Arrhythmias Don’t Wait: How Penn Presbyterian Elevated Cardiac Care With RhythmStar® Monitoring
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of EP Lab Digest or HMP Global, their employees, and affiliates.
EP LAB DIGEST. 2025;25(9):14-16.
Benjamin D’Souza, MD; and Alanna Miller, DNP, CRNP
Summary
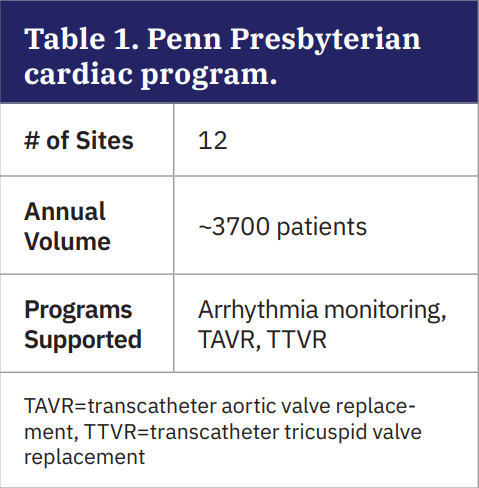
At Penn Presbyterian Medical Center and 12 affiliated sites within the University of Pennsylvania Health System (Table 1), Dr Benjamin D’Souza and the electrophysiology (EP) team sought to address the limitations of a fragmented remote monitoring system. Challenges with inconsistent data quality, delayed transmissions, and variable service and device performance across vendors prompted a system-wide evaluation. RhythmStar® (RhythMedix) was selected based on its diagnostic reliability, continuous data transmission via built-in cellular connectivity, and ability to support both routine and complex patient populations.
 A key factor in the decision was RhythmStar’s triple-review workflow, which combines Augmented Arrhythmia Intelligence™ (AAI) with continuous, daily, and final electrocardiogram (ECG) analysis. This approach integrates algorithmic prescreening with expert review by credentialed professionals certified by Cardiovascular Credentialing International (CCI), including Certified Cardiac Technicians (CCTs) and Certified Rhythm Analysis Technicians (CRATs). The result was more consistent reporting, quicker clinical decision-making, and the ability to support newer care models, such as postprocedural monitoring following transcatheter aortic valve replacement (TAVR) and transcatheter tricuspid valve replacement (TTVR), within existing workflows.
A key factor in the decision was RhythmStar’s triple-review workflow, which combines Augmented Arrhythmia Intelligence™ (AAI) with continuous, daily, and final electrocardiogram (ECG) analysis. This approach integrates algorithmic prescreening with expert review by credentialed professionals certified by Cardiovascular Credentialing International (CCI), including Certified Cardiac Technicians (CCTs) and Certified Rhythm Analysis Technicians (CRATs). The result was more consistent reporting, quicker clinical decision-making, and the ability to support newer care models, such as postprocedural monitoring following transcatheter aortic valve replacement (TAVR) and transcatheter tricuspid valve replacement (TTVR), within existing workflows.
Background: A Fragmented Monitoring Infrastructure
Remote cardiac monitoring has become a cornerstone in the evolving landscape of EP, enabling clinicians to detect, manage, and intervene on arrhythmias with greater precision and efficiency. At Penn Presbyterian Medical Center, part of the University of Pennsylvania Health System, the EP team, led by Dr D’Souza, recognized the limitations of its fragmented monitoring infrastructure. With multiple vendors supplying devices of varying quality and service levels, the department faced significant clinical and operational inefficiencies.
The decision to transition the multisite cardiology network to RhythmStar was driven by a commitment to improving patient care, optimizing provider workflows, and standardizing monitoring practices. What followed was a comprehensive transformation, marked by enhanced diagnostic accuracy, improved patient satisfaction, and accelerated care delivery in both routine and high-acuity settings.
Before adopting RhythmStar, the EP program at Penn Presbyterian relied on several of the major ambulatory ECG (AECG) vendors in the market. Each of these larger vendor solutions brought its own strengths but also significant drawbacks. Patients frequently reported issues such as delayed shipments, complex setup instructions, uncomfortable devices, and inconsistent battery performance. From a provider standpoint, the lack of data uniformity and reporting standardization created extra work for already overburdened staff. Reports often required reformatting or reinterpretation, and delays in data transmission reduced the window for timely intervention.
Customer service also varied widely, and EP staff spent significant time troubleshooting device issues or responding to patient concerns. There was no single vendor accountable for performance across the system, and this fragmentation ultimately eroded confidence in remote monitoring as a reliable extension of the EP lab.
Choosing RhythmStar: A Data-Driven Decision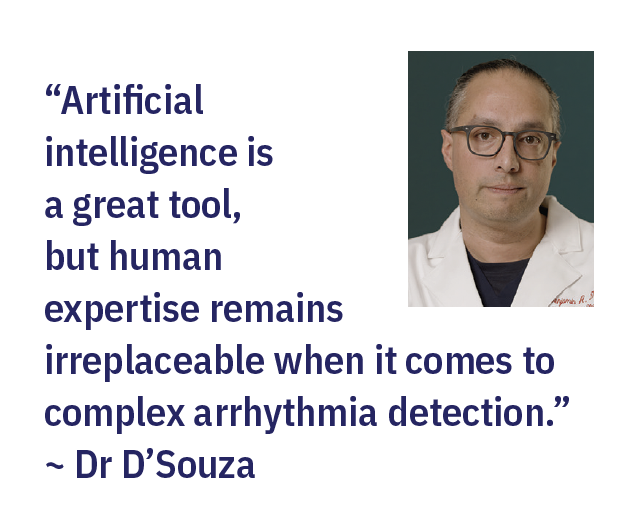
After a series of AECG vendor evaluations and numerous pilot trials, Penn Presbyterian selected RhythmStar first as a complement to other vendors and then ultimately as its exclusive ambulatory monitoring solution. Several key attributes drove this decision:
• High-fidelity ECG signal quality with minimal artifacts, enabling superior diagnostic confidence
• Triple-review workflow combining AAI with continuous, daily, and final ECG analysis—pairing advanced algorithms with expert review by CCI-certified CCTs and CRATs
• Continuous cellular transmission, eliminating delays associated with Bluetooth or mail-back models
• Seamless, customizable reporting formats aligned with Penn’s clinical decision-making processes
• Responsive, US-based 24/7 customer service
• Streamlined ordering and device delivery process, ensuring timely access to monitoring for patients across 12 outpatient sites
It was the triple-review and 24/7 staffed customer service that became the tipping point for Penn Presbyterian. They could not rely on algorithms only to process this information.
The impact of the transition to RhythmStar has been broad and measurable. From a clinical perspective, Penn Presbyterian has observed improved signal fidelity that reduces false-positives and enhances atrial fibrillation (AF) burden assessments. This has translated into faster, more confident interventions, particularly in high-risk populations such as TAVR patients.
“I do not want to find out about post-TAVR heart block or untreated AF weeks later. I want near real-time alerts,” stated Dr D’Souza. RhythmStar’s continuous data transmission provides just that.
Operationally, the integration of RhythmStar into Penn Presbyterian’s TAVR workflow has enabled discharges to occur later in the day and even on weekends, supported by preauthorized monitor orders and at-the-bedside education. Nursing staff hand patients a device with simple instructions, and data collection begins immediately, no technician involvement or post-discharge setup required.
Alanna Miller, DNP, CRNP, leads the team of 11 EP advanced practice providers (APPs) working at multiple Penn Presbyterian facilities across the Philadelphia and New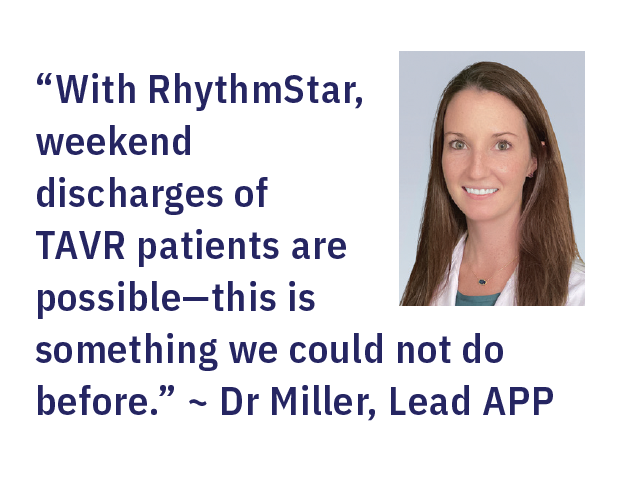 Jersey regions. As the leader for this critical component, Dr Miller has a vested interest in ensuring patients have a positive, comfortable, and clinically reassuring experience when remotely managed.
Jersey regions. As the leader for this critical component, Dr Miller has a vested interest in ensuring patients have a positive, comfortable, and clinically reassuring experience when remotely managed.
Pioneering a New Standard With TTVR Monitoring
In early 2025, Penn Presbyterian launched one of the nation’s first TTVR programs. This minimally invasive procedure replaces a diseased tricuspid valve via catheter-based delivery without open-heart surgery. Patients undergoing this new minimally invasive procedure face a 25% risk of developing conduction abnormalities requiring a pacemaker within the first 30 days. With no existing monitoring protocols or benchmarks, the team adopted RhythmStar for 30-day post-discharge monitoring to help identify early signs of heart block and arrhythmia.
Dr Miller’s insight underscored the unprecedented nature of Penn Presbyterian’s initiative, as it ventured into uncharted clinical territory without historical data to guide decision-making. By leveraging RhythmStar to monitor TTVR patients in near real time, the team was not only responding to an urgent clinical need but also generating the very data that could define future care protocols. This bold approach laid the groundwork for what would become a landmark year of clinical insights.
“There is zero data out there. We are one of the first to monitor this group in near real time,” stated Dr Miller.
Program Outcomes and Arrhythmia Findings
To evaluate the clinical and operational impact of RhythmStar, Penn Presbyterian conducted a comprehensive review of all remote cardiac monitoring studies performed in 2024. The goal was to assess diagnostic yield, time-to-event detection, and modality effectiveness across a diverse patient population.
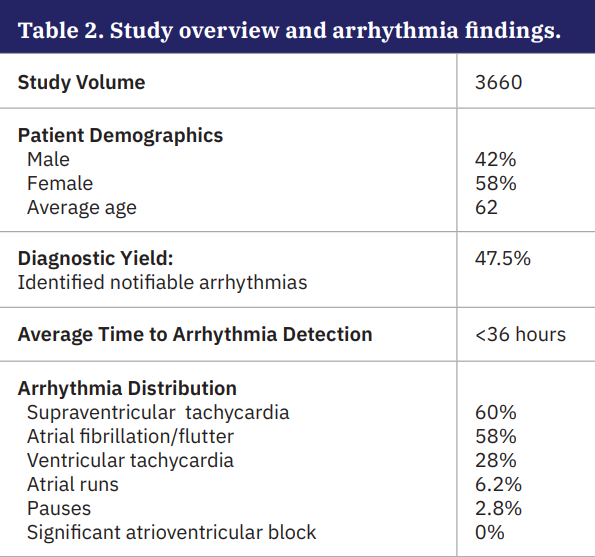
Across almost 3700 patients, 47.5% identified notifiable arrhythmias, underscoring the platform’s effectiveness in capturing clinically actionable events. Importantly, the average time to first arrhythmia detection was just 36 hours (Table 2), allowing for timely clinical intervention. Supraventricular tachycardia was the most common arrhythmia (60%), followed closely by AF/atrial flutter (58%), reflecting the high atrial burden in the monitored population. Ventricular tachycardia (VT) appeared in 28% of cases, while atrial runs and pauses were less frequent (6.2% and 2.8%, respectively). No significant atrioventricular block events were observed (Table 2).
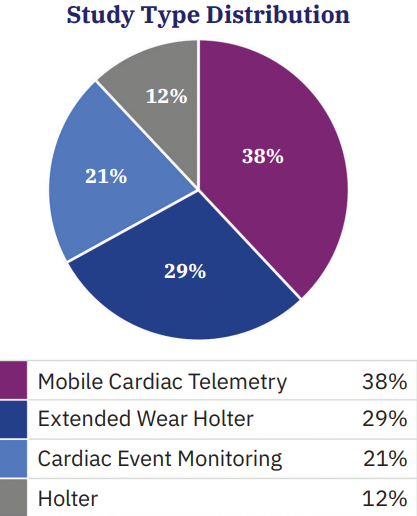
In terms of study type, mobile cardiac telemetry accounted for the largest share (38%), followed by extended wear Holter (29%), cardiac event monitoring (21%), and traditional Holter studies (12%) (Figure 1). These results not only validate the decision to standardize remote monitoring through RhythmStar but also provide valuable data to guide future protocol development, alert customization, and resource allocation.
These results underscore RhythmStar’s role in advancing Penn Presbyterian’s remote monitoring program by delivering both a high detection rate and rapid time-to-event identification. The data continues to fuel workflow optimizations, such as tailored alert configurations and smarter monitoring durations based on when notifiable events are most likely to occur. This continuous feedback loop not only improves patient outcomes but positions Penn Presbyterian to shape future monitoring protocols and perhaps payer policies in high-risk cardiac populations.
From Innovation to Influence: Shaping the Future of Cardiac Care
While these operational and clinical improvements have already begun to reshape how care is delivered, they also highlight a broader opportunity: using the RhythmStar platform not just as a clinical tool, but as a catalyst for innovation. The infrastructure and insights gained through early success positioned Penn to look beyond immediate outcomes and toward research-driven advancements in cardiac care.
The TTVR monitoring initiative also opened the door for future research collaborations. With RhythmStar’s near real-time capabilities, Penn Presbyterian is now exploring partnerships to analyze arrhythmia trends, alert timing, and outcomes. The data may help guide national standards for post-procedural rhythm surveillance and contribute to future device labeling and payer policy decisions.
An important opportunity identified during the rollout was the need for smarter alert customization. Default settings were adequate, but not always relevant to the patient’s clinical indication. Working with RhythMedix, the Penn Presbyterian team proposed integration into their Epic electronic health record ordering workflow, enabling providers to select monitoring intent (eg, AF detection, bradycardia, premature ventricular contraction burden). The goal is to automate alert thresholds based on indication, reducing alert fatigue and increasing signal-to-noise ratio for on-call electrophysiologists.
Additionally, efforts are underway to study the timeline of notifiable events—including how many occur in the first 3, 7, or 30 days—and use that data to refine monitoring duration. The outcome could shape future payer coverage, improve patient adherence, and ensure clinicians get the right data at the right time.
Conclusion: A Scalable Model for Health Systems
Penn Presbyterian’s experience with the RhythmStar Monitor represents a blueprint for how remote cardiac monitoring can, and should, function within an advanced academic health system. The combination of advanced signal processing, near real-time telemetry, human oversight, and responsive service has transformed the EP program into a model of modern, data-driven cardiac care.
For electrophysiologists and cardiology administrators evaluating monitoring platforms, RhythmStar offers a comprehensive solution that aligns clinical excellence with operational scalability. Institutions interested in improving patient outcomes, reducing alert burden, and enhancing workflow integration are encouraged to trial RhythmStar and experience its impact firsthand.
Reference
1. Hahn RM, Makkar R, Thourani VH, et al. Transcatheter valve replacement in severe tricuspid regurgitation. N Engl J Med. 2025;392(2):115-126. doi:10.1056/NEJMoa2401918
Disclosure: Benjamin D’Souza, MD, and Alanna Miller, DNP, CRNP, have completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest,
and have no conflicts of interest to report.
This content was published with support from RhythMedix.











