Expanding Access to Cardiac Care: Electrophysiology in the Ambulatory Surgery Center Setting
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of EP Lab Digest or HMP Global, their employees, and affiliates.
EP LAB DIGEST. 2026;26(2):26-27.
Becky Joseph, BSN, RN
Director, Cath Lab and Ambulatory Surgery Center Alaska Heart & Vascular Institute, Anchorage, Alaska
The Alaska Heart & Vascular Institute (AHVI) has operated as an ambulatory surgery center (ASC) since 2013. The center is currently approved to perform procedures for Medicare and Medicaid beneficiaries one day per week. On other days, the same facility functions as an office-based laboratory (OBL), utilizing state-of-the-art technology used for electrophysiologic (EP) procedures in hospitals. Because the lab is located on hospital grounds, rapid access to emergency department, intensive care unit (ICU), and operating room (OR) services is available through established transfer protocols. At AHVI, the top priority is preserving high standards of procedural safety, optimizing the efficiency of elective cardiac care, and consistently achieving high levels of patient satisfaction. The care team includes a director, supervisor, 5 registered nurses, and 5 registered technologists (cardiovascular or radiologic). The facility currently consists of 1 OR and 7 preoperative and recovery bays.
AHVI’s ASC currently offers a wide range of cardiac procedures, including cardiac resynchronization therapy defibrillator (CRT-D) and implantable cardioverter-defibrillator (ICD)
implantations (single-, dual-, and multi-lead), generator changes, system upgrades, electrode removals, and pocket revisions. Additional procedures include cardiac resynchronization therapy pacemaker (CRT-P) and pacemaker implants, upgrades, and generator changes for both atrial and ventricular configurations. The ASC also performs loop recorder implantations and explants, lead revisions, and transesophageal echocardiography (TEE). EP studies, cardioversions, and cardiac ablations are performed for atrial fibrillation (AF), atrial flutter (AFL), supraventricular tachycardia (SVT), and premature ventricular contractions (PVCs). AHVI utilizes 3 advanced cardiac mapping systems for ablation procedures: the EnSite mapping system (Abbott), the CARTO mapping system (Johnson & Johnson MedTech), and the Affera mapping system with Sphere-9 catheter (Medtronic).
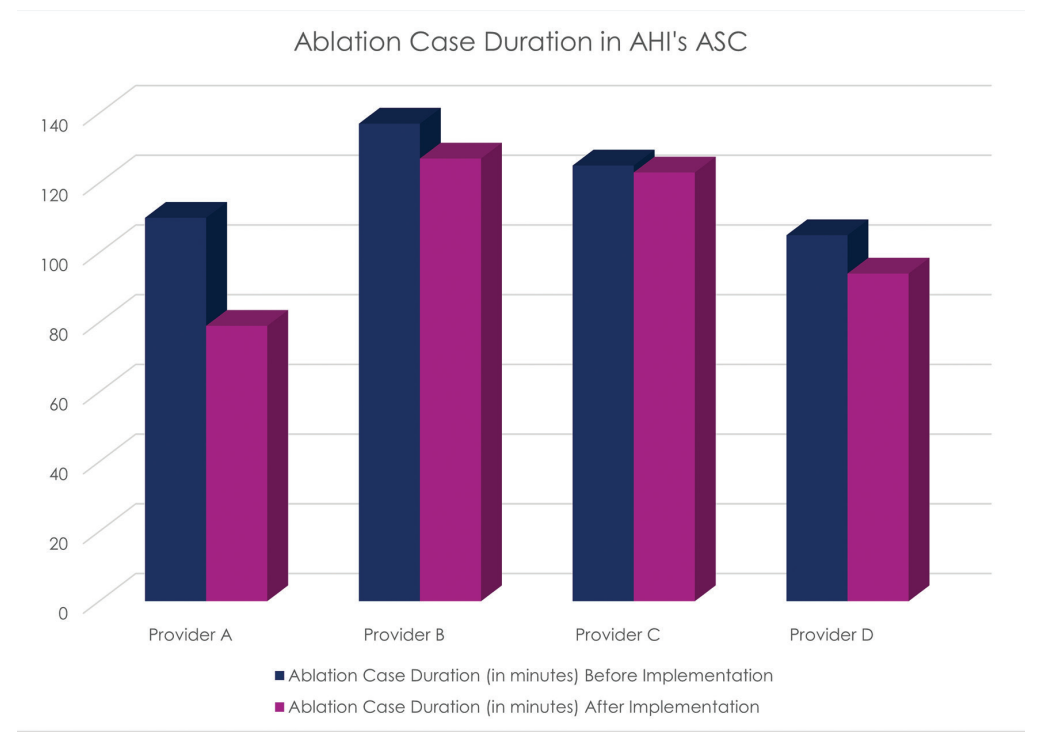
The newest technology at AHVI includes the Affera Mapping System, which utilizes the Sphere-9 mapping and ablation catheter to provide dual-energy ablation capabilities using both radiofrequency (RF) and pulsed field ablation (PFA) energies. This all-in-one system enables mapping, ablation, and validation through a single transeptal, zero-exchange workflow. The Sphere-9 catheter features a compressible lattice tip with a wide-area focal design and close-unipolar mapping capacity for procedural safety, efficacy, and efficiency. AHVI is the first ambulatory outpatient facility in the world to implement this technology. Since incorporating the Affera Mapping System and Sphere-9 catheter, the center has achieved an average 18% reduction in case duration.
AHVI maintains an excellent patient safety record and has been a national leader in this area. Two of AHVI’s electrophysiologists, Mark Willcox, MD, and Steve Compton, MD,
along with other experts in the field, contributed to both a single-center study and a multicenter trial demonstrating the safety and feasibility of performing cardiac EP procedures in ASCs. In a retrospective study published by Aryana et al in 2024,1 currently approved cardiac EP procedures performed in hospital outpatient departments (HODs) were associated with a 36% higher cost compared with ASCs ($11,093 ± 9,532 vs $8,172 ± 8,463; P=.03). The study also showed a low complication rate associated with various EP procedures conducted in ASCs. These findings informed the American College of Cardiology’s advocacy for the safe performance of EP procedures in ambulatory settings, where costs are substantially lower than in hospital-based care.
The COVID-19 pandemic forced health care providers to adapt and innovate in response to the substantial strain on hospital systems. One key development was the Centers for Medicare & Medicaid Services (CMS) Hospitals Without Walls program, which enabled the expansion of several EP procedures into the ASC setting.
The use of ASCs, rather than traditional HODs, offers several advantages. ASCs are associated with lower procedural costs and help reduce the operational burden on hospital systems. In Alaska, where patients often face unique barriers to accessing care, this model enhances access, improves clinical outcomes, and lowers both overall health care costs and out-of-pocket expenses for patients. Following the recent update to reimbursement rates by CMS in November, AHVI anticipates continued growth and expansion of services.
In November 2025, CMS approved an expanded list of EP procedures for Medicare and Medicaid beneficiaries in ASCs. In response, AHVI plans to increase the number of ASC operating days. This expansion is intended to reduce health care costs and improve access to high-quality care in a setting demonstrated to be both safe and efficient. AHVI remains committed to delivering exceptional care while continuing efforts to lower health care costs for Alaskans.











