The Pros and Cons of OBLs and ASCs

Accountable Physician Advisors and DocCentric Surgery Centers
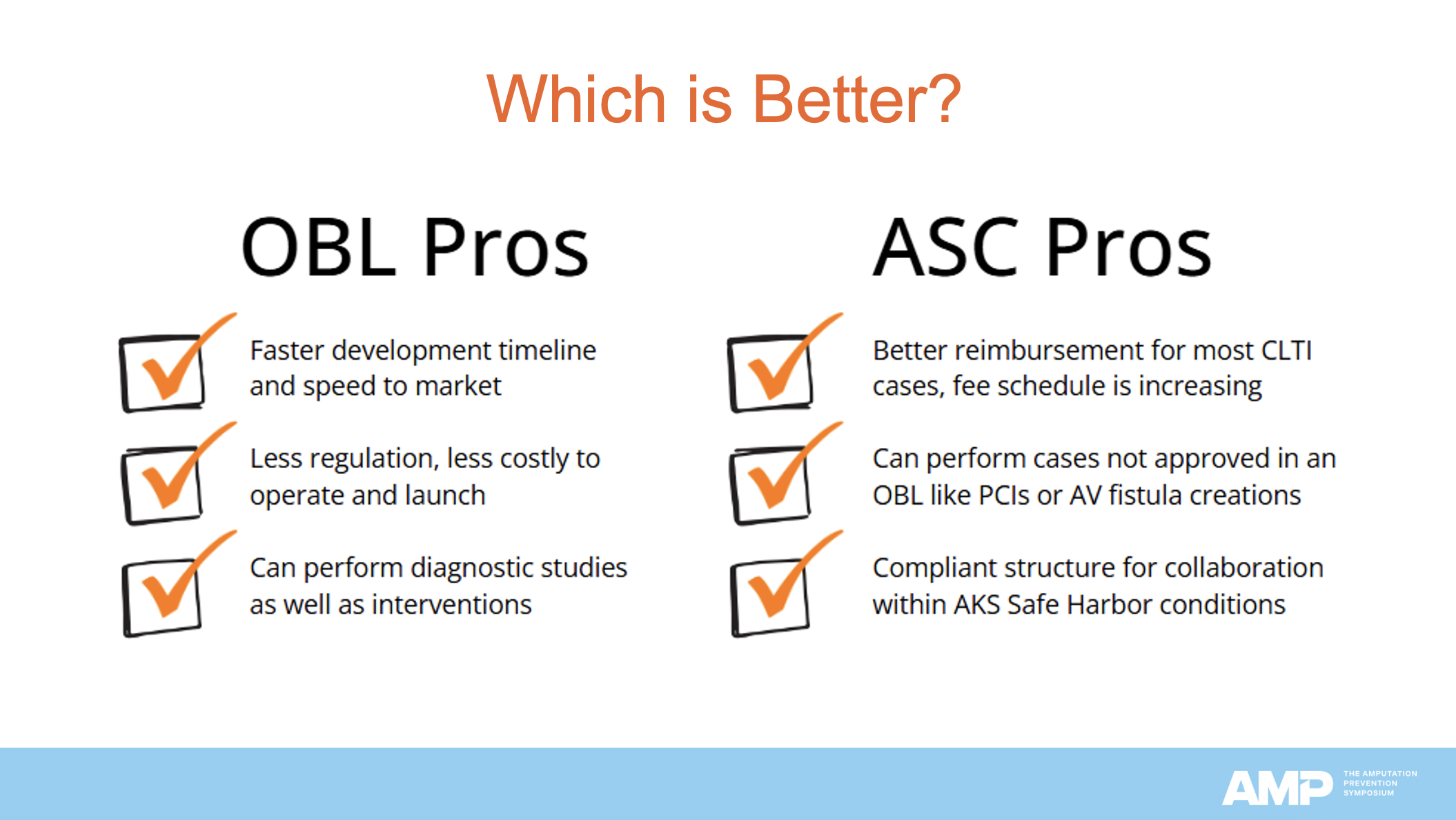
At the recent AMP Symposium in Chicago, Teri Yates, CEO of Accountable Physician Advisors and DocCentric Surgery Centers, delivered an in-depth presentation titled "OBL vs ASC? Pros and Cons". Drawing on her extensive experience in developing and managing physician-owned surgical facilities, Ms Yates provided a detailed comparison between office-based laboratories (OBLs) and ambulatory surgery centers (ASCs). Her presentation highlighted regulatory distinctions, facility requirements, financial considerations, and strategic implications for physicians choosing between the 2 models.
Ms Yates began by clarifying the fundamental distinctions. OBLs are typically part of a physician’s existing medical practice and are regulated primarily by state medical boards and, in some cases, state Departments of Health. Accreditation may or may not be required, depending on state regulations. By contrast, ASCs are standalone facilities regulated by the Centers for Medicare & Medicaid Services, state Departments of Health, and, in some cases, subject to Certificate of Need (CON) laws. Accreditation is mandatory for ASCs.
The facility design standards differ markedly between the 2 settings. OBLs often have more flexibility, with design decisions largely left to the physician, unless state-specific Department of Health rules or accreditation standards apply (as in Florida). In contrast, ASCs must conform to National Fire Protection Association (NFPA) Life Safety Code and Health Care Facilities Code, both of which impose strict structural, safety, and operational requirements.
