Resolution of Nummular Eczema With Mupirocin Monotherapy
Nummular eczema (NE), also known as nummular dermatitis, is a chronic inflammatory skin condition characterized by coin-shaped plaques that are intensely pruritic and often scaly. These lesions commonly appear on the extremities and trunk and are associated with xerosis and impaired skin barrier function. Although the precise etiology of NE remains unclear, it is believed to arise from a combination of intrinsic factors, such as immune dysregulation, and extrinsic triggers, including irritants, environmental factors, and microbial colonization.1,2
Emerging evidence suggests that Staphylococcus aureus plays a significant role in the pathogenesis of NE. S. aureus can exacerbate inflammation through the production of superantigens and proteases, disrupting the skin barrier and triggering immune responses.3 Elevated levels of S. aureus colonization have been observed in lesional skin compared to unaffected areas, correlating with increased disease severity in NE and related conditions like atopic dermatitis (AD).4 The shared immune profile of NE and AD, characterized by Th2- and Th17-mediated responses, further supports the role of microbial factors in NE pathophysiology.5
Standard treatment for NE includes mid- to high-potency topical corticosteroids to reduce inflammation and emollients to restore the skin barrier. Antibiotics are typically reserved for cases with secondary bacterial infection or impetiginization. However, the potential of antimicrobial agents as therapeutic adjuncts is increasingly being explored, particularly in patients where microbial colonization may drive disease progression.
This case highlights the rapid resolution of NE with mupirocin monotherapy, challenging traditional treatment paradigms and emphasizing the need to explore bacterial contributions to NE progression.6,7
Case Presentation

A 77-year-old man with no significant dermatologic history presented to the clinic with a several-month history of pruritic, scaly, and crusted plaques localized to his right lower leg. He denied pain, systemic symptoms, and any history of asthma or seasonal allergies. Despite attempts to wash and scrub the lesions with soap, he noted no improvement in symptoms or appearance. The patient also reported that he had not used any moisturizers or emollients on the affected area.
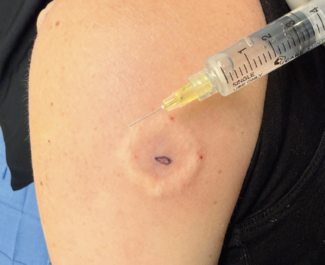
Physical examination revealed erythematous, scaly plaques with crusting, consistent with mild impetiginization (Figure 1). Based on these findings, a clinical diagnosis of nummular dermatitis was made. The patient was prescribed clobetasol 0.05% ointment twice a day and mupirocin 2% ointment 3 times a day for 2 weeks. He was also encouraged to moisturize the affected area with unscented lotions or emollients after showers.
At the 2-week follow up, the patient returned with near complete resolution of the plaques and complete resolution of pruritus. He disclosed that he had used only the mupirocin ointment, mistakenly assuming the clobetasol was an extra prescription intended for later use. Given the rapid response to antibacterial therapy alone, clobetasol was discontinued. The patient was instructed to continue mupirocin 3 times daily and maintain moisturization after showers for an additional 2 weeks or until the plaques resolved (Figure 2).

Three weeks later, the patient returned to the clinic with continued improvement of the plaques without any pain or pruritus (Figure 3). He was instructed to continue the same regimen and follow up in the clinic if symptoms worsened. Subsequent phone interviews with the patient confirmed complete resolution of the lesions without recurrence after several additional weeks of treatment.
Discussion
This case highlights the potential role of S. aureus in the pathogenesis and management of NE. Although S. aureus is well-documented in exacerbating inflammation in eczema-related conditions such as AD, our case brings to light its possible role as a primary driver in NE. The rapid resolution of plaques with mupirocin monotherapy suggests that bacterial colonization may play a more central role in NE pathogenesis than previously recognized. These findings build upon established evidence linking S. aureus colonization to increased disease severity and disrupted skin barrier function in eczema, indicating that it may represent a therapeutic target in NE.1,4,5
The effectiveness of mupirocin in this case raises important questions about the broader utility of antibacterial treatments in NE. While antibiotics are typically reserved for cases with secondary bacterial infections, this case suggests that targeted antibacterial therapy may also benefit patients with significant bacterial colonization. However, alternative factors must be considered. First, although the patient reported not using clobetasol, inadvertent application cannot be ruled out, given its known efficacy in reducing inflammation. Second, consistent moisturization may have restored the skin barrier, allowing for faster healing. Finally, spontaneous remission, a characteristic feature of NE’s relapsing-remitting nature, may have contributed to the outcome.

