Inside the Future of Electrophysiology: Four-Dimensional Intracardiac Echocardiography and the Evolution of Concomitant Atrial Fibrillation and Left Atrial Appendage Occlusion Procedures
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of EP Lab Digest or HMP Global, their employees, and affiliates.
EP LAB DIGEST. 2025;25(9):19-21.
Interview With Apoor Patel, MD
In this interview, EP Lab Digest speaks with Apoor Patel, MD, to discuss atrial fibrillation (AF) and left atrial appendage occlusion (LAAO) concomitant procedures at Houston Methodist Hospital using the 4D ICE NUVISION Ultrasound Catheter (Johnson & Johnson MedTech), including patient benefits, economic value, and the future for these procedures.
Can you describe your transition from transesophageal echocardiography (TEE) to intracardiac echocardiography (ICE) for LAAO procedures? What motivated the shift, and how has it changed your workflow?
When I first began performing LAAO procedures, I was using TEE. This was soon after the appendage closure was first introduced. I had the same 2 cardiologists doing all my TEEs, which led to good consistency and quality. While the imaging quality was excellent, there were notable logistical challenges, particularly in coordinating schedules among the electrophysiology (EP), cardiology, and anesthesia teams. Delays occurred during the procedure due to staggered arrivals, as these departments typically do not converge simultaneously at our institution.
A few years later, I transitioned to a different practice, where the responsibility for TEE had shifted from cardiology to cardiac anesthesia. The personnel now performing the imaging varied from case to case, leading to significant variability in both image quality and interpretation, and there were the ongoing challenges of coordination between the services.
My colleague was skilled at using 2-dimensional (2D) ICE for appendage closure, so I decided to adopt that workflow. To make the procedure easier, I started with 2D ICE and CARTOSOUND (Johnson & Johnson MedTech), which was incredibly helpful in visualizing how the ICE fan or imaging plane cut through the 3-dimensional (3D) anatomy. This allowed me to better understand catheter position and device orientation. I could ensure that I had imaged the device in multiple coaxial planes. We eventually published a guide on how to do this in Heart Rhythm.1
