What the New CONNECT-HCM Digital Registry Means for Electrophysiology
Interview With Matthew Martinez, MD
Interview With Matthew Martinez, MD
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of EP Lab Digest or HMP Global, their employees, and affiliates.
EP LAB DIGEST. 2025;25(9):Online Only.
In this episode, EP Lab Digest sits down with Dr Matthew Martinez, director of Atlantic Health System Sports Cardiology at Morristown Medical Center, to explore the launch of the American College of Cardiology (ACC)’s CONNECT-HCM Digital Registry. Designed to capture real-world patient experiences across diverse care settings, this registry opens new opportunities to understand arrhythmia risk, device therapies, and long-term rhythm outcomes in hypertrophic cardiomyopathy (HCM). We will discuss how the collaboration came together, what makes this registry unique, and how it may transform both clinical research and day-to-day EP practice.

From your perspective, why is this registry such an important development for the care of patients with HCM?
The registry allows patients to enroll directly using their own medical records. That means we can include patients no matter where they receive their care. By giving them the ability to share their charts across providers, we are creating a truly patient-centered, multi-institutional registry. This will finally allow us to follow HCM patients longitudinally in a way we have never been able to before, ensuring that everyone—regardless of where they seek care—can be included in the registry.
This effort represents a collaboration between the ACC, Atlantic Health, Arboretum, and Yale’s Center for Outcomes Research & Evaluation. Can you share how this partnership came together and why it is significant for advancing EP research?
We were invited to help launch the program because we are a high-volume center for HCM care. To identify and achieve meaningful outcome signals for HCM, we need large datasets collected across many centers. A patient-driven model offers the fastest and most effective way to achieve that.
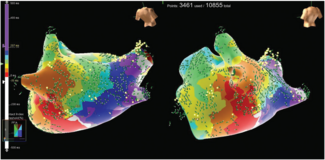
Because the registry links patient health records across different hospitals and providers, it creates a more complete view of the patient journey. How might this help electrophysiologists better understand arrhythmia risk or atrial fibrillation (AF) patterns in HCM?
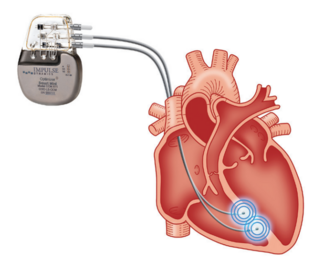
The overall risk of sudden cardiac death (SCD) in HCM is low, but its variable presentation makes it challenging to predict. By analyzing large datasets, we can identify clearer signals that can guide best practices, improve outcomes, and optimize follow-up care.
Participants also receive education tools, including exercise guidance from the latest HCM guidelines. How do you see this type of patient engagement influencing overall EP care?
This is an increasingly recognized and critical part of HCM care. Exercise is medicine—even for patients with HCM. Providing individualized education on safe exercise practices to HCM patients is essential, but we also need large datasets to better understand how to refine those recommendations.
As the registry expands nationally, what opportunities do you see for incorporating EP-specific metrics—such as device therapies, ablation outcomes, or long-term rhythm surveillance—into its framework?
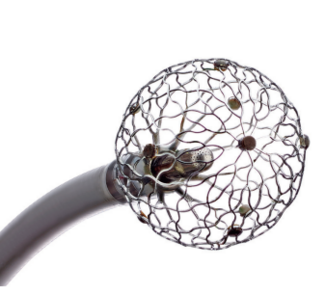
All aspects of HCM care stand to benefit from this registry, but EP in particular—especially management of AF and SCD risk—are areas where we still need refinement. While we have established strategies, there are specific shortcomings in these areas. By identifying current practice patterns, we can design better therapies, research strategies, and treatment algorithms to improve patient outcomes.