May-Thurner Syndrome Masking Concomitant Arteriovenous Fistula: A Deadly Combination With Diagnostic and Therapeutic Challenges
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Vascular Disease Management or HMP Global, their employees, and affiliates.
VASCULAR DISEASE MANAGEMENT. 2025;22(5):E35-E38
Abstract
May-Thurner Syndrome is characterized by compression of the left common iliac vein by the overlying right common iliac artery. The vein is compressed between the hard bony spine and the stiff pulsatile artery, resulting in venous thrombosis, collateral formation, and limb swelling. It is rarely associated with a concomitant ilio-iliac arteriovenous fistula (AVF). There are only a few reports of this rare combination, which poses significant diagnostic challenges and increases complication risks. We present the case of a 56-year-old woman with left leg swelling and pain due to May-Thurner syndrome and an associated AVF that was successfully treated with endovascular techniques.
Introduction
May-Thurner syndrome was first described by R. May and J. Thurner in 1957.1 It is seen most commonly in women in their third to fifth decades. Patients present with varying symptoms of venous hypertension, which leads to swelling of the left leg with or without deep vein thrombosis (DVT). Rarely, it is associated with an arteriovenous fistula (AVF) between the adjacent right iliac artery and the left iliac vein. It is important to properly diagnose the combination, as treatment success is very much dependent on it. Whether to treat both conditions or just one is based on the individual presentation. We present a similar rare combination in a 56-year-old woman who was successfully evaluated and treated with endovascular techniques.
Case Report
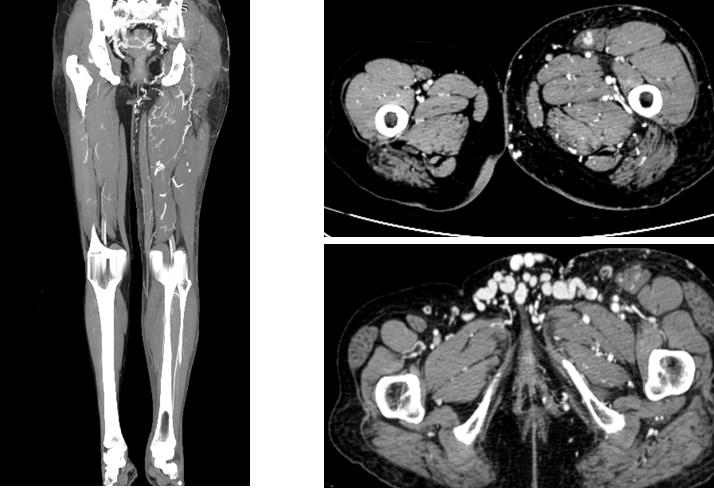
A 56-year-old woman presented with complaints of left lower limb swelling and pain for 6 months. Doppler examination 6 months earlier revealed acute DVT of the iliofemoral and popliteal veins, and the patient had been taking oral anticoagulants since then. She was taking 2 mg nicoumalone daily, with monitoring of the prothrombin time and international normalized ratio (INR) every 15 days. The previous few INRs were in the suboptimal range (<2). She continued to experience swelling in her left leg with heaviness and pain. As there was no relief with routine treatment, she was referred to our center for further evaluation and treatment. Initial venous Doppler showed recanalized left lower limb veins with no acute DVT. However, it failed to show the left common iliac vein (CIV) patency. A computed tomography (CT) venogram was done, which showed asymmetrical enlargement of the left lower limb with evidence of multiple collaterals in the bilateral inguinal and left thigh regions (Figure 1).
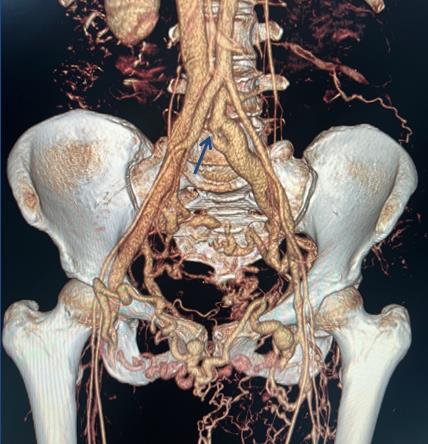
There was evidence of compression of the left CIV by the right common iliac artery (CIA). Near-total occlusion of the left CIV at its junction with the inferior vena cava is associated with dilatation of the prestenotic segment (Figure 2).
Abbreviation: AVF, arterioivenous fistula.
