Revolutionizing Cardiac Electrophysiology: Advancing Access Site Management, Workflow Efficiency, and Patient Outcomes in High-Volume Electrophysiology Labs
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of EP Lab Digest or HMP Global, their employees, and affiliates.
EP LAB DIGEST. 2025;25(10):14-16.
Interview by Jodie Elrod
In this interview, EP Lab Digest speaks with Luigi Di Biase, MD, PhD, System Director of Electrophysiology at Montefiore Einstein Health System, as well as Professor of Medicine (Cardiology) at the Albert Einstein College of Medicine, about his experience with the LockeT device (Catheter Precision) for access site closure with suture retention.
Can you describe your cardiac electrophysiology (EP) program? As a high-volume EP center recognized for clinical innovation and patient care, what distinguishes your lab’s approach to catheter access site and groin management?
 I serve as the System Director of Electrophysiology (EP) at Montefiore Einstein Health System, overseeing a comprehensive program that spans multiple EP labs across various locations. Each site serves a unique patient population and has its own director, while I provide overarching leadership and coordination for the entire system. For example, at White Plains Hospital in Westchester County, patients often have greater access to support systems, which can facilitate same-day discharge and adherence to medical recommendations. In contrast, patients served in the Bronx may present with more complex clinical profiles and face different social determinants of health, such as limited support at home, which can impact discharge planning and care pathways. These differences reflect the diverse needs of the communities we serve. As the overseeing physician, it is my responsibility to recognize and adapt to these varying circumstances to ensure that every patient receives high-quality, personalized care.
I serve as the System Director of Electrophysiology (EP) at Montefiore Einstein Health System, overseeing a comprehensive program that spans multiple EP labs across various locations. Each site serves a unique patient population and has its own director, while I provide overarching leadership and coordination for the entire system. For example, at White Plains Hospital in Westchester County, patients often have greater access to support systems, which can facilitate same-day discharge and adherence to medical recommendations. In contrast, patients served in the Bronx may present with more complex clinical profiles and face different social determinants of health, such as limited support at home, which can impact discharge planning and care pathways. These differences reflect the diverse needs of the communities we serve. As the overseeing physician, it is my responsibility to recognize and adapt to these varying circumstances to ensure that every patient receives high-quality, personalized care.
We are a high-volume EP lab, performing more than 2000 ablations a year across the system (supraventricular arrhythmias, atrial fibrillation [AF], ventricular tachycardias, and premature ventricular contractions). We perform a similar number of device implants, including a program for lead extraction. In addition, we have a large program on left atrial appendage closure (LAAC), including concomitant cases of LAAC and AF ablation. We also do cardioneuroablation for patients with syncope. In short, there is really no EP procedure that we do not do. We are lucky enough to have most of all the different technologies available on the market today. We are part of the many IDE trials evaluating almost all new technologies and energy sources. It has been exciting to be exposed to all the new tools in the approval and post-approval phases.

How important is access site management in the overall success of a procedure? What are some of the common challenges your team faces with catheter access site closure?
When I speak with EP fellows, I stress that technical success does not always define a patient’s perception of a procedure. After a pacemaker implant, for example, patients often focus less on lead placement or device function and more on the appearance and healing of the wound. Similarly, in ablation procedures, a perfect outcome without arrhythmia recurrence may still be overshadowed by groin pain or a hematoma. Registry data confirm that access site complications—especially hematomas—are the most common adverse events in EP procedures, underscoring the importance of meticulous vascular management.
Early in my career, my mentor and I studied anticoagulation strategies for EP procedures. We found that bridging with low-molecular-weight heparin increased hematoma risk, leading us to adopt uninterrupted anticoagulation, which soon after became standard of care. In this setting, vascular access must be precise, beginning with the first needle puncture. We standardized ultrasound guidance to improve accuracy. Yet, optimal puncture is only half the task—secure closure is equally vital. Once the sheath is removed, inadequate compression or misuse of closure devices can still result in complications.
Because access site complications are frequent, memorable to patients, and relevant across ablation, leadless pacemakers, and any device requiring vascular entry, careful attention to this aspect of care is essential. This applies not only to ablation but also to procedures involving LAA occlusion closure devices, leadless pacemakers, and any intervention requiring vascular access.
Can you discuss the significance of postprocedural workflow in your EP program, and how LockeT fits into or enhances that process?
When discussing workflow, it is important to recall how access site management was performed before closure devices were available. At that time, depending on institutional practice, the heparin effect was either reversed or left unreversed. The sheath was then removed, and manual compression was applied for 20, 30, or even 40 minutes. Proper compression technique was essential, and although time-consuming, it had to be performed correctly. Following compression, patients were required to remain immobilized for approximately 6 hours. This was the starting point for our current practices.