The use of antibacterial therapies in eczema, including NE, remains a topic of debate. Although evidence is limited, a 2019 Cochrane Review noted that combining topical antibiotics with corticosteroids provided only marginal benefits over corticosteroids alone in eczema treatment.8 In this case, the patient’s response to mupirocin alone underscores the need for controlled studies to better understand its role as a primary treatment option, particularly in cases with S. aureus colonization.
Our case also aligns with emerging evidence suggesting immunologic overlap between NE and AD, both of which are characterized by Th2- and Th17-mediated immune responses. These shared mechanisms may explain the observed efficacy of interventions targeting microbial factors.5 This highlights the importance of recognizing S. aureus colonization not merely as a secondary complication but as a potential driver of disease progression in some patients with NE.
While corticosteroids remain the cornerstone of NE management, this case emphasizes the need for an individualized approach that considers microbial involvement. Incorporating bacterial factors into the diagnostic and therapeutic framework for NE may lead to improved outcomes, particularly for patients with treatment-resistant or recurrent cases.
Conclusion
This case demonstrates the rapid resolution of NE with mupirocin monotherapy, suggesting a potential role of S. aureus colonization in disease pathogenesis and management. The patient’s response highlights the importance of considering microbial factors in NE and raises the possibility of targeted antimicrobial therapies as adjuncts or alternatives to corticosteroids in select cases.
Although the findings are compelling, the contribution of other factors, such as moisturization, inadvertent corticosteroid use, or spontaneous remission, cannot be ruled out. Further controlled studies are necessary to evaluate the broader applicability of antimicrobial treatments in NE and their impact on clinical outcomes. In the meantime, clinicians should consider the potential contribution of bacterial colonization when managing NE and adopt an individualized approach to treatment that balances efficacy with the risk of antibiotic resistance.
Linh H. Tran is a third-year medical student at the University of California Davis School of Medicine in Sacramento, CA, and a research assistant at VA Northern California Health Care System. Dr Dafinone is a PGY-1 resident at the Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas. Dr Isseroff is a distinguished professor in the department of dermatology at the University of California Davis School of Medicine and chief of dermatology at the VA Northern California Health Care System. Dr Sood is a professor of clinical dermatology in the department of dermatology at the University of California Davis School of Medicine and VA site director of the dermatology residency program at VA Northern California Health Care System.
Disclosure: The authors report no relevant financial relationships
References
1. Robinson CA, Love LW, Saleh HM, Farci F. Nummular dermatitis. In: StatPearls [Internet]. StatPearls Publishing; 2024.
2. Jiamton S, Tangjaturonrusamee C, Kulthanan K. Clinical features and aggravating factors in nummular eczema in Thais. Asian Pac J Allergy Immunol. 2013;31(1):36-42.
3. Böhner A, Jargosch M, Müller NS, et al. The neglected twin: nummular eczema is a variant of atopic dermatitis with codominant TH2/TH17 immune response. J Allergy Clin Immunol. 2023;152(2):408-419. doi:10.1016/j.jaci.2023.04.009
4. Lee M, Van Bever H. The role of antiseptic agents in atopic dermatitis. Asia Pac Allergy. 2014;4(4):230-240. doi:10.5415/apallergy.2014.4.4.230
5. Gong JQ, Lin L, Lin T, et al. Skin colonization by Staphylococcus aureus in patients with eczema and atopic dermatitis and relevant combined topical therapy: a double-blind multicentre randomized controlled trial. Br J Dermatol. 2006;155(4):680-687. doi:10.1111/j.1365-2133.2006.07410.x
6. Kim WJ, Ko HC, Kim MB, Kim DW, Kim JM, Kim BS. Features of Staphylococcus aureus colonization in patients with nummular eczema. Br J Dermatol. 2013;168(3):658-660. doi:10.1111/j.1365-2133.2012.11072.x
7. Hepburn L, Hijnen DJ, Sellman BR, et al. The complex biology and contribution of Staphylococcus aureus in atopic dermatitis, current and future therapies. Br J Dermatol. 2017;177(1):63-71. doi:10.1111/bjd.15139
8. George SM, Karanovic S, Harrison DA, et al. Interventions to reduce Staphylococcus aureus in the management of eczema. Cochrane Database Syst Rev. 2019;2019(10):CD003871. doi:10.1002/14651858.CD003871.pub3