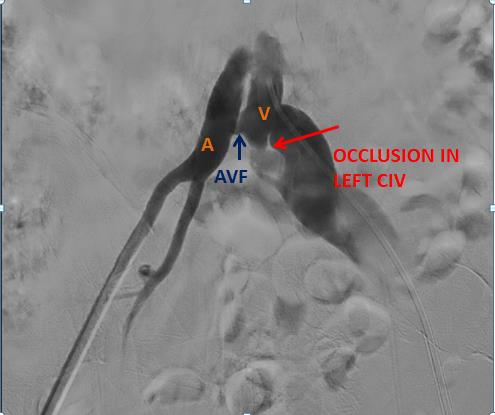
Communication between the right CIA and left CIV was seen, which is indicative of an AVF. Doppler was repeated, which confirmed high velocity reversed flow in the CIV. Digital subtraction angiography was completed under ultrasound guidance; the left common femoral vein was punctured and access was secured with a 7F sheath (Figure 3). Using a vertebral catheter (Glidecath, Terumo), the left CIV was cannulated and a venogram was obtained. It revealed an abrupt cutoff of the left CIV due to complete thrombotic occlusion, with multiple venous collaterals and retrograde filling of the left internal iliac vein and right CIV. Pressures were measured across the common iliac and external iliac veins.
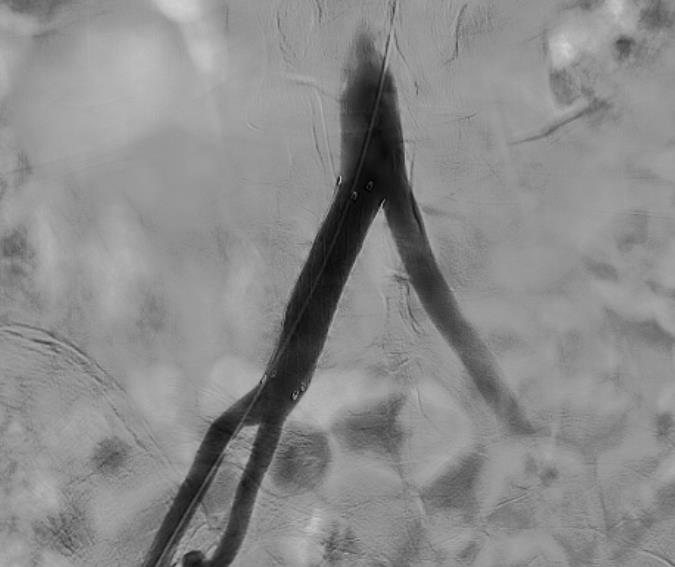
Under ultrasound guidance, the right common femoral artery was punctured, and access was secured with a 7F sheath. Using a vertebral catheter, an angiogram of the right CIA was performed, which revealed a high-flow fistula between the right CIA and left CIV at the level of the superior endplate of the L5 vertebra. A 7F sheath was exchanged for a 10F sheath. A 0.35” hydrophilic guide wire was passed across the aortic bifurcation, and a 10- x 40-mm covered stent graft was deployed with the cranial end of the stent below the aortic bifurcation and the caudal end above the CIA bifurcation. The check angiogram showed complete obliteration of the fistula track with nonvisualization of the collateral veins (Figure 4).
Pressures were recorded again in the left CIV. There was a significant drop in pressures, from 70/44 mm Hg to 14/10 mm Hg. As the venogram from the venous access did not reveal significant collateral filling, the CIV occlusion was left alone without recanalization. The next day, Doppler confirmed the absence of flow reversal in the left CIV. The patient was discharged after 2 days. Follow-up after a month showed a reduction in left limb swelling with no pain.
Discussion
May-Thurner syndrome is a condition wherein the left CIV is compressed between the underlying vertebral column and the overlying pulsating right CIA. These repetitive pulsations can cause endothelial damage to the vein, leading to thrombus formation and eventually DVT of the left leg.
Patients with May-Thurner syndrome account for at least 2% of patients evaluated for venous disorders of the leg, with 60% of patients with left lower limb DVT and 37% with isolated left lower limb swelling.2 In our patient, the initial Doppler scan failed to recognize the AVF. A multiphasic CT venogram revealed the fistula due to differential contrast densities in the left CIV in different phases. The arterial phase showed increased density in the left CIV, which was reduced in the later phases. Multiple dilated collaterals in the pelvis also indicated severe venous hypertension, more than that seen in simple May-Thurner syndrome. Post CT venogram, a Doppler scan was repeated by a senior radiologist, which showed high velocity reversed flow in the left CIV. Spectral Doppler showed turbulent arterial waveforms in the left CIV, which was confirmative of the existing fistula.
