Inova Fairfax Medical Campus
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of EP Lab Digest or HMP Global, their employees, and affiliates.
EP LAB DIGEST. 2025;25(9):22-26.
Jordan Hamilton, BSN, RN, RCES; Cameron R Mulloy, RN, BSN, CCRN, RCES; and Monica Preiser, RN
EP Lab, Inova Schar Heart and Vascular, Falls Church, Virginia
When was the cardiac electrophysiology (EP) program started at your institution, and by whom?
EP procedures at Inova began circa 1988 by Albert Delnegro, MD.
What drove the need to implement an EP program? What is the size of your EP lab facility?
Inova Fairfax Medical Campus is the flagship Inova hospital, situated in the “heart” of northern Virginia, a busy metropolitan area just outside of Washington, DC.
The region has experienced tremendous growth over time, and with that, an increased need for more specialized medical services. It became clear that our population would benefit from the availability of EP services, so our cardiac catheterization laboratory branched off and formed an EP department.
Around 2014, our colleagues from interventional radiology (IR) joined us in what we now refer to as the “Invasive Corridor,” which consists of 5 EP labs, 7 cath labs, and 2 IR labs (the IR department operates 2 neuro IR labs, a pre/postprocedure area, and 2 computed tomography-guided procedure rooms elsewhere on the campus).
We are expanding to 6 dedicated EP labs later this year. We also perform high-risk extractions in a hybrid cardiovascular operating room (OR) when necessary.

Does your institution offer EP-related procedures in an ambulatory surgical center?
The EP labs at Inova Fairfax Medical Campus are hospital-based only. Inova offers EP services at 2 sister hospitals: Loudon and Alexandria, although these labs are combination EP/cath/IR, whereas Inova Fairfax Medical Campus has dedicated EP labs.
Who manages your EP lab, and what is the mix of credentials and experience?
Our lab is managed by Monica Preiser, BSN. Monica has been with Inova for 4 years and has over 15 years of EP experience. She has served in the EP lab at Inova in multiple capacities, including lab personnel, nurse navigator, supervisor, interim manager, and now manager. Stephen Ives is the director and is responsible for managing all team members across EP, cath, and IR. Our EP lab has 4 front-line supervisors: Nichole Robison, RCIS; Brad King, RCIS; Jordan Hamilton, BSN, RN, RCES; and Cameron Mulloy, RN, BSN, CCRN, RCES.
What is the number of staff members?
We have over 30 team members working in our EP labs, including supervisors and our manager providing support for 23 physicians from 3 different practice groups. The majority of our team is full time, and we have a few part-time and PRN team members. Two of our team members rotate to fulfill the role of EP nurse navigator, ensuring our patients are educated about their upcoming procedure and are scheduled appropriately. Some of our team members are cross trained to work at multiple Inova facilities in both cath and EP.

What types of procedures are performed?
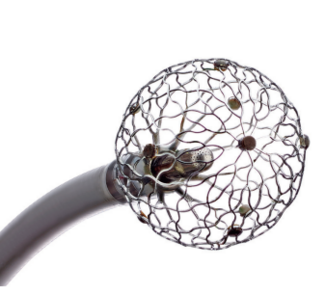
We perform nearly every EP-related procedure: device placements including leadless pacemakers, extravascular implantable cardioverter-defibrillators (EV-ICDs), subcutaneous ICDs (S-ICDs), conduction system pacing (CSP) (left bundle and Bachmann’s bundle pacing), a wide variety of ablations including ganglionic plexus ablations and pediatric/congenital EP cases, lead extractions, and a variety of pulsed field ablation (PFA) procedures. We are also home to one of the busiest pediatric/congenital EP programs in the country.
Our EP lab is proud to be one of the first 14 facilities to use the new dual-energy systems (Affera Mapping and Ablation System, Sphere-9 catheter, Medtronic). We are the first hospital to have 3 Affera systems operating simultaneously. We recently transitioned our left atrial appendage closure (LAAC) cases to the cath lab and have started doing concomitant Watchman (Boston Scientific)/atrial fibrillation (AF) ablation cases in the EP lab.
Approximately how many ablations (for all arrhythmias), device implants, lead extractions, and LAAC procedures are performed each week?
In 2024, we performed 2219 ablations, 1959 device cases (not including loop recorder implants), 56 lead extractions, and 144 Watchman procedures.
