Evaluating Superficial Venous Disease: When and How to Assess for Deep Venous Obstruction
Key Summary
- The evaluation of patients presenting to superficial venous practices whose symptoms are discordant with duplex findings (eg, significant edema/claudication without reflux, recurrent ipsilateral deep vein thrombosis, pelvic symptoms) are discussed.
- Clinical “red flags” are described that should prompt assessment for proximal deep venous obstruction and a diagnostic pathway using duplex ultrasound (eg, loss of common femoral vein phasicity) followed by targeted cross-sectional imaging.
- Recognition of deep venous obstruction can change treatment sequencing, set realistic expectations, and explain recurrence or incomplete response after superficial interventions; limits include imaging availability and protocol quality. Next steps emphasized are maintaining a systems-based evaluation and applying guideline-supported imaging in selected patients.
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Vascular Disease Management or HMP Global, their employees, and affiliates.
VASCULAR DISEASE MANAGEMENT. 2026;23(2):E19-E20

UNC Health, Chapel Hill, North Carolina
At the 2025 VEITHsymposium, Gloria Salazar, MD, FSIR, an interventional radiologist at UNC Health in Chapel Hill, North Carolina, addressed a critical and often underrecognized component of venous disease evaluation: identifying when superficial venous pathology may be a marker of underlying deep venous obstruction. In her presentation, “When Evaluating Superficial Disease, When And How Do You Look For Deep Venous Obstruction?”, Dr Salazar emphasized the importance of maintaining a comprehensive, systems-based approach to venous assessment, particularly in patients whose symptoms or clinical course do not align with typical superficial venous findings.
In this interview, Dr Salazar discusses the clinical red flags that should prompt further investigation for deep venous obstruction, outlines her diagnostic strategy, and explains how recognizing proximal disease can fundamentally alter treatment planning and patient expectations. She also shares key takeaways for clinicians seeking to improve outcomes by integrating deep and superficial venous evaluation into everyday practice.
What are some of the key clinical indicators or patient presentations that should prompt a clinician to investigate for deep venous obstruction when assessing superficial venous disease?
That's a very important question when you are running a superficial venous practice and you're trying to figure out the best way to approach the patient. In patients that have recurrent deep venous thrombosis in the same limb, pelvic symptoms, or they have symptoms that are really not matching the Doppler ultrasound findings—for example, somebody who does not have any superficial venous reflux and they have significant edema and venous claudication—I start thinking about a more proximal problem in these patients. I would usually order cross-sectional imaging to evaluate for compression or even post-thrombotic changes, particularly in patients with deep venous thrombosis history.
Could you walk us through your preferred diagnostic approach for identifying deep venous obstruction, including which imaging modalities or techniques you find most effective and why?
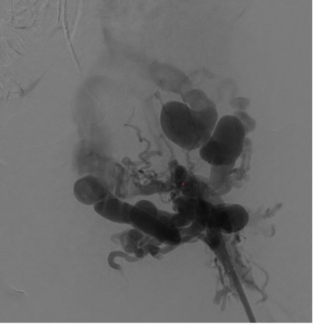
That is a very important question, mostly because of health care utilization. In the United States, we have overuse of cross-sectional imaging for other reasons. Therefore, other than the duplex ultrasound to evaluate for superficial venous disease, what I typically do before I even see the patient in consultation, is to look for cross-sectional imaging in the case that could potentially lead me to investigate compression before the patient even comes in. But the cross-sectional imaging is not always available and performed in a manner that is tailored for the protocol for the venous phases, for example. So in those situations, when I order the superficial ultrasound, if there's any finding in the duplex, for example, lack of venous phasicity in the common femoral vein, that is an indication to me that there's more proximal problem in the iliac vein.
Other ways of thinking about ordering the cross-sectional imaging is in patients who that have additional symptoms, as I mentioned before. Now, most patients would undergo computed tomography (CT) venography, which is essentially a CT scan that is less than 5 minutes protocol, you get into the scan and then they time the contrast bolus to be done in the venous phase for us to look for obstruction. But there are centers of excellence with imaging protocols at magnetic resonance imaging (MRI) that actually can do a very good job in evaluating the venous system. The difference for the patient with an MRI and a CT scan, other than the length of the exam—because it's faster to do a CAT scan—is in patients who have claustrophobia, so maybe the MRI is not a good option. So you just have to talk to the patient. For me, it's easier to just say CT scan venography, but certainly there are other ways to evaluate it in different centers, depending on where you are.
How does recognizing an underlying deep venous obstruction change the management or treatment strategy for patients with superficial venous disease?
When I started my career, I treated a lot of patients with superficial disease. And what I noticed is there is a subset of patients that consistently have recurrence or lack of full improvement of symptoms that I would expect for a treatment. And I'm talking 20 years ago. In that type of patient population that I saw about 20% had some compression higher up that I would diagnose with cross-sectional imaging. I started ordering myself additional imaging, to get a selection of patients that I knew potentially could have compression; but essentially, the way that it helps is you can fully describe to the patient the expectations and what they should look for in the future, so in my consultation, for example, even when I don't have any imaging, let's say I'm seeing a patient for the first time, I always tell them there's a subset of patients who may require a CT scan or an MRI ,and these patients will benefit from having the full evaluation to justify the study because they can have a compression that sometimes needs to be treated first, or needs to be followed up, to ensure a full improvement of the symptoms. That is how I think this whole concept of full evaluation of deep and superficial systems comes to be important, because it is about patient outcomes and reducing the quality of life because you don't look for central obstruction in this situation.
What is the main message you want attendees to take away from your presentation, something they can apply immediately in their own evaluation and treatment of venous disease?
The main message we are doing vascular disease in general is not to just focus on one thing, to be open minded for different presentations and different diagnosis. Yes, a majority of patients with varicose veins will have superficial venous reflux, but there's a subset of patients who have presentations that are beyond just the superficial. For me, in terms of being an educator, it's important for me to convey the message that there is definitely evidence that supports ordering cross-sectional imaging based on the guidelines for patients who have a history of thrombosis or a history of worsening venous symptoms or pelvic symptoms in which you will think about a central obstruction. n