Ms Yates stressed that OBLs offer a faster, less capital-intensive path to launch. They can often be retrofitted into existing spaces, require significantly lower construction costs, and can begin payer credentialing before opening. The typical launch timeline ranges from 6 to 12 months. ASCs, however, require either new construction or substantial renovation to meet NFPA Life Safety Code standards. Payer credentialing cannot begin until after an accreditation survey is complete, which extends the start-up timeline, about 18 to 24 months for construction and 6 to18 months for credentialing.
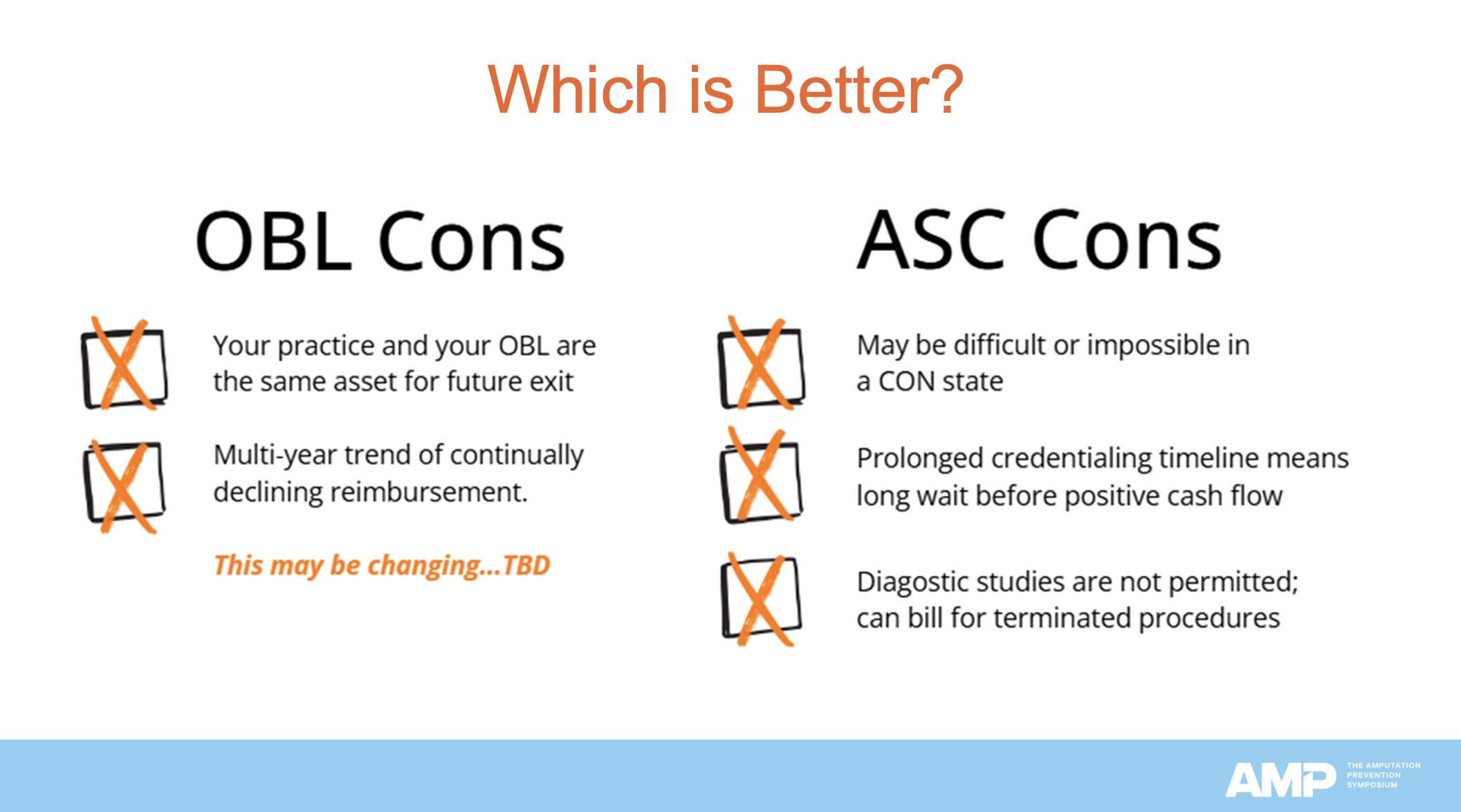
The choice between an OBL and an ASC is not one-size-fits-all, Ms Yates emphasized. In states with strict CON laws, an ASC may not be feasible. While ASCs involve a higher financial investment and more regulatory hurdles, they can offer superior long-term returns under current payment structures. ASCs are also distinct, saleable assets that can generate significant equity value, allowing physicians to maintain their private practices while monetizing the surgical facility. However, due to the high start-up costs, it was noted that banks often require physicians to work with ASC-specialized architects, contractors, and consultants to minimize financial and compliance risks.
Ms Yates provided practical, experience-based guidance for physicians navigating these complex choices, emphasizing that strategic planning, compliance awareness, and realistic financial forecasting are key to success in either model.