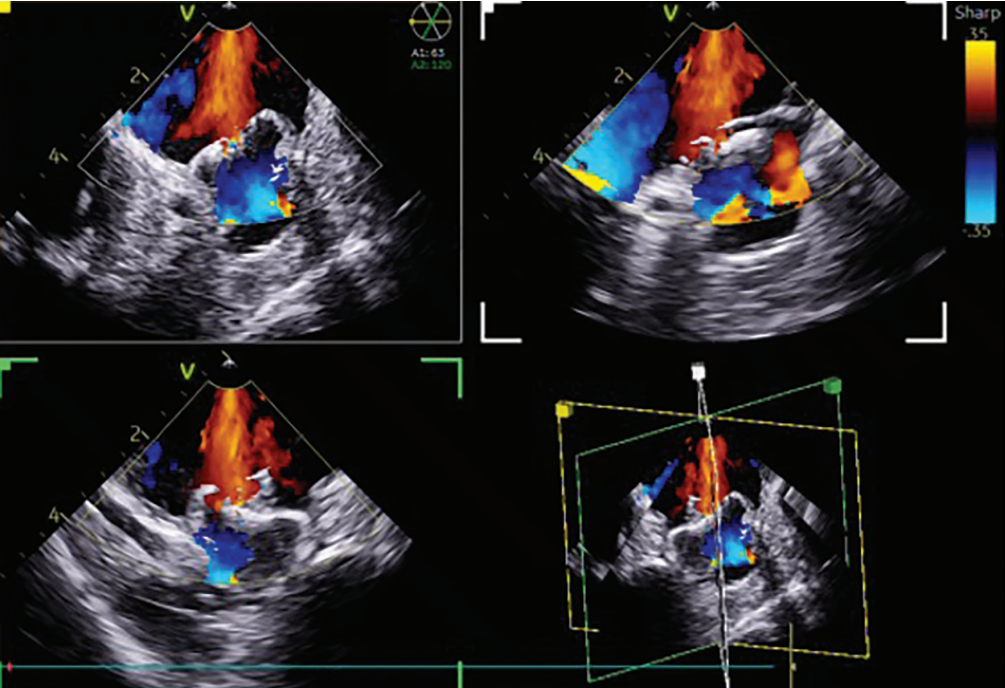
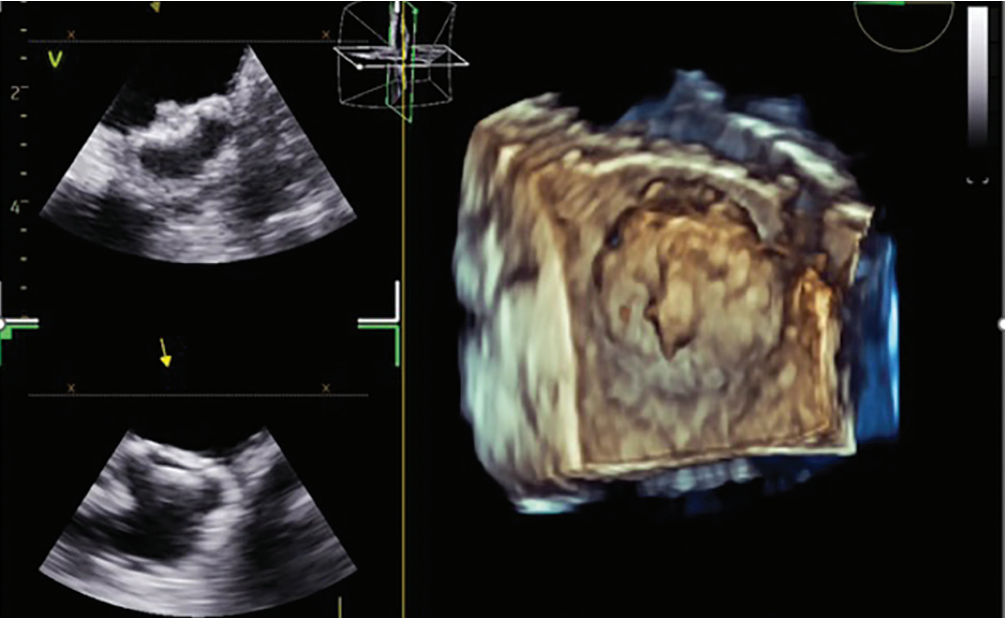
I then transitioned to the 4D ICE NUVISION Ultrasound Catheter and found that it offered superior image resolution with much less catheter manipulation due to the catheter design, as compared to 2D ICE. You can place the catheter in the left atrium in different places, and with minimal manipulation, gather the images that you need in 2D, 3D, and 4D due to its wide imaging field. The ultrasound specialist can provide multiple imaging planes at the same time, so you can quickly and coaxially visualize the device without having to manipulate the catheter. Use of ICE and NUVISION afforded more predictability, more consistent quality, and more control over the imaging, which has facilitated the implant process for me.

In what ways has NUVISION 4D ICE improved procedural efficiency and patient comfort—especially in hospitals with limited anesthesia resources or echo support?
Certainly, there are procedural benefits to using NUVISION, including less coordination needed with anesthesia, the echo technician, or additional cardiologists. General anesthesia is not required for all cases; conscious sedation may be used in selected patients and is often preferable. The patients wake up feeling better, and not having to do a TEE eliminates the patient discomfort that comes with TEE and intubation. Thus, use of NUVISION can be especially valuable in settings with limited anesthesia or echo resources, which is fairly common throughout the country. The ability to use NUVISION, maintain a predictable workflow, and reduce reliance on anesthesia provides a significant clinical advantage.
We assess the anesthesia needs of each patient on a case-by-case basis. Not all patients can get a device under conscious sedation—some of them need deeper sedation because they cannot tolerate lying flat, for example. We ask a series of questions, such as: how well can they breathe lying flat? How sick are they in general? What are their comorbidities? How bad is their ejection fraction? What is their lung function? All these factors influence the decision to involve anesthesia or to proceed with conscious sedation. They are integral to the clinical decision-making process.

How does NUVISION 4D ICE compare to 2D ICE in terms of value under MS-DRG-317, and has this influenced your imaging choices for LAAO or concomitant procedures?
