Beyond the Rash: Targeted Strategies for Skin Toxicities in Oncology
At Dermatology Week 2025, Blair Allais, MD, brought clinical clarity to one of oncology’s most frustrating complications: skin toxicities. In her session, “Navigating Skin Toxicities in Oncology: Identification and Management,” Dr Allais moved beyond the basics, outlining thoughtful, patient-centered strategies to tackle acneiform eruptions, immunotherapy-induced rashes, and even blistering diseases—all without compromising cancer care.
“We see the whole spectrum of dermatology in these patients,” she said, emphasizing that proper identification is just as important as treatment.
Dr Allais began with a practical refresher on acneiform eruptions caused by estimated glomerular filtration rate inhibitors, which can affect up to 80% of patients. Emphasizing prevention, she encouraged early moisturization, broad-spectrum sunscreen, topical steroids, and preemptive doxycycline. “Prevention is paramount,” she said. “These rashes correlate with tumor response, and patients need to hear that.”
Next, she turned to toxic erythema of chemotherapy, a sweat-driven reaction often seen in folds and intertriginous zones. Her key advice? Cool it down. “Avoid warm blankets, laptops, and heating pads,” she said, noting that even something as simple as wiping down with cold paper towels after infusion can make a difference.
One of the most exciting updates was the novel use of high-dose vitamin D. Dr Allais cited recent findings showing rapid improvement with 100,000 IU doses of oral D2—an easy intervention that has shown promise in chemo-induced skin toxicity. “It’s very safe,” she noted, “but use caution in patients with renal impairment.”
Shifting into immune checkpoint inhibitor (ICI)-induced rashes, Dr Allais walked through real-world scenarios and her evolving approach to systemic steroids. The key takeaway? Be thoughtful. “Use the lowest dose for the shortest course and be mindful of the first 50 days.”
For morbilliform eruptions, she recommends ruling out antibiotic triggers, applying high-potency topicals with a soak-and-smear technique, and reserving prednisone for more severe cases. She reminded the audience that many ICI rashes are self-limited but counseling patients that they may recur is crucial.
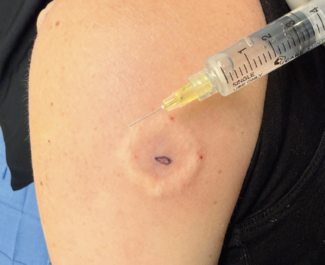
The session then explored more complex terrain: bullous pemphigoid, which appears more frequently in ICI-treated patients and often results in discontinuation of life-saving therapies. But there is hope. “Dupilumab appears to be safe and effective,” she said, referencing new data showing high response rates without compromising cancer outcomes.
She shared a straightforward algorithm: start with topicals, introduce biologics early (dupilumab or omalizumab), and consider intravenous immunoglobulin for rapidly progressive cases. Notably, she has moved away from antibiotics altogether, largely due to microbiome concerns.
And speaking of microbiomes, Dr Allais ended with a timely reminder: fiber matters.
She highlighted research showing differences in gut flora between ICI responders and non-responders, and how antibiotics can impair survival. Her practical advice? “Beans and greens. Every day.”
For more meeting coverage, visit the Dermatology Week newsroom.
Maximize your experience by adding up to 90 days of on-demand access. Find the package that works for you. Upgrade here.
Reference
Allais B. Navigating skin toxicities in oncology: identification and management. Presented at: Dermatology Week; May 14–16, October 22–25, 2025; Virtual.