What types of EP equipment are commonly used in the lab?
We use the CardioLab EP Recording System (GE HealthCare) for monitoring and the EP-4 Computerized Stimulator (EP MedSystems). We have capabilities for the Carto (Johnson & Johnson MedTech), EnSite (Abbott), and Affera (Medtronic) mapping systems. We have participated in PFA trials with the Farapulse (Boston Scientific) and Volt (Abbott) systems. We routinely use the PulseSelect PFA ablation system (Medtronic), and also use the Affera system with the Sphere-9 catheter (Medtronic). Our ICE catheters are SoundStar (Johnson & Johnson MedTech), ACUSON AcuNav (Johnson & Johnson MedTech), and ViewFlex (Abbott), utilizing either Vivid (GE HealthCare) or Zonare (Abbott) ultrasound systems. We also have 3-dimensional ultrasound intracardiac echocardiography (ICE) capabilities with VeriSight (Philips) and NuVision (Johnson & Johnson MedTech) ICE catheters. We implant devices from Medtronic, Abbott, Boston Scientific, and Biotronik, as well as a variety of loop monitors.

What are some of the new technologies and techniques recently introduced in your lab? How have these changed the way procedures are performed?
Heraclitus did not know it at the time, but he described our EP department well when he said: “The only constant is change.” Particularly in the past year or so, we have experienced a whirlwind of technological advances, construction, and documentation changes. We have used PFA systems from nearly every major manufacturer. We have started implanting Medtronic EV-ICDs and left bundle/Bachmann’s bundle leads, and have also been fine-tuning our S-ICD implants. In Q2, we will have 2 new labs opening in our Invasive Corridor, which will lead to our EP department gaining one more lab space. In January of last year, we went live with our new Cupid build (Epic Systems), transitioning all documentation to a single source and virtually eliminating double documentation.
With a strong focus on education, we have held a physiologic pacing course in which visiting physicians come to Inova and learn techniques for effective and efficient placement of left bundle and Bachman’s bundle pacing leads. Likewise, we are a Medtronic Cardiac Ablation Solutions Experience Center for the Affera system, inviting visiting labs and operators to see our Affera workflow virtually or in person.
We have also noticed our patient population staying up to date with the latest advances. Our physicians are reporting patients specifically asking for PFA ablations and left bundle pacing leads, when applicable. The latest trends in cardiology at Inova were recently featured in several publications and social media platforms as well.
Our team is a monument to adaptability and resilience. The ever-increasing complexity and knowledge required to be proficient is incredible, and our team continually steps up to the plate to take on new challenges.
Discuss your technique for preventing esophageal injury during AF ablation.
Transitioning to PFA has added another layer of safety for preventing esophageal injury. When we perform an ablation using radiofrequency (RF) or cryo, we utilize a standard esophageal temperature probe for monitoring esophageal temperature, verifying placement with either fluoroscopy or ICE imaging.

Tell us more about your program’s use of PFA, including patient selection, challenges, and initial experience.
As with many other EP labs across the country, we have recently gained access to PFA technology through use of the Farapulse catheter, Volt system, PulseSelect PFA catheter, and Affera system. We currently have 3 Affera systems in operation. Our internal data has already shown improvements in outcomes using PFA over RF ablation, while also having the benefit of shorter case times on average. Our use of cryoablation for AF has been nearly eliminated in favor of PFA. Cryo therapy is now utilized almost exclusively through the use of focal cryo in pediatric EP cases.
Our teams were eager to jump into PFA, particularly because of its potential benefits over RF and cryo ablation technology. We started using multiple systems from different vendors around the same time, so it was a steep learning curve for us, and have since transitioned to routine use of PulseSelect and Affera.
How is inventory managed in your EP lab?
We use QSight (Owens & Minor) as our inventory management system. We scan any billable supplies we use during a case into QSight via an integration built into Epic. Our Invasive Corridor requires a team of 5 full-time inventory team members to keep up with our department’s needs.

Tell us what a typical day might be like in your EP lab.
