Limb Salvage in Complex Femoropopliteal Occlusion
Successful Use of Percutaneous Transmural Arterial Bypass With the Detour System in Cases Doomed for Amputation
Successful Use of Percutaneous Transmural Arterial Bypass With the Detour System in Cases Doomed for Amputation
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Vascular Disease Management or HMP Global, their employees, and affiliates.
VASCULAR DISEASE MANAGEMENT. 2025;22(9):E60-E63
Abstract
Chronic limb-threatening ischemia due to complex femoropopliteal occlusive disease remains a formidable challenge, especially in patients with large stented segments creating hurdles for the entire inflow and outflow for transmural bypass. This manuscript describes the successful application of percutaneous transmural arterial bypass (PTAB) utilizing the Detour system (Endologix) as a limb salvage strategy for a patient with previously failed femoropopliteal bypass, recurrent failed stenting of the femoropopliteal system, and now complete occlusion of flow to the entire extremity. The PTAB technique allowed for the creation of a durable, minimally invasive arterial bypass, effectively restoring perfusion and preserving limb function. Our experience demonstrates that PTAB with the Detour system offers a viable alternative in anatomically complex and high-risk patients, with encouraging technical success and limb salvage rates, and acceptable safety profiles. These findings support the incorporation of PTAB into the armamentarium for limb salvage in patients otherwise facing inevitable amputation.
Case Report
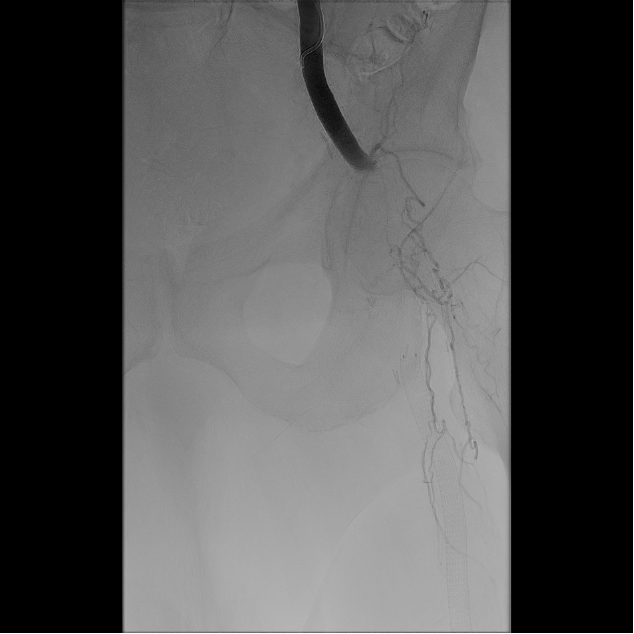
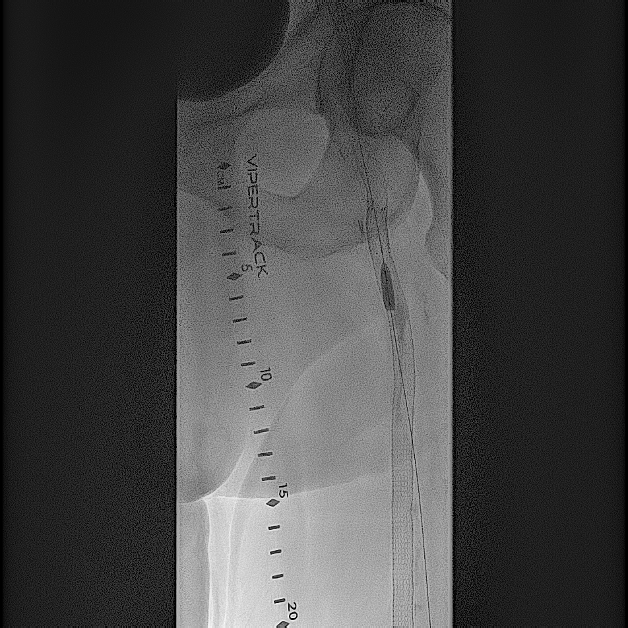
A 76-year-old White man with a medical history of hypertension, tobacco abuse, coronary artery disease, and coronary artery bypass grafting presented with a nonhealing wound of his left lower extremity. He had a previous history of stenting of the left superficial femoral artery (SFA) 8 years prior to presentation. He was noted to have complete occlusion of the left SFA and also abrupt occlusion of the left common and profunda femoral artery (Figure 1). The patient was offered an above-knee amputation, which he refused, and opted for endovascular intervention for revascularization of his entire left lower extremity.