Both 2D ICE and 3D/4D NUVISION are viable options for concomitant procedures, but using ICE alone is preferable to combining ICE and TEE, which is still what is commonly done. There are many procedures where 2D ICE is used for transseptal and TEE is used for stand-alone appendage closure and with concomitant procedures, which increases complexity and potentially cost to the case in general. There is a cost associated with TEE in terms of labor and additional personnel. Being able to do everything with one catheter facilitates the implant process.
Our group published a cost analysis looking at 2D ICE versus TEE for stand-alone appendage closure and found that total costs were roughly equivalent. While I cannot comment on the value of using NUVISION for concomitant procedures without a formal analysis, its ability to serve dual roles—guiding both ablation and appendage closure—strongly suggests a cost and workflow advantage in my mind.
Should 4D ICE be considered the standard imaging tool for LAAO, particularly in light of the CHAMPION and OPTION trial outcomes? How do these results validate your current practice?
Although data from the CHAMPION trial are not yet available, if the results are favorable, this data, in conjunction with the recently published OPTION trial, will likely establish LAAO as a viable option across broader patient populations. As the field evolves, 4D ICE such as NUVISION is well positioned to become an increasingly important imaging modality. Given the anticipated growth of LAA procedures and the limited capacity of hospitals and anesthesia resources across the country, I can see 4D ICE gaining usage because it reduces the need for TEE and general anesthesia, reducing strain on hospital and anesthesia resources. At the same time, it delivers high-resolution, real-time imaging that is critical for safe and effective device deployment. In the OPTION trial, use of ICE for appendage closure was 2%, so most operators were still using ICE for the ablation and TEE for appendage closure. As time goes on, I think there is significant room for growth with 4D ICE to be used for both.
What ripple effects do you expect from OPTION and CHAMPION in shaping broader clinical adoption of 4D ICE? How might this shift influence future ICE usage?
The OPTION and CHAMPION trials will likely accelerate the shift away from TEE and more toward ICE, especially in EP-driven labs, for concomitant procedures and even for just stand-alone appendage closure. As LAAO becomes more widely adopted—particularly in combined procedures—ICE offers scalability and independence from echo-specific resources.
This broader adoption will likely drive investment in operator training, device development, and platform integration. We are seeing the beginning of a paradigm shift where ICE is not just an alternative, but the first-line approach for appendage closure and potentially other structural interventions. We are starting to see that as well with mitral valve procedures and tricuspid valve interventions.
What makes NUVISION particularly beneficial for concomitant cases, and how is it supporting your team in procedures involving atrial fibrillation, LAAO, or pulsed field ablation (PFA)?
It is still common to use ICE for the transseptal and TEE for appendage closure. I think this adds procedural complexity, requires significant coordination, and increases patient discomfort due to the need for a TEE. The use of NUVISION for both procedures gives the electrophysiologist control over imaging quality for PFA and appendage closure. I think we have realized the importance of contact with PFA, not just with respect to lesion efficacy, but also with regard to hemolysis. When placed in the left atrium, NUVISION can be tremendously helpful due to its superior imaging quality and limited need for manipulation. We can clearly assess contact in the pulmonary veins and posterior wall and then use the same catheter for appendage closure. With a single catheter, we can visualize ablation targets and then immediately assess and guide appendage closure—all under one workflow.
With NUVISION NAV on the horizon, how do you see features like remote user interfaces (UI), CARTOSOUND integration, and catheter tracking changing the way you perform your procedures?
I believe NUVISION NAV will be a game changer. I am most excited about CARTOSOUND integration—the ability to see the imaging plane superimposed on a 3D map will improve spatial orientation for both ablation and appendage closure. Remote UI will allow the CARTO clinical to meaningfully integrate ultrasound-guided anatomy with activation mapping. It will make ablation and appendage closure more intuitive for most operators and ensure adequate device imaging. We have data showing that 4D ICE as compared to 2D ICE is associated with fewer device redeployments. You are more likely to get the device in on the first or second try than with 2D if using 4D ICE. So, imaging quality and accuracy can really make a difference when it comes to appendage closure.
The ability to track the ablation catheter within the ultrasound field will enhance lesion visualization and contact assessment. I see this as being particularly helpful in challenging sites such as papillary muscle premature ventricular contractions (PVCs)—being able to track the catheter as you are moving along the papillary muscle in the ultrasound field will be beneficial. In general, it will facilitate ablation efficacy and real-time