We start with a department huddle at 7:05 AM each day. We then break up to our assignments and load our first patients by 8:00 AM. Our patient scheduling practices are designed to provide maximum flexibility. We utilize a flip lab model to help minimize downtime between cases and maximize productivity. This allows us to quickly adjust when cases run shorter or longer than expected, or if we have add-on inpatient emergencies. Since we do not know what the day will bring, we aim to be prepared for any case that might come next into our lab. We work collaboratively to care for patients, with each of us fulfilling our role to achieve that shared goal. There are 6 staff members on call each day: 4 on primary call and 2 on backup. This setup allows us to run 2 labs after-hours when necessary, though our preference is always to finish on time (5:30 PM). Our average call burden is 1 weekday call shift per week and 1 weekend every 2 months.
Can you describe the extent and use of vascular closure devices at your lab? Tell us about your approach for same-day discharge.
We have historically used a variety of hemostasis techniques including manual pressure, figure-of-8 sutures, and closure devices such as Perclose (Abbott), Angio-Seal (Terumo Interventional Systems), and Vascade (Haemonetics). We typically use Perclose for arterial and large-bore venous closure, Angio-Seal for arterial closure, and Vascade for pediatric cases. Our team is currently conducting a cost-benefit analysis on the use of closure devices in our cases. Most of our patients are discharged same day.
Has your lab recently undergone a national accrediting inspection?
Our EP lab is a recognized program through the Intersocietal Accreditation Commission. We are prepared for a Joint Commission visit, which is expected in the coming weeks.
Inova Fairfax Medical Campus routinely earns an “A” rating from The Leapfrog Group for safety, a 5-star rating from Centers for Medicare & Medicaid Services, and we have been designated the Health System of the Year by Press Ganey for 2025.
Inova is the largest hospital system to have all its hospitals (5 total) accredited by Magnet. Over the previous year, we have been preparing for Magnet recertification, and 2 of our nurses (Jordan Hamilton and Sue Pettit) represented our department in these preparations. We just finished showcasing our accomplishments and efforts to the Magnet appraisers and are looking forward to celebrating the redesignation.
How do you ensure timely case starts and patient turnover?
Our nurse navigators strategically schedule cases and set up our flip schedule to maximize efficiency, utilizing tools built into Epic to project case times. As one of our charge nurses put it when asked about his role: “I predict the future.” We rely on our leaders to anticipate both challenges and opportunities, adjusting the schedule and resources accordingly.
As part of our current “WIG” (Wildly Important Goal) project, we are analyzing data and identifying barriers to improving first case start times. We lean heavily on our room leads and supervisors to work together to overcome these barriers. Our standard turnover time between cases is 30 minutes or less. We have the capacity to easily document delay reasons in Epic. Our leadership and administrative teams compile that data, analyze it, and work to address any patterns that arise.
As part of a push to evaluate all aspects of our operation, we recently consulted with another high-efficiency, high-volume center to compare notes on resource management, room turnover, and efficiency tactics. We remain convinced our department is effectively managing all the many complexities of our operations. As we continue to evaluate our processes, we are working closely with our physician colleagues to capitalize on opportunities for improvement.
Do you have flexible or multiple shifts? How do you handle slow periods?
Our standard work week includes 4 ten-hour shifts. Most of us prefer to have one designated day off during the week, and our schedule can often accommodate those individual preferences. Slow periods are rare, though we take advantage of those times by flexing team members home early.
How are vendor visits managed?
After an extensive vetting process, our vendors check in at an electronic kiosk, where they get a temporary badge suitable for a single day visit. Our vendors utilize RepScrubs for their scrub needs.

What are the best features of your EP program’s layout or design?
With ever-increasing clinical expansion, storage space is at a premium in our Invasive Corridor. To alleviate some of the storage stresses, we use portable storage carts in the sterile core. We recently transitioned our storage model such that each cabinet is dedicated to a specific purpose or product type. For example, we have dedicated cabinets for ICE catheters, Affera cases, PulseSelect cases, decapolar catheters, leadless pacemaker implants, and device storage. This helps us quickly assess current inventory, identify supply needs, and improve efficiency in case preparation.
As part of a true medical campus with a dedicated heart hospital, the cath lab is located in the same corridor and shares pre- and postprocedural areas with IR. All cardiac units, along with cardiac diagnostics, are situated directly above our department.
What measures has your lab implemented to cut or contain costs?
We have an established recycling and reprocessing program for our catheters and sheaths, which helps us recover costs and pass the savings on to our patients.
What quality control measures are practiced in your lab?
We partner with infection prevention, environmental services, biomedical engineering, information technology, and other departments to maintain peak performance in all aspects of our operation. All team members are empowered to take an active role in maintaining operational excellence.
What works well in your lab for onboarding new team members?
This area has been a primary focus over the past year or so. One of our supervisors (Cameron Mulloy) spent time last year renovating our orientation program and developing an evidenced-based hybrid Tiered Skill Acquisition Model (TSAM) designed specifically for procedural areas. He and our manager, Monica, collaborated with our colleagues from professional practice to develop a model tailored to our department’s needs. While completely different than our previous orientation model, it has shown promise and good buy-in from the team. We are also thrilled to have one of our team members, Jordan Hamilton, step up to be our EP clinical educator. She will be responsible for further implementing and fine-tuning the hybrid TSAM orientation model, developing and training preceptors, coordinating incoming students from partner registered cardiovascular invasive specialist (RCIS) schools, and collaborating with industry and physicians to continue to meet the high level of competency that our patients deserve.
Inova has a partnership with Howard Community College (HCC) in which we accept students to participate in clinical rotations in cath and EP towards earning RCIS certification. This partnership is mutually beneficial, as many HCC students transition into full-time roles at Inova upon completing the program.
What continuing education opportunities are provided to staff? How do staff typically maintain and renew credentials?
We use a somewhat unique staffing model in the EP labs at Inova. Our team consists of roughly one-third registered nurses (RNs) and two-thirds RCIS non-RN personnel, and there is no distinction when it comes to performing the role. Each team member, regardless of which education track they have completed, is trained to circulate, monitor, and scrub. Because nearly all of our cases are supported by anesthesia personnel, our team is able to focus entirely on the procedural aspects of care.
We encourage registered cardiac EP specialist (RCES) certification in our department, offering incentives such as tuition/certification reimbursement and certification bonuses to facilitate that goal. For example, in 2021, we began partnering with Springboard Healthcare’s EP education program, developed in partnership with Duke Health. We also work closely with our onsite medical library in supporting study opportunities and learning resources. We reserve time on the second and fourth Wednesdays of each month for team member education, delivered by our own staff and leaders, industry representatives, or physicians. We were pleased to have the opportunity to send 3 team members to the Heart Rhythm Society’s annual scientific sessions this year.
Discuss the role of mid-level practitioners in your program.
Our advanced practice providers (APPs) support the physicians by rounding on their inpatients, identifying opportunities for procedures, and performing follow-up as indicated.
Does your lab use a third party for reprocessing or catheter recycling? How has it impacted your lab?
Yes, we partner with a third-party reprocessing and recycling company, which enables us to recover valuable materials and repurpose catheters—resulting in significant cost savings that can be passed on to patients.
Discuss your program’s approach to CSP.
We were early adopters of CSP, influenced in part by our section chief of cardiac EP, Brett Atwater, MD. Both Dr Atwater and Stephen Gaeta, MD, PhD, medical director of our EP lab, conduct in-person CSP courses at our facility. A large percentage of our transvenous device implants utilize left bundle CSP. As of February 2025, our facility ranked sixth nationally in the number of Medtronic left bundle pacing leads implanted, with nearly 600 model 3830 leads placed over the preceding 12 months.
Starting in the third quarter of 2024, our EP lab began implanting Bachmann’s bundle leads to synchronize the atria. We have also implanted a number of dual-chamber Aveir leadless pacemakers (Abbott).
Tell us about your primary approach for LAA occlusion.
We transitioned Watchman implants to the cath lab last year. However, we expect to start performing concomitant AF ablation and Watchman implant procedures in 2025.
Tell us about Inova’s AF Center of Excellence. Discuss goals, members of the comprehensive care team, and development of team-based care pathways.
Since Fall 2021, the Inova AF Center of Excellence has functioned as a comprehensive system designed to ensure that all patients with AF—from those newly diagnosed to those with longstanding persistent disease—receive personalized care for optimal disease management. This includes a multidisciplinary team with EP, cardiology, sleep medicine, neurology, and medical weight loss services, extending through APPs, pharmacists, and clinic staff to address all risk factor modifications (including hypertension, sleep apnea, obesity, and alcohol use, etc). From the moment a patient enters the system—whether through a primary care visit or the emergency department—the goal of the AF Center pathway is to proceed efficiently, minimizing the time from diagnosis to intervention. A current initiative involves the development of an advanced AF Registry to support this aim by enhancing coordination across the expansive Inova system, from EP laboratories to outpatient clinics.