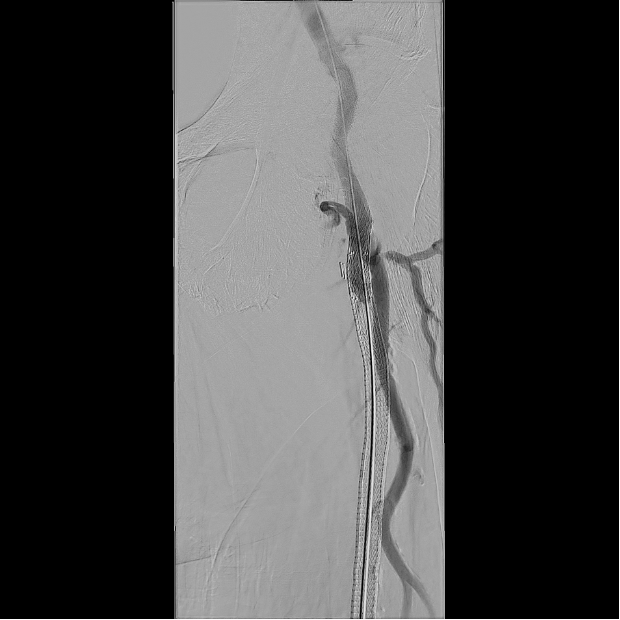
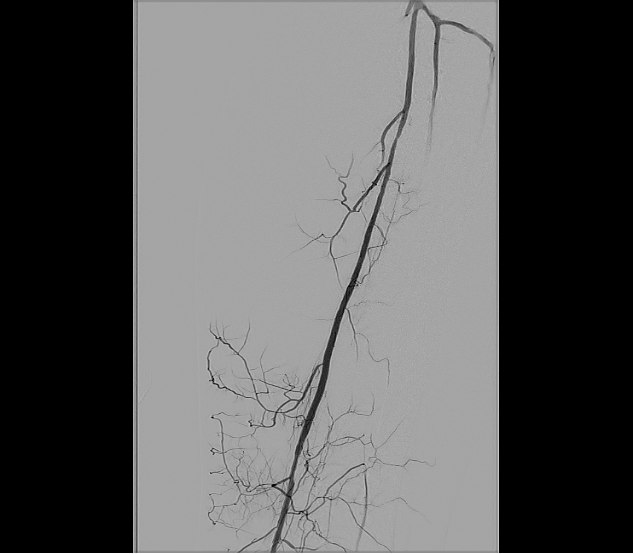
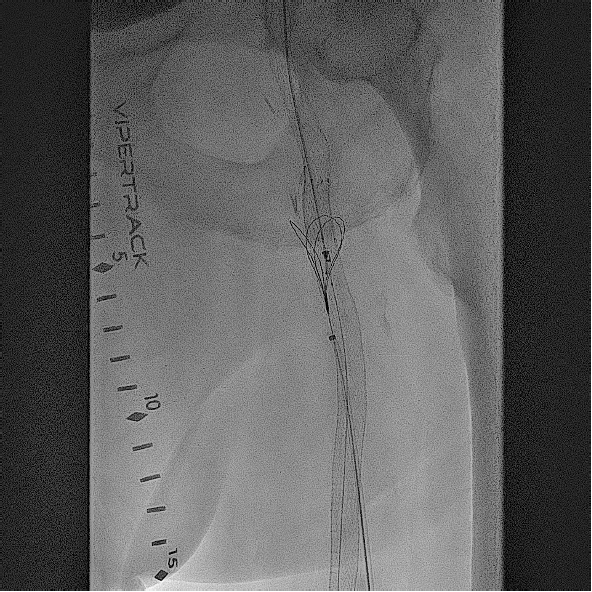
Based on his comorbidities, history of recurrent stenting of the left SFA, and an occlusion of the SFA over 200 cm, he was deemed to be an appropriate candidate for percutaneous transmural arterial bypass (PTAB). However, in order to establish long-term patency, we proceeded to gain posterior tibial artery access to identify a 3-vessel runoff (Figure 2). With this information, using the outline of the stents in left SFA and using a 0.018-in Glidewire Advantage (Terumo) and a 0.018-in Rubicon catheter (Boston Scientific), we were able to obtain access into the left profunda femoral artery (Figure 3). Despite multiple-balloon angioplasty, the recoil within the left common femoral artery (CFA) left little option but to place a 7.0-mm Eluvia stent (Boston Scientific), which was overlapped with the proximal stent in the left SFA (the profunda femoral artery was patent after balloon angioplasty; Figure 4).
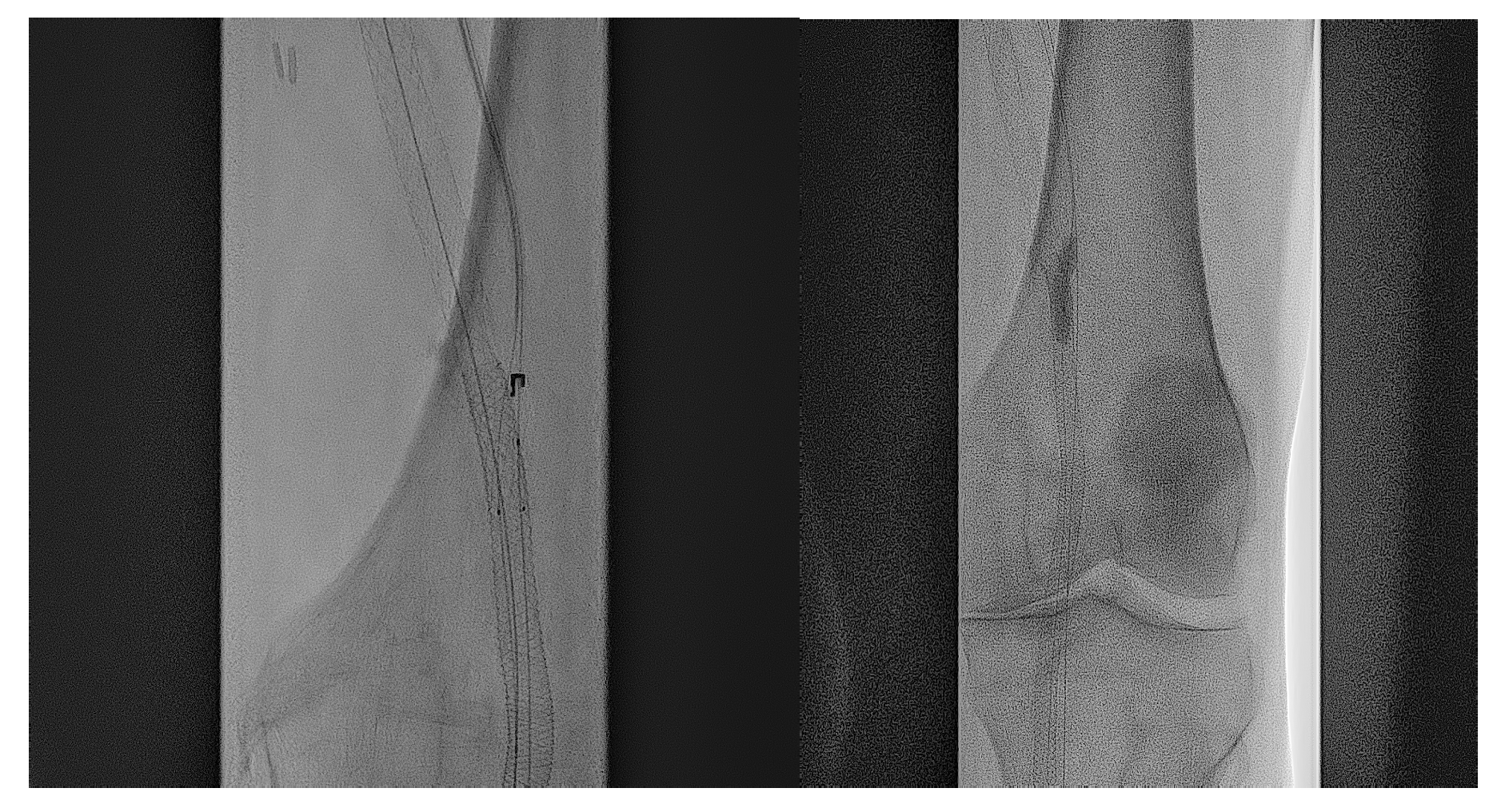
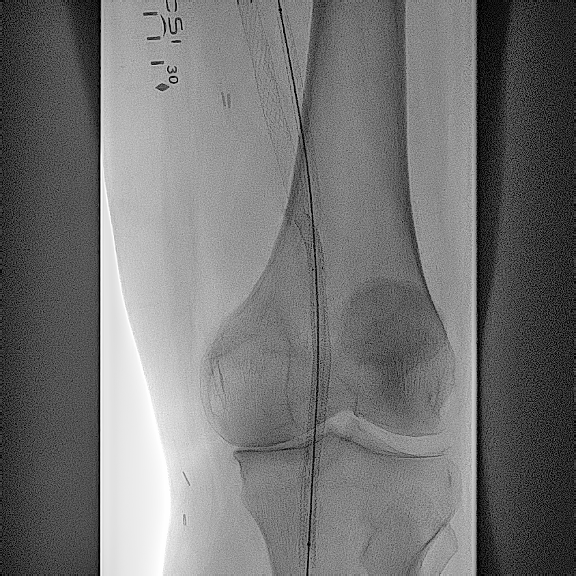


After gaining access into the SFA, the first step of crossing from the SFA into the femoral vein was done with the Endocross catheter (Endologix; Figure 5). Although it had to be done through stent struts, this proved to be fairly easily accomplished with minimal resistance. A 0.014-in Grand Slam wire (Asahi Intecc Medical) was snared from the Endocross to the femoral vein using a pre-existing snare. The crossover site was then dilated using a 5.0-mm Serranator balloon (Cagent Vascular; Figure 6), allowing for the Endocross to advance into the distal femoral vein for distal access into the P1 portion of the popliteal artery through a pre-existing Supera stent (Abbott Cardiovascular) with minimal resistance. This was pre-dilated with a 4.0-mm Coyote balloon (Boston Scientific) followed by a 5.0-mm Serranator balloon (Figure 7). After sufficient pre-dilatation, the Torus stents (Endologix) were placed from the distal anastomosis to proximal anastomosis (5.5 mm distally and 6.5 mm proximally; Figure 8) followed by post-dilatation with a 6.0-mm Mustang balloon (Boston Scientific; Figure 9). Repeat angiographic assessment showed good apposition and expansion of the stents and robust vessel runoff down to the foot (Figure 10). The patient’s wound did require transmetatarsal amputation but was spared an above-knee amputation. His wounds had shown sufficient healing 3 months from the principal procedure.
Discussion
Chronic limb-threatening ischemia (CLTI), the most severe form of peripheral arterial disease, poses a significant global health burden.1 CLTI is associated with chronic rest pain, nonhealing ulcers, or gangrene, and is estimated to affect approximately 1% to 1.5% of individuals age 50, with incidence rates increasing among older populations and those with comorbidities such as diabetes and smoking history.2 In patients with untreated or refractory CLTI, the risk of major amputation can reach up to 40% within 1 year of diagnosis.3 Moreover, both morbidity and mortality remain high despite advances in revascularization techniques.4 These realities underscore the pressing need for innovative strategies in limb salvage and revascularization.
The Detour PTAB is an innovative endovascular technique designed to restore blood flow in patients with complex femoropopliteal occlusive disease, particularly when traditional surgical or endovascular options are exhausted or not viable. Using a combination of specialized catheters, guidewires, and stent technology, PTAB creates a bypass channel by traversing from the SFA into the adjacent femoral vein, then re-entering the arterial system distal to the occlusion. This minimally invasive approach allows for limb salvage in high-risk patients, offering a crucial alternative in cases where extensive arterial disease or previous interventions limit conventional therapies.
This case highlights the value of PTAB using the Detour system in a patient who was left with no endovascular or surgical approach to correction. He had been seen by vascular surgery and was not felt to have a viable venous conduit. The complexity of this case was magnified by the presence of associated common femoral and profunda femoral occlusion, limiting assessment of runoff via this angiographic route. Therefore it was pertinent to establish the presence of a 3-vessel runoff prior to even proceeding with restitution of flow in the above-knee segment. Clearly, with limited options for the common femoral and profunda femoral vessels, stenting of the CFA was considered a reasonable (albeit not ideal) option in this “no-option” case. Establishing robust inflow paved the way for access into the SFA.
The presence of stents across the entire length of the femoropopliteal system was an obstacle both with respect to crossing with the Endocross but also with respect to maintaining sufficient expansion and patency of the Torus stents. We found the Serranator balloon very useful in creating the tissue plane needed for stent expansion and also facilitating Endocross delivery. At the end, post-dilatation angiographic flow seemed sufficient and unimpeded. We opted to maintain anticoagulation with aspirin, clopidogrel, and rivaroxaban, 2.5 mg bid, to prevent acute thrombosis and facilitate endothelialization.
The Detour2 study was a prospective, multicenter trial assessing the safety and efficacy of the Detour system in patients with long-segment SFA occlusions, many of whom were considered poor candidates for conventional surgical bypass due to comorbidities or lack of viable venous conduits. The study included over 200 patients with CLTI or severe claudication and mean lesion lengths exceeding 30 cm—populations comparable to the challenging scenario described in the present case.5
Conclusions
This case was unique both with respect to complexity of access but also of crossing with the PTAB system. The presence of Supera stents across both inflow and outflow provided a challenge to entry and pre-dilatation but ultimately, with sufficient vessel prep, was attainable. Primary patency rate at 12 months in the Detour2 study was approximately 72% at 12 months.5 Six-month angiography revealed full patency in this patient. This case paved the way for utilization of this technology in areas of limb salvage where previously we were limited to conventional endovascular or surgical options. It exemplifies the novelty of this technology, giving both patients and providers a third choice. n
REFERENCES
1. Criqui MH, Aboyans V. Epidemiology of peripheral artery disease. Circ Res. 2015;116(9):1509-1526. doi:10.1161/CIRCRESAHA.116.303849
2. Duff S, Mafilios MS, Bhounsule P, Hasegawa JT. The burden of critical limb ischemia: a review of recent literature. Vasc Health Risk Manag. 2019;15:187-208. doi:10.2147/VHRM.S209241
3. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FGR, TASC II Working Group. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg. 2007;45(Suppl S):S5-S67. doi:10.1016/j.jvs.2006.12.037
4. Cacoub PP, Abola MTB, Baumgartner I, et al; REACH Registry Investigators. Cardiovascular risk factor control and outcomes in peripheral artery disease patients in the Reduction of Atherothrombosis for Continued Health (REACH) registry. Atherosclerosis. 2009;204(2):e86-e92. doi:10.1016/j.atherosclerosis.2008.10.023
5. Lyden SP, Soukas PA, De A, et al; DETOUR2 Trial Investigators. DETOUR2 trial outcomes demonstrate clinical utility of percutaneous transmural bypass for the treatment of long segment, complex femoropopliteal disease. J Vasc Surg. 2024;79(6):1420-1427.e2. doi:10.1016/j.jvs.2024.02.004
Affiliations and Disclosures
John H. Shao, MD; John Lee, MD; and M. Haris U. Usman, MD, MS, are from Newark Beth Israel Medical Center in Newark, New Jersey.
Disclosures: Dr Usman has been a consultant for Endologix. Dr Lee and Dr Shao report no financial relationships or conflicts of interest regarding the content herein.
Manuscript accepted August 26, 2025.
Address for Correspondence: Mohammed Haris Umer Usman, MD, Newark Beth Israel Medical Center, 201 Lyons Ave, Newark, NJ 07112. Email: harisumermd@gmail.com











