Baylor Scott & White The Heart Hospital Denton
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of EP Lab Digest or HMP Global, their employees, and affiliates.
EP LAB DIGEST. 2025;25(6):1,16-20.
Matthew Evans, MD
Denton, Texas
What is the size of your cardiac electrophysiology (EP) facility? Has the EP program recently expanded in size, or will it soon?
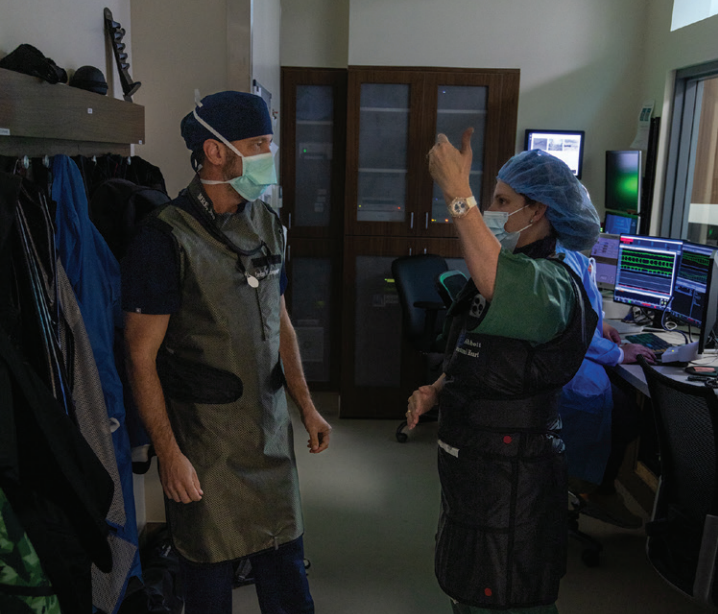
We currently possess 2 dedicated EP and 2 cardiac catheterization laboratories (one of which has EP capabilities as well), in addition to 2 cardiovascular operating rooms. The new EP laboratory became available earlier last year, and there are plans for buildout of additional catheterization laboratories. There are plans for expansion of all service lines in different stages of development. The hospital has a current capacity of 22 inpatient beds with plans to expand. Our EP lab is accredited by the American College of Cardiology.

Who manages your EP laboratory, and what is the mix of credentials and experience?
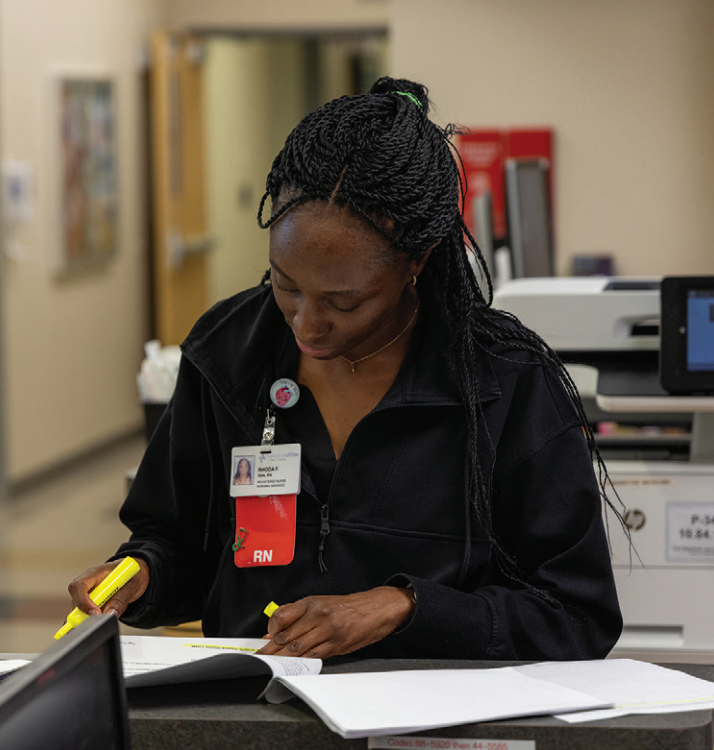
I serve as medical director, and Scotty Ross, RN, manages our laboratories in Denton, having been in the laboratory as a nurse from the beginning. His leadership has been instrumental in the expansion that we have seen in the program over the last several years. We have 6 techs and 11 nurses with over half a century of cumulative experience in the EP lab.