Discuss your approach to lead extraction and management.
We have a fairly substantial lead extraction program. In 2024, we performed 56 lead extraction cases in collaboration with our colleagues from the cardiac operating room, utilizing their hybrid OR. In 2025, the physician groups with whom we partner added 2 electrophysiologists credentialed in lead extraction.
How does your EP lab handle radiation protection for physicians and staff?
Many of our physicians perform ablation procedures using zero fluoroscopy, relying on ICE for transseptal access and to confirm esophageal temperature probe placement.
For the cases using x-ray, we use a variety of physical shielding methods. Each team member is fitted for their own lead after their orientation is completed. Our department also utilizes a wide selection of nonassigned lead aprons that can be used by anesthesia personnel, guests, or trainees. Each of our Philips procedure tables has a lead shield on both sides of the table. We also have a ceiling-mounted radiation shield that is used for groin access procedures.
What approaches has your lab taken to reduce fluoroscopy time? How are fluoroscopy times/dosages recorded?
Radiation doses, including milligray exposure and fluoroscopy time, are tracked for each case and compiled into annual reports stratified by physician. Team member exposures are monitored on a monthly and annual basis from data gathered by individually assigned dosimeters.
What clinical research is your EP lab currently involved in?
In 2024, we were involved with multiple trials and studies, including Volt, RESTART, REINVENT-CRT, Left vs Left, OMNYPULSE, and RESOLVE-AF. We anticipate starting ELEVATE AF, Sphere-360, and LBBx soon.
What is considered historic about your EP program or hospital? Has your program or hospital recently experienced any “firsts”?
We were selected as one of the first sites to launch the Affera mapping and ablation system and Sphere-9 catheter. Inova Fairfax Medical Campus is the first site to utilize 3 Affera systems and we just completed our 500th Affera case. Zack Hollis, MD, was the first in the country to successfully implant a leadless Bachmann’s bundle pacemaker using the Aveir device. We also are starting our first EP physician fellowship program in July 2025.
Describe your city or general regional area. How is it unique?
Inova Fairfax Medical Campus sits in the “heart” of Northern Virginia, which is home to over 3.25 million people. Located in a vibrant suburban–metropolitan area just outside Washington, DC, Inova draws patients from well beyond the immediate region.
What specific challenges does your hospital face given its unique geographic service area?
Inova has a large percentage of the health care market share in the immediate northern Virgina region, though it is geographically surrounded by a variety of competitors. Inova is growing strategically and finding ways to attract patients from further away and offer services outside of our traditional market area.
A substantial portion of the economy in northern Virginia is driven by military, government, and government contractor organizations. Because of this, the area tends to be populated by a higher-than-average amount of well-compensated though somewhat transient residents. A relatively smaller percentage of people are born here and remain here their whole lives. Because of this, health care worker turnover tends to be higher in the greater metropolitan DC region, though Inova overall maintains a nursing turnover rate lower than the national average—a tribute to this being a great place to work.
Please tell our readers what you consider special about your EP lab and staff.
We are fortunate at Inova Fairfax to have a dedicated and collaborative team of physicians, leaders, and staff. The EP lab has a long and distinguished history, with many team members and physicians who have been part of the program for decades. Our operations are recognized for delivering high-quality, comprehensive, and diverse care. Our team takes pride in achieving competency and accuracy in their practice, often independently seeking out specialized education to enhance their skills.
In addition to our professional achievements, we take pride in fostering a strong sense of community within the department. Whether participating in a local kickball league (where our skills are better suited to EP than athletics!) or enjoying events organized by our Sunshine Committee—such as March Madness brackets, holiday parties, and potlucks—we value the camaraderie that strengthens our team. At Inova Fairfax, we believe that our culture of clinical excellence, mutual respect, and community is what truly sets us apart.
For more information, please visit:
https://www.inova.org
https://www.facebook.com/InovaHealth/
http://www.linkedin.com/company/inovahealth
https://www.inova.org/careers
For more on Inova Fairfax Medical Campus, be sure to check out their podcast episode from The EP Edit!