Proper diagnosis is critical for proper management of the patient. In most simple cases of May-Thurner syndrome, reconstruction of the occluded left CIV is the optimal treatment. However, in cases of May-Thurner syndrome complicated by concomitant AVF, treatment of the AVF will receive prime importance as the goal of treatment is reduction in venous hypertension. A fistula will result in more venous hypertension than a simple venous occlusion. Due to rich venous collaterals in the pelvis, venous hypertension will be less in occlusive cases. This can be better understood by a digital subtraction angiogram of the pelvic veins, which will optimally delineate all the collateral pathways in real time, whereas in a case of AVF, constant high-pressure flow from the artery to the vein will result in significant venous hypertension, causing dilatation and tortuosity of the draining veins. Hence, we ended up only closing the AVF in our case without recanalizing the occluded left CIV.
Endovenous therapies are increasing in numbers in recent years, and studies have shown 50% to 100% patency after 1 year.3,4 Link and Granchi, in their case of May-Thurner syndrome and AVF causing nonhealing ulcers of the leg, also ended up only treating the AVF with onyx liquid embolic agent and coils, followed by sclerotherapy of the varicose veins. Venous recanalization was not needed in their case as well.5
In another case of May-Thurner syndrome and AVF in an older woman treated by Shima and Shimada, the AVF was not treated due to technical difficulties. Only venous recanalization was enough in their case to relieve the limb swelling.6 The AVFs were small in their case, with no significant dilated collateral veins due to AVF; therefore, only venous recanalization was done.
In another case of May-Thurner syndrome with AVF, treated by Kim, Yeon, et al, only AVF embolization with coils and gelatin was sufficient to treat the patient.7
In the limited case reports available about this rare combination, AVF embolization was seen in all those cases where an AVF was a dominant component with more prominent dilated collateral veins. In cases where the AVF was the smaller or nondominant of the two, venous recanalization was done.
In our case, we chose to treat the AVF by using a covered stent in the right CIA as it was a simple and faster procedure compared with embolization by using different embolic materials. Every case is different, and proper study of the pathology is important in deciding the mode of treatment. n
Affiliations and Disclosures
Amithavikrama Kheda, MD; Sharath BM, DNB, RD; Vijayalakshmi Devi Bodagala, DNB, RD; and Neha Oruganti, MBBS, are from the Department of Radiodiagnosis, Sri Venkateswara Institute of Medical Sciences, Tirupati, Andhra Pradesh, India; and Sri Satyavathi Davuluri, MS, MCh, is from the Department of Cardiothoracic Surgery, Sri Venkateswara Institute of Medical Sciences, Tirupati, Andhra Pradesh, India.
Manuscript accepted April 29, 2025.
The authors report no financial relationships or conflicts of interest regarding the content herein.
Address for Correspondence: Amithavikrama Kheda, MD, Sri Venkateswara Institute of Medical Sciences, Alipiri Rd, Sri Padmavati Mahila Visvavidyalayam, Tirupati, Andhra Pradesh 517507, India. Email: amithavikrama@gmail.com
REFERENCES
1. May R, Thurner J. The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins. Angiology. 1957;8(5):419-427. doi:10.1177/000331975700800505
2. Huynh N, Gates L, Scoutt L, Sumpio B, Sarac T, Ochoa Chaar CI. May-Thurner syndrome and iliac arteriovenous fistula in an elderly woman. J Vasc Surg Cases Innov Tech. 2016;2(2):46-49. Doi: 10.1016/j.jvsc.2016.02.001
3. Taheri SA, Williams J, Powell S, et al. Iliocaval compression syndrome. Am J Surg. 1987;154(2):169-172. doi:10.1016/0002-9610(87)90172-3
4. Moudgill N, Hager E, Gonsalves C, Larson R, Lombardi J, DiMuzio P. May-Thurner syndrome: case report and review of the literature involving modern endovascular therapy. Vascular. 2009;17(6):330-335. doi:10.2310/6670.2009.00027
5. Link DP, Granchi PJ. Chronic iliac vein occlusion and painful nonhealing ulcer induced by high venous pressures from an arteriovenous malformation. Case Rep Radiol. 2011;2011:514721. doi:10.1155/2011/514721
6. Shima Y, Shimada T, Tanaka H, Kadota K. Iliac May-Thurner syndrome coexisting with arteriovenous fistula treated by endovascular therapy. SAGE Open Med Case Rep. 2020;8:2050313X20938222. doi:10.1177/2050313X20938222
7. Kim TH, Yeon JW, Kim HJ, Jang SK. Ilio-iliac arteriovenous fistula with May-Thurner syndrome: a case report. J Korean Soc Radiol. 2024;85(1):235-239. doi:10.3348/jksr.2023.0049