How do you ensure timely case starts and patient turnover?
Through Epic integration, we monitor first case on-time starts, all cases on-time starts, and same-room turnover. This gives us a percentage view of laboratory efficiency on a monthly and weekly basis. We also look at case length accuracy for 3 categories: overscheduled, accurate, and under-scheduled. This is discussed with staff at staff meetings.

How does your laboratory schedule team members for call?
We schedule staff as a ST elevation myocardial infarction (STEMI) call team, as our laboratory staff is cross trained in EP, structural, and interventional cardiology. We have a schedule that is repeatable to allow staff to be able to plan accordingly. We also allow staff to request “no call” when they have plans involving time when they could be placed on call.
Do you have flexible or multiple shifts?
We offer 2 shifts, with the majority of staff working four 10-hour shifts per week, and some working five 8-hour shifts. We have developed a shift rotation that allows the staff working 10-hour shifts to have a 4-day weekend every fourth week.

How do you handle slow periods?
The need to flex staff off is very little, typically limited to when we have multiple physicians on vacation. We also allow the 10-hour staff to shift their day off during the week to higher volume days; this greatly reduces the need to flex staff on lower volume days. We also utilize slow times for education, cleaning/organizing, or working in the catheterization laboratory.
How are vendor visits managed?
Vendors are managed by Green Security. Each vendor must remain current with all documentation and vaccines. The vendor must place a visit request into Green Security for the area they want to visit, which is then approved by leadership.
How is inventory managed in your EP lab?
Currently, we use the iRIS inventory management system (Mobile Aspects, Inc), which allows us to inventory, order, and charge out to patients. This software, bolstered by radiofrequency identification and artificial intelligence technologies, automates inventory control and is integrated in the electronic heath record for supply capture during procedures.

What types of procedures are performed at your facility?
• Ablation of atrial fibrillation (AF) (using pulsed field ablation [PFA], cryo, and radiofrequency [RF] options), supraventricular tachycardia (SVT) ablation, ventricular tachycardia (VT/PVC) ablation
• Left atrial appendage occlusion (LAAO) (Amplatzer Amulet left atrial appendage occluder, Abbott)
• Device implantation, including conventional cardiac implantable electronic devices (CIEDs), dual- and single-chamber leadless (Micra, Medtronic, and AVEIR DR and AVEIR VR, Abbott), and conduction system pacing (CSP)
• Cardiac Contractility Modulation (CCM; Impulse Dynamics) devices for select heart failure patients
What types of EP equipment are commonly used in the lab?
• OPAL HDx Mapping System (Boston Scientific), Carto (Johnson & Johnson MedTech), EnSite X (Abbott)
• Farapulse PFA System (Boston Scientific)
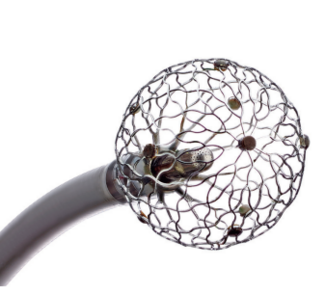
• Arctic Front Cryoballoon (Medtronic)
• Standard and 4-dimensional (4D) intracardiac echocardiography (ICE)
What are some of the new technologies and techniques recently introduced in your lab?
PFA is the most recent addition; in particular, its integration with the OPAL mapping system has significantly improved fluoroless workflow. Dual-chamber leadless pacing (AVEIR DR) is another recent addition that is being performed more frequently; it is a particularly attractive option in younger patients due to their increased relative lead dwell time due to the potential to remove AVEIR devices as part of their design. We recently implanted the first dual-chamber leadless device within the Baylor Scott & White system (and North Texas). We also recently implanted the first CCM device, a promising therapeutic option for select patients with advanced heart failure, in Denton County, Texas. We are constantly striving to improve the safety, efficacy, and efficiency of these procedures, in that order. There is a strong interest in minimizing or eliminating fluoroscopy where possible. This is not only in the interest of patient safety, but also the safety and comfort of the staff. With the exception of AV node ablation, all ablations that I perform, including PFA, are now completely fluoroless.

Tell us more about your program’s use of PFA.
As a more recent addition to our repertoire, PFA has substantially changed and improved AF management. The improved safety profile over traditional thermal ablation options is probably the most important aspect of this procedure, particularly when it comes to potential complications such as esophageal or phrenic nerve injury. We believe the selection of appropriate candidates has expanded as a result of the improved safety profile of PFA together with the recent guidelines for the management of patients with AF. While I have begun using the OPAL mapping system for many of these cases, our operators routinely use all our mapping systems to aid in this procedure.

My personal workflow for a PFA case includes administration of glycopyrrolate (or atropine) in addition to heparin prior to femoral venous access. Three access sites are obtained in the right femoral vein under ultrasound-guided access. Then, 11 French (F), 8F, and 7F short sheaths are inserted. The ICE catheter is inserted in the 11F sheath and placed in the right ventricle (RV) for initial assessment of pericardial effusion, followed by advancement to the superior vena cava (SVC). The transseptal wire is then inserted into the 8F sheath and advanced to the SVC. A VersaCross pigtail system (Boston Scientific) is typically used for transseptal access. This wire is highly visible by ICE and allows clear placement in the left superior pulmonary vein (LSPV) upon entering the left atrium (LA). Given the large size and stillness of the Faradrive Steerable Sheath (Boston Scientific), the Faradrive sheath is then inserted over the wire and advanced to the SVC. The VersaCross wire is pulled into the sheath, slight deflection is added to the sheath, and ICE is withdrawn to the fossa. Much like the cryoballoon strategy, transseptal access is aimed more inferior and anterior relative to that used with access for RF-based pulmonary vein isolation (PVI). This allows more room for manipulation of the system to the right-sided PVs. Once access is achieved, the wire and dilator are removed and the Farawave catheter (Boston Scientific) is advanced to the tip of the sheath after the system is extensively aspirated and flushed. The catheter is advanced to the tip of the sheath, with a Rosen Wire (Cook Medical) leading the tip of the catheter by 3-4 cm. The tip of the wire is placed in the LSPV as the splines are exposed in the LA under ICE guidance. From there, the sheath is often backed into the RA to allow the ICE catheter to follow the Farawave catheter into the LA; however, when there is clear delineation of structures from the RA, the ICE catheter is right sided. Once in the LA, posterior tilt is applied to the ICE catheter, and the sheath is re-advanced back across the septum while pinning the catheter, all under direct ICE guidance. From there, the LSPV and left inferior pulmonary vein (LIPV) can be easily identified and cannulated by the wire and Farawave catheter. Two pulses each in 2 separate offset basket configurations are performed, followed by 2 pulses each in 2 flower configurations, for a baseline of 8 treatments per PV. All splines of the catheter are separate colors on our system, in this case, typically guided by EnSite mapping. After ablation is performed, the device is placed in a narrow basket configuration and placed in the treated PV. Pacing of at least 2 splines is then performed to document exit block. Typically, the 2 splines with the largest signal are used for pacing. It is rare for exit to be demonstrated; however, when present, additional basket and/or flower configuration lesions are placed. For the right-sided veins, the catheter is backed into the sheath, which is deflected, and 1-2 cm of wire is exposed. The ICE beam and sheath/catheter are moved clockwise in concert. The right inferior pulmonary vein (RIPV) is typically the first vessel to appear. Great caution is employed to ensure that the wire is always leading, and advancement is minimized in this configuration to avoid perforation. One of the elegant features of ICE guidance is direct visualization of the wire and catheter as they are being advanced to their target positions. Not only does this help prevent perforation, but it allows direct visualization of catheter configuration and contact within the PV. Once all veins are treated and exit block is achieved, a comprehensive EP study is performed. If typical flutter is induced, this arrhythmia is also targeted. Throughout the procedure, intravenous fluids are continuously administered if the patient has normal left ventricular systolic function. We have yet to encounter evidence of hemolysis or renal dysfunction associated with PFA. Typically, vascular closure devices (Vascade, Haemonetics, and Perclose, Abbott) are also employed to minimize risk of post-procedural bleeding as well as allow for earlier ambulation and same-day discharge (SDD).
Discuss your techniques for preventing esophageal injury during AF ablation.
When using thermal ablation, which is less common after the institution of PFA, an esophageal temperature probe is employed in my cases, tethered tip-to-tip with a quadripolar EP catheter visible on 3-dimensional mapping to allow for frequent repositioning. This probe is also simultaneously visible on ICE imaging, which is used during initial placement and as needed for repositioning. An important aspect of any successful laboratory is developing a positive work environment as well as culture of learning and engagement of all staff members. Not only does this foster a more enjoyable day, but it adds layers of safety as staff that is engaged is watching more closely, particularly at points in a case where the potential risk of complication is higher. An example of this includes knowing where the catheter is during ablation. Staff is aware when on the PW and there are multiple staff members, in addition to the operator, watching for temperature rise. We usually have at least one staff member call out when the temperature rises by 0.1-0.2 ºC. We halt energy and/or move to an anterior location when the temperature increase exceeds 0.5 ºC from baseline. This information is displayed continuously on multiple monitors in the laboratory, anesthesia monitors, and in the control room. We also routinely prescribe a minimum of 30 days of proton pump inhibitor therapy post-thermal ablations (both RF and cryo, since the risk exists with all thermal forms of ablation).
Discuss your use of hybrid AF ablation.
We offer hybrid surgical ablation via the Convergent approach. We work closely with our heart surgeons in patient selection, which also often includes LAA closure with LAA clipping via a minimally invasive video thoracoscopic approach.
Tell us about your device clinic and approach to remote monitoring of arrhythmias.
Our device clinic utilizes device reps for in-office checks and a team of registered nurses for remote monitoring. They log in daily and review the site-deemed red alerts, followed by yellow and scheduled/no alert remotes. They work on dual screens and often open the patients’ charts to review the most recent office visit notes while reviewing the remote transmission to give a better understanding of the patient, including medication status and arrhythmia histories, along with symptoms associated with any of their historically relevant arrhythmias. They write key pieces of information in the notes section for each patient. For more critical or new findings, the patient is called by the nurse, who provides a direct office number for any future questions or concerns. This personal, concierge-level treatment has been well received by our patients. The nurses have worked with our electrophysiologists to learn individual nuances and preferences. They work hard to be the first-line filter for the electrophysiologists so they can have more time for each patient and also earn their trust in judgement.
Tell us what a typical day is like in your EP lab.
We typically start cases at 0700 and wrap up around 1600 each day. When possible, we also alternate lab cases between general anesthesia and devices under moderate sedation directed by the electrophysiologist. All our lab staff is cross trained in structural and interventional cardiology as well as EP, which allows us to seamlessly move back and forth from the catheterization and EP laboratory. Further, we often benefit from excess anesthesia availability (eg, gaps between heart surgery cases) wherein we can also perform transesophageal echocardiography (TEE) and/or cardioversion in the noninvasive spaces while turning over the primary EP laboratory. Safety and efficiency are always in focus and evaluated (usually informally) on at least a weekly basis.

Tell us more about your approach for SDD.
We have employed SDD with most elective EP procedures since 2018. This began through use of a retention stitch and stopcock technique at the groin access site. We have more frequently moved to using the Vascade MVP closure device (Haemonetics) for larger French sizes, which has provided a trend toward less bleeding while simultaneously allowing earlier ambulation and discharge. The Vascade protocol allows the patient to sit up earlier, which helps to mitigate much of the discomfort often associated with stick post-procedural bed rest. It also allows us to free up outpatient staff earlier in the day.
What are the best features of your EP laboratory’s layout or design?
The close proximity of the laboratory with the day surgery and post-anesthesia care unit is ideal. It allows for more efficient patient transport and closer communication with staff between these areas. Additionally, our EP laboratories are quite large and mapping systems are mounted on booms, which allows them to be easily tucked out of the way when not in use. In our new EP laboratory, the C-arm is ceiling mounted, allowing it to be completely moved out of the way when not in use.
Discuss your program’s approach to CSP.
I tend to consider CSP mostly in patients whom we predict a greater than 25% ventricular pacing burden with normal baseline left ventricular systolic dysfunction. However, as CSP continues to evolve and improve, we have been using it more and more. This will become a particularly compelling option once a leadless CSP option becomes available. On average, CSP is being performed at an increasing frequency, and as such, procedural complexity and duration has begun to approximate implantation of a standard RV pacing lead.
Tell us about your primary approach for LAAO.
In all patients undergoing LAAO, the patient’s AF rhythm management strategy is reviewed, and if appropriate, PVI is discussed with the patient. If the patient wishes to undergo this procedure, ablation typically occurs first, followed by a staged LAAO. In patients at risk for falls or a known history of falls, we often ask our physician liaison to communicate with their primary care physician to discuss potential physical therapy options to help reduce the risk of future falls and injury. Additional historical risk factors are also considered, such as generalized weakness, slow walking speed, low physical activity, self-reported exhaustion, and unintentional weight loss. Patients are imaged within 48 hours prior to the procedure. Most are done by computed tomography (CT); however, for those with renal dysfunction, TEE is sometimes performed to clear and assess the appendage before the case is started. Most cases are performed by TEE guidance; however, in patients with contraindications or difficulties with TEE or general anesthesia, we can guide the case by 4D ICE under moderate sedation. This is decided on a case-by-case basis. CT-based LAA measurements (if available), TEE measurements, and LAA angiography are used for initial sizing of the device. At the conclusion of the procedure, the venotomy site is typically closed, which has allowed earlier ambulation and SDD. A limited echocardiogram is performed prior to discharge to rule out the development of pericardial effusion. All patients are re-imaged (ideally by TEE) to assess residual leak, device positioning, and any evidence of associated thrombus. Dual antiplatelet therapy is initiated the day of implant and continued for 6 months. Assuming the follow-up imaging is acceptable, the P2Y12 is dropped and aspirin (81 mg) is continued indefinitely.
Does your program have a dedicated AF clinic? Discuss goals, members of the comprehensive care team, development of team-based care pathways, and approach to lifestyle risk factor modification (RFM) for reduction of AF.
The data is clear that lifestyle and RFM is an important aspect of any rhythm control strategy. At Baylor Scott & White The Heart Hospital Denton*, we are excited to be rolling out a dedicated clinic for the comprehensive management of AF. This is largely an advanced practice provider (APP)-directed clinic with involvement by nurse educators, nutrition, and exercise physiology, with referrals to primary care, sleep medicine, and general cardiology as indicated. It is located on the campus of The Heart Hospital Baylor Denton. We are developing specific diets (plant-based and Mediterranean variants) designed for this population with further direction on meal prep available. Also, we are developing an exercise and training program with our cardiac rehabilitation facility, which is adjacent to the clinic. The referral base for this primarily includes urgent care and primary care (ideally at the time of initial diagnosis), with the goal to capture AF early in the course of the disease. The primary focus is rhythm management, but initial consultation also addresses risk factor reduction with specific counseling on alcohol cessation, activity (and exercise counseling), weight loss (with potential dietary counseling), and management of comorbidities such as hypertension and diabetes. Clinical data will be recorded prospectively as well. We are optimistic this will show improved patient satisfaction, improved outcomes, and long-term rhythm control post intervention. Any electrophysiologist credentialed at our facility may take part in this clinic. For each day that the clinic is operational, an electrophysiologist is identified who will be available if the APP or other staff have questions or need guidance. Ideally, the physician will also meet with the patient (between cases on procedure days) to establish rapport and answer questions. Follow-up visits will then occur at that physician’s clinic. We are optimistic that this will quickly become a model for other such clinics throughout the system.
Has your program or hospital recently experienced any “firsts”?
We are excited about the opening of our AF clinic, which will be transformative in the management of recently-diagnosed AF in our community. This will not only improve overall access to care, but its strong focus on lifestyle and dietary counseling, RFM, and prompt rhythm management if desired will set it apart from many other clinic models. This will be first of its kind for our system and North Texas. We are also instituting a remote rhythm monitoring solution for our emergency department, which will allow patients to leave the department with a 2-week monitor and close outpatient follow-up. We are the first in Denton County to offer PFA, LAAO, CCM implantation, and transcatheter aortic valve replacement (including being one of the smallest hospitals in the nation to offer this).
What dominant trends do you see emerging in the practice of EP?
There is definitely a continued push in the AF realm to manage the entire disease process as soon as possible after the diagnosis of the condition is made. Through the development of our comprehensive AF clinic, our aim is to approach AF on a holistic level from the start. An exciting advancement in device therapy will likely be CSP via leadless devices. We are hopeful that this will allow for clinical results on par or better than the current standard of biventricular pacing, without the dependence on acceptable coronary venous anatomy and myocardial suitability for optimal intrinsic conduction system activation.
*Joint ownership with physicians