Transradial Access Shifts the Paradigm in Treating Chronic Limb-Threatening Ischemia

Medical University, Graz, Austria
During Thursday afternoon’s “How I Would Do It” session, Marianne Brodmann, MD, from the Division of Angiology at the Medical University of Graz in Austria, delivered a detailed update on how she employs radial artery access to manage chronic limb-threatening ischemia.
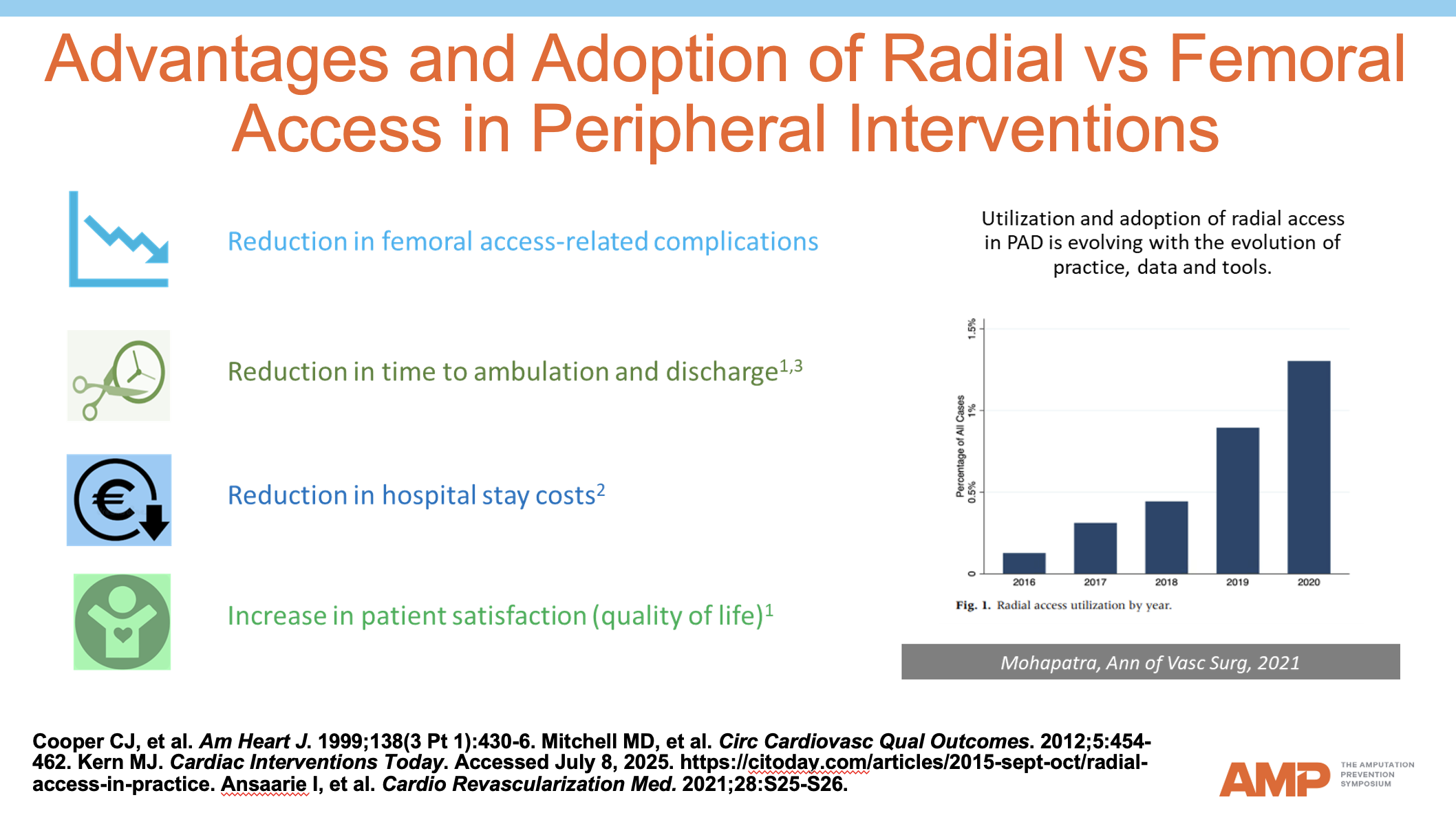
Historically, most peripheral endovascular procedures have relied on transfemoral access. Available evidence now challenges that paradigm: across 37 studies involving 70,882 patients, only 2,616 interventions were performed via the radial artery, yet the aggregated data revealed a procedural failure rate of just 3.9 % and significantly fewer access-site complications and minor bleeds compared with femoral access.
To address gaps specific to peripheral disease, Dr Brodmann highlighted her team’s prospective RADIANCY trial. Patients with a radial diameter of at least 2.5 mm underwent treatment of iliac or femoropopliteal lesions. Interim analysis demonstrated an “excellent” technical success rate, an absence of serious radial access-site complications or device-related mortality through discharge, and a sustained improvement in quality of life at 30 days. Final results are still pending.
In daily practice, Dr Brodmann begins with a straightforward algorithm. She weighs radial and femoral puncture options against patient factors such as frailty, obesity, ability to tolerate prolonged bed rest, and the presence of below-the-knee disease. Frail or obese patients who can receive a radial puncture but have multilevel lesions are first treated proximally (“inflow first”) with close monitoring of wound healing before deciding on further distal intervention.
Radial access resonates with patients familiar with transradial coronary angioplasty and, importantly for older patients with CLTI, eliminates hours of post-procedure immobility. The field, however, still lacks purpose-built long shafts and appropriately sized adjunct tools for below-the-knee work, and Dr Brodmann urged industry partners to close this gap as adoption increases.











