removal. Notably, no procedure-related issues occurred, and adjunctive thrombolytics were not required.
The hybrid procedure salvaged the occluded axillary-profunda graft, avoiding the need for more invasive graft revision or replacement surgery. Additional surgery is associated with longer recovery time and higher risk of in-hospital complications including stroke, myocardial infarction, major bleeding, and compartment syndrome.6 By utilizing Artix to clear the graft and profundoplasty to improve the distal anastomotic focal stenosis and outflow for the revascularized graft, the existing graft was preserved and its long-term patency enhanced. The graft has remained patent without need for reintervention at follow-up. Additionally, the patient retained future treatment options in the event of recurrent thrombosis or graft failure. Given that he had undergone numerous previous revascularizations, this hybrid procedure aligns with a stepwise approach to limb salvage in the acute setting. Rather than committing to a complete bypass revision immediately, this strategy allows for conservative graft management, delaying or potentially avoiding more complex interventions unless necessary.
Conclusion
Hybrid revascularization with the Artix thrombectomy system and profundoplasty was safe and effective in salvaging an acute-on-chronically occluded axillary-profunda bypass graft. Mechanical thrombectomy with Artix efficiently removed a large subacute thrombus burden without complications, preserving the graft and avoiding the morbidity of more invasive graft revision or replacement surgery. Further investigation is warranted to validate and expand the application of Artix and this hybrid approach in both acute and chronic limb ischemia management.
References
1. Song P, Fang Z, Wang H, et al. Global and regional prevalence, burden, and risk factors for carotid atherosclerosis: a systematic review, meta-analysis, and modelling study. Lancet Glob Health. 2020; 8(5): e721-e729.
2. She K, Zhang X, Yin J, et al. Case report: lateral axillary-profunda femoris artery bypass for acute lower limb ischemia due to thrombosis after bilateral axillofemoral bypass. J Cardiothorac Surg. 2020; 15(1): 206.
3. Bjorck M, Earnshaw JJ, Acosta S, et al. Editor's choice - European Society for Vascular Surgery (ESVS) 2020 clinical practice guidelines on the management of acute limb ischaemia. Eur J Vasc Endovasc Surg. 2020; 59(2): 173-218.
4. Arnoldussen C, Notten P, Brans R, et al. Clinical impact of assessing thrombus age using magnetic resonance venography prior to catheter-directed thrombolysis. Eur Radiol. 2022; 32(7): 4555-4564.
5. Mond D, Salinas C, Parks J, et al. Setting the new standard for arterial thrombectomy: introducing Artix, a dual aspiration and mechanical thrombectomy solution designed to address a broad spectrum of arterial thrombus cases. Endovascular Today. 2025; 24(1): 8. https://evtoday.com/articles/2025-jan/setting-the-new-standard-for-arterial-thrombectomy
6. Kolte D, Kennedy KF, Shishehbor MH, et al. Endovascular versus surgical revascularization for acute limb ischemia: a propensity-score matched analysis. Circ Cardiovasc Interv. 2020; 13(1): e008150.
Find More:
Renal Denervation Topic Center
Cardiovascular Ambulatory Surgery Centers (ASCs) Topic Center
Grand Rounds With Morton Kern, MD
Peripheral Artery Disease Topic Center
Go to Cath Lab Digest's Current Issue
Go to the Journal of Invasive Cardiology Issue