Aortic Endograft and Femorofemoral Bypass in a Patient With Acute Aortic Occlusion Post-COVID Respiratory Disease, Atrial Fibrillation, and Vocal Cord Cancer With Chronic Left External Iliac Occlusion
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Vascular Disease Management or HMP Global, their employees, and affiliates.
VASCULAR DISEASE MANAGEMENT. 2025;22(10):E88-E91
Abstract
Respiratory infection due to COVID-19 has been associated with thrombotic events such as deep vein thrombosis, pulmonary embolism and, to a lesser extent, arterial thrombosis. Cases of acute aortic occlusion (AAO) in patients with COVID-19 have been previously described in the literature. AAO has been associated with a 30-day mortality rate of 20%, an overall mortality rate of 60%, morbidity ranging from 30% to 74%, and a 30% risk of limb loss. Historically, surgical treatment has included aortobifemoral bypass, extra-anatomic bypass (axillobifemoral), bilateral inguinal thrombectomy, pharmacomechanical thrombectomy, and thrombolysis. Endovascular techniques provide new tools and therapeutic options, particularly for patients at high surgical risk. In selected cases, these may represent the only therapeutic option. However, optimal surgical management has not been standardized. We report the case of a 64-year-old man with bilateral acute ischemia caused by AAO in the context of COVID-19 pneumonia, new-onset atrial fibrillation, and a history of vocal cord cancer. The patient underwent a hybrid procedure under local anesthesia: femoral embolectomy, aortic endograft placement, and femorofemoral bypass due to chronic left external iliac occlusion. This approach is safe, effective, and applicable to patients at high surgical risk and/or those contraindicated or unable to undergo intubation.
Introduction
Respiratory infection by the COVID-19 virus has been shown to be a risk factor for thromboembolic events.1 It has been associated with episodes of deep vein thrombosis (DVT), pulmonary embolism (PE)2 and, to a lesser extent, arterial thrombosis.3 Acute aortic occlusion (AAO) cases and series have been described in the literature in COVID-positive patients, showing a high morbidity and mortality rate.1,4,5 Recent developments and refinements in endovascular techniques and devices have introduced a new therapeutic option that is now regarded as both acceptable and the preferred treatment in selected cases.6
We present the case of a 64-year-old man with bilateral acute ischemia due to AAO, in the context of bilateral COVID-19 pneumonia, new-onset atrial fibrillation (AF), and a medical history of vocal cord cancer. The patient was treated by a hybrid procedure under local anesthesia: bilateral femoral embolectomy, aortic endograft, and right-to-left femorofemoral bypass resulting from a chronic occlusion of the left external iliac artery (LEIA).
Case Report
A 64-year-old man, an active smoker with a history of 1 pack per day, type 2 diabetes mellitus, and a recent diagnosis of squamous cell carcinoma of the vocal cords, presented to the emergency department (ED) with odynophagia and fever. He was diagnosed with bilateral pneumonia due to COVID-19 without clinical or laboratory warning signs and was discharged with symptomatic treatment.
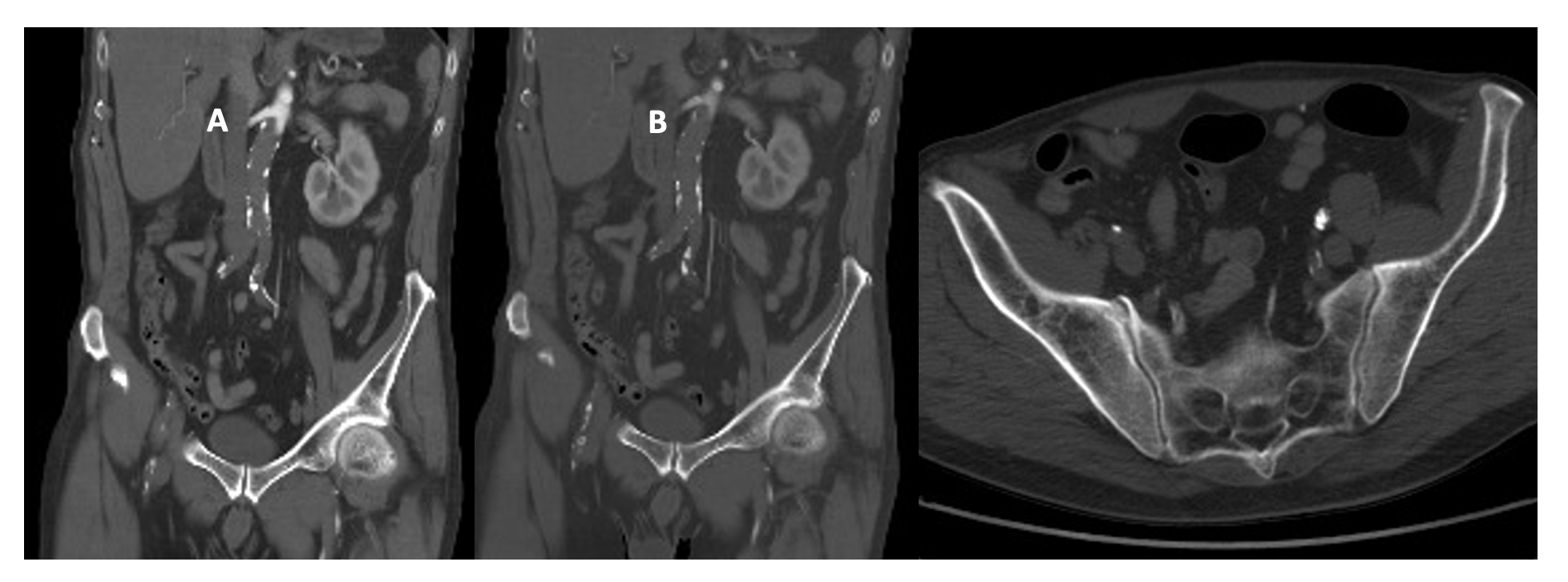
He presented to the ED 5 days later with pain, paralysis, and bilateral anesthesia of the lower limbs of 3 hours' duration, presenting with pulselessness at any level, with cutaneous lividity in the abdomen and both thighs on physical examination. The electrocardiogram showed new-onset AF, and an aorta computed tomography (CT) scan revealed complete acute occlusion of the infrarenal aorta and bilateral iliac arteries, along with chronic occlusion of the LEIA (Figure 1).
This case took place during the COVID pandemic and our center lacked access to ventilators. Added to the patient’s respiratory condition, the procedure was performed under local anesthesia and deep sedation. The patient underwent right transfemoral embolectomy and unsuccessful attempts at left transfemoral embolectomy due to chronic occlusion of the LEIA.
Given the possibility of isolating thrombotic debris from the infrarenal aorta and both iliac axes, a 16 x 10 aortic endograft (Medtronic) was implanted, extending to the right common iliac artery with a Viabahn VBX 8 x 79 stent graft (Gore), a right-to-left femorofemoral bypass using 8-mm ringed polytetrafluoroethylene catheter to restore vascularization to the left leg, and bilateral fasciotomies of the anterior and posterior compartments.
During surgery, sinus rhythm was restored. The patient was extubated in the operating room with bilateral pedal pulses and was transferred to the intensive care unit (ICU) on anticoagulant therapy (low-molecular-weight heparin, 80 mg every 12 hours) and single antiplatelet therapy (aspirin, 100 mg) without the need for vasopressor medications.
During the postoperative period, the patient required a 5-day stay in the ICU due to renal function deterioration resulting from rhabdomyolysis (elevated creatine phosphokinase, creatinine, and urea levels), which necessitated hydration and monitoring of urine output, along with the recovery of respiratory function.
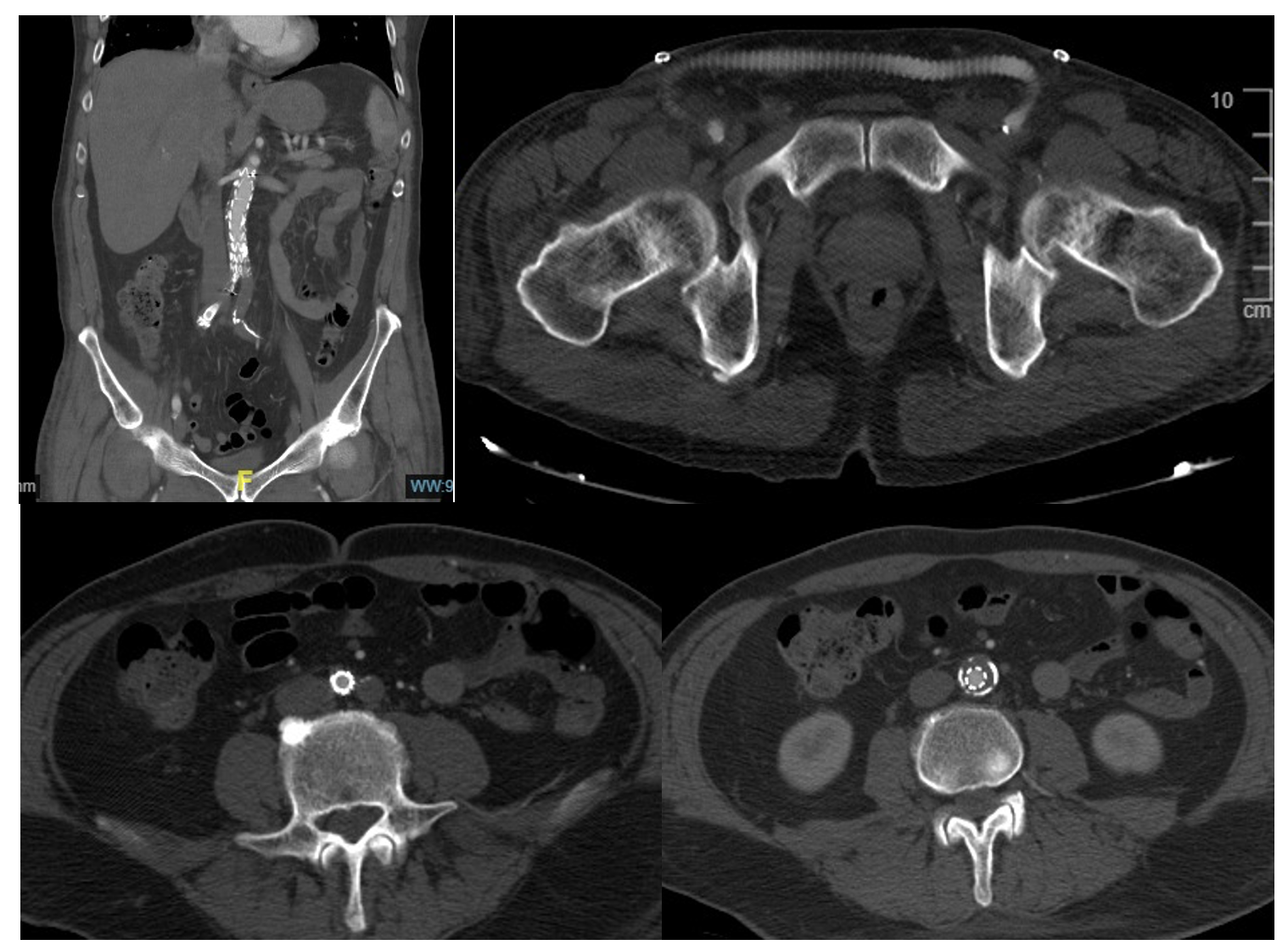
The patient was transferred to the hospital ward and discharged on the 8th postoperative day with closed fasciotomies and preserved bilateral pedal pulses. During the hospitalization, a follow-up CT scan for his bilateral pneumonia showed a patent endograft without leaks (Figure 2). Two months later, the patient received treatment for his vocal cord carcinoma from the otolaryngology department through radiotherapy. In the most recent outpatient follow-up 1 year ago, he maintained distal pulses, and ultrasound evaluation showed the endograft without leaks and patent femorofemoral bypass.
Discussion
A high percentage of patients with respiratory infections due to COVID-19 experience complications related to thrombotic events, primarily venous (DVT and PE) and, to a lesser extent, arterial.3 In our center, during the COVID pandemic, we published a case series of 3 patients with arterial thrombosis in the infrapopliteal territory as part of a cohort of 14 patients with thrombotic events. These events included acute coronary syndromes and cerebrovascular events related to their respiratory infection.7
Since the onset of the COVID-19 pandemic, cases of AAO due to acute thrombosis related to the infection have been reported,1,4 with an incidence of 2.7 to 5 cases per million persons per year.6
AAO is one of the most dramatic diagnoses in a vascular surgical practice. The acute interruption of blood flow to the infrarenal aorta leads to ischemia of the lower limbs, possible visceral ischemia, spinal cord ischemia, and renal failure if the occlusion propagates proximally.8 It carries a high morbidity and mortality rate, as well as a significant risk of limb loss, which can reach up to 30%.9 Contemporary case series report morbidity rates between 30% and 74%, an in-hospital mortality rate of 20% within 30 days, and an overall mortality rate of up to 60%.10 The most common presenting symptom is limb pain, followed by motor or sensory loss (18%-86%). Renal failure and/or visceral ischemia can occur in 12% to 24% of patients. Overall, the most common etiology tends to be thrombotic, occurring in 35% to 84% of patients, with embolic events being less frequent (8%-75%).11 Furthermore, the incidence of embolic events has shown a decreasing trend in recent years due to better control of embolic causes, such as AF, cardiomyopathies, and the use of safer and more effective anticoagulant therapies.9
In this scenario, the origin of the acute occlusion is unclear, as the patient has a predisposition to both embolic (recent AF diagnosis) and thrombotic etiologies (tumoral, COVID infection, and chronic LEIA occlusion).
Among the historically preferred surgical treatments for these patients are aortobifemoral bypass, extra-anatomic bypass (axillobifemoral), and bilateral thromboembolectomy, as well as pharmacomechanical thrombectomy and thrombolysis.12,13 The development and refinement of endovascular techniques provide us with new tools and therapeutic options, particularly for patients at high surgical risk. In some selected cases, these may represent the only therapeutic option. As a result of the above, the mortality rate has been reduced by 15.5% over the past 7 years.14 Despite this, and due to the limited case series reported in the literature, there is no consensus on the preferred surgical technique for this type of pathology, as it depends on various factors, including age, comorbidity, degree of urgency, and anatomical disposition.
Conclusions
In cases of AAO treated with bilateral embolectomy, where thrombectomy of one of the axes is not feasible and thrombotic debris persists in the infrarenal aorta, a hybrid approach with an aortic endograft and femorofemoral bypass represents a viable and safe option. This strategy is particularly applicable to patients at high surgical risk and/or those contraindicated or unable to undergo intubation, as demonstrated in this case. n
Affiliations & Disclosures
From the Department of Vascular Surgery, Alcorcón University Hospital, Madrid, Spain.
The authors report no financial relationships or conflicts of interest regarding the content herein.
Manuscript accepted September 9, 2025.
Address for correspondence: Miguel Ignacio Herrero, MD, Department of Vascular Surgery, Alcorcón University Hospital, C. Budapest, 1, 28922 Alcorcón, Madrid, Spain. Email: miguelignacio.herrero@salud.madrid.org
REFERENCES
1. Gomez-Arbelaez D, Ibarra-Sanchez G, Garcia-Gutierrez A, Comanges-Yeboles A, Ansuategui-Vicente M, Gonzalez-Fajardo JA. COVID-19-related aortic thrombosis: a report of four cases. Ann Vasc Surg. 2020;67:10-13. doi:10.1016/j.avsg.2020.05.031
2. Li YS, Li YC. Simultaneous acute limb ischemia related to acute Leriche syndrome and pulmonary embolism without existing patent foramen ovale: a case report. BMC Cardiovasc Disord. 2021;21:465. doi:10.1186/s12872-021-02272-3
3. Giacomelli E, Dorigo W, Fargion A, Calugi G, Cianchi G, Pratesi C. Acute thrombosis of an aortic prosthetic graft in a patient with severe COVID-19- related pneumonia. Ann Vasc Surg. 2020;66:8-10. doi:10.1016/j.avsg.2020.04.040
4. Woehl B, Lawson B, Jambert L, Tousch J, Ghassani A, Hamade A. 4 cases of aortic thrombosis in patients with COVID-19. JACC Case Rep. 2020;2(9):1397-1401. doi:10.1016/j.jaccas.2020.06.003
5. Yarımoglu R, Yarımoglu R, Tastan H, Erkengel HI. case report. Acute infrarenal abdominal aortic occlusion in a patient with COVID-19. Ann Saudi Med. 2021;41(6):392-395. doi:10.5144/0256-4947.2021.392
6. Barsanti-Innes B, Roche-Nagle G. Acute infrarenal aortic occlusion. BMJ Case Rep. 2020;13(3): e233238. doi:10.1136/bcr-2019-233238.
7. Cantador E, Núñez A, Sobrino P, et al. Incidence and consequences of systemic arterial thrombotic events in COVID-19 patients. J Thromb Thrombolysis. 2020;50(3):543-547. doi:10.1007/s11239-020-02176-7
8. Mosa E, Manouvelou S, Tolia M, et al. Acute Leriche syndrome in pancreatic adenocarcinoma: a case report. Curr Med Imaging. 2020;16(5):622-624. doi:10.2174/1573405615666190206161013
9. Hines GL, Liu HH. Acute aortic occlusion and its sequelae: metabolic, pathologic etiology, and management. Cardiol Rev. 2021;29(2):57-61. doi:10.1097/CRD.0000000000000313
10. Robinson WP, Patel RK, Columbo JA, et al. Contemporary management of acute aortic occlusion has evolved but outcomes have not significantly improved. Ann Vasc Surg. 2016;34:178-186. doi:10.1016/j.avsg.2015.12.021
11. Grip O, Wanhainen A, Björck M. Acute aortic occlusion. Circulation. 2019;139(2):292-294. doi:10.1161/CIRCULATIONAHA.118.036420
12. Crawford JD, Perrone KH, Wong VW, et al. A modern series of acute aortic occlusion. J Vasc Surg. 2013;59(4):1044-1050. doi:10.1016/j.jvs.2013.10.080
13. de Varona Frolov SR, Acosta Silva MP, Volo Pérez G, Fiuza Pérez MD. Outcomes after treatment of acute aortic occlusion. Cir Esp. 2015;93(9):573-579. doi:10.1016/j.ciresp.2013.07.002
14. Grip O, Wanhainen A, Björck M. Temporal trends and management of acute aortic occlusion: a 21 year experience. Eur J Vasc Endovasc Surg. 2019;58(5):690-696. doi:10.1016/j.ejvs.2019.05.018