Then, industry introduced closure devices designed to expedite the process. Multiple devices became available, each with slightly different workflows but all aimed at improving procedural efficiency. These closure devices have allowed patients to leave the recovery area sooner and begin ambulation earlier than the traditional 6-hour period. In addition, these devices have been associated with a reduced risk of rebleeding from the access site.
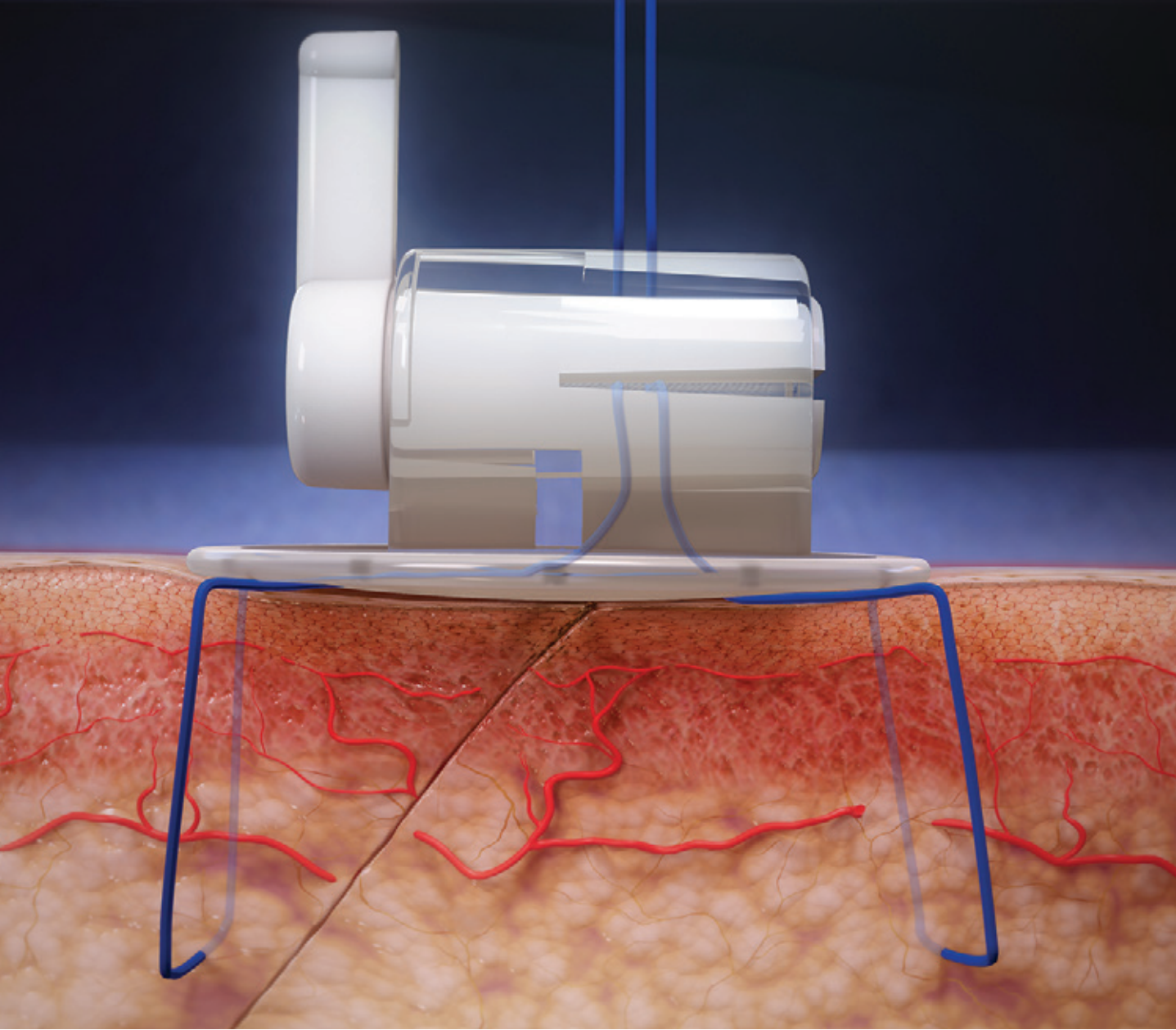
The LockeT is one of several closure devices available for sheath management after a procedure. It is simple to use, requiring placement of a figure-of-8 suture that is not tied but instead secured within the device and locked. The key advantage is if the patient experiences discomfort during postprocedural care, the pressure can be reduced, and if rebleeding occurs, the device can be unlocked to increase compression at the groin. The LockeT is also easily removed. If the patient remains hospitalized overnight, any staff member can remove it by unlocking and pulling the device. Alternatively, patients with average health literacy can be discharged with the device in place and remove it themselves at home, as there is no suture to cut and no additional intervention required—simply unlocking and withdrawing the device.
A second advantage of the LockeT is that only one device is needed per groin, regardless of the number of venous access sites. This contrasts with other closure systems, which typically require a separate device for each vein. As a result, the LockeT is particularly cost-effective: even in cases requiring multiple access sites—such as 4 total, split between 2 groins—only 2 devices are needed, and when 3 sites are obtained from the same groin, a single device still suffices.
The LockeT device features a disc with a locking mechanism on top. Patients often prefer this design because, compared with the figure-of-8 suture secured by a 3-way stopcock, it offers greater comfort and a cost advantage over having no closure device at all. A figure-of-8 stitch with a 3-way stopcock is frequently associated with pain; however, in my experience, the LockeT’s disc design significantly reduces discomfort. Patients are aware of the device’s presence in the groin but rarely report pain, allowing for earlier ambulation and the ability to stand sooner after the procedure. Depending on individual factors—such as living arrangements and absence of comorbidities—same-day discharge (SDD) is feasible, and patients can remove the device themselves at home. Unlike many other closure devices, the LockeT requires no specialized removal process, as there is no suture to cut. Its comfort, ease of removal, and cost-effectiveness distinguish it from other options currently available.
What specific improvements have you seen in your recovery room workflow since adopting LockeT?
The LockeT has allowed us to more quickly prepare the procedure room for the next case. The ability to transition the previous patient out of the room and bring the next patient onto the table as soon as possible is critical for efficiency. Some laboratories prefer to perform manual compression outside the procedure room and wait for the patient to be extubated; in our workflow, we perform this step in the room. With the use of closure devices, procedural delays are no longer attributable to groin access management. We are ready to proceed at the same time the anesthesiologist is prepared, optimizing both room and laboratory time. This benefit applies to all closure devices; however, when combined with the fact that only one device is needed per groin, the gain in laboratory time is achieved at a lower cost. This combination of procedural efficiency, cost-effectiveness, and improved patient experience represents a significant advantage.

Beyond workflow efficiencies, what additional benefits have you and your team observed with LockeT, and which features do you find most valuable in supporting your procedures?
Beyond procedural efficiency, overall cost must also be considered. Ultimately, each procedure should be both clinically effective and cost-effective. While we aim to provide the highest quality compression for the patient, maintaining cost balance is essential—a challenging aspect of procedural planning. For example, if I am performing a case at 6:00 PM with no subsequent cases scheduled, and the patient is elderly and unlikely to ambulate within the next 4 to 5 hours, extended manual compression by staff for an hour may be the most cost-efficient approach, as there is no urgency to expedite discharge.
While I am mindful of the overall procedural cost, extended manual compression is not feasible when procedures occur in the morning and multiple cases are scheduled. Shortening compression to only 20 minutes increases the risk of rebleeding, hematoma formation, and patient discomfort, making this approach impractical in a busy schedule. Closure devices have therefore become integral to our workflow—and to that of EP labs worldwide—because they expedite procedural turnover and are well accepted by patients. However, using the most expensive closure device for every venous access site is not sustainable from a cost perspective. It must be balanced. The LockeT device meets the majority of our critical objectives: it enables safe procedures without complications, is cost-effective, limits the use of additional tools, requires only one device per groin, facilitates early ambulation, and provides a positive patient experience. Overall, its clinical performance and economic value are excellent.

LockeT supports closure of multiple access sites, including large-bore access sites (up to 27 French), with a single device. How has this versatility impacted your procedural approach and patient outcomes?
The LockeT device offers the advantage of requiring only one device per groin, regardless of the number or size of access sites. Some closure devices are limited to certain access sizes, cannot accommodate larger sites, or must be used off-label in such cases. In contrast, the LockeT can be used for any venous access size, eliminating the need to consider sheath diameter when planning closure. In my experience, the device performs consistently well across the full spectrum—from small-caliber venous access to large-bore access—yielding equally favorable outcomes. This versatility represents a significant advantage in procedural planning and execution.
Reflecting on your experience with LockeT, what practical insights would you share with EP labs evaluating its adoption? Have you seen measurable improvements in efficiency—such as improved staff utilization, enhanced patient comfort during bedrest, or a reduction in cost—as a result of integrating LockeT into your catheter access site closure strategy?
The LockeT device performs effectively, is cost-efficient, and is well accepted by patients. It is compatible with a variety of access site sheath sizes and can be applied quickly. Overall, I consider it a valuable tool for use in every EP lab practice.
The transcripts were edited for clarity and length.
Disclosure: Dr Di Biase has completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest, and reports consulting fees from Abbott, Boston Scientific, Medtronic, Siemens, Stereotaxis, ZOLL Medical, Haemonetics, and Johnson & Johnson MedTech.
This content was published with support from Catheter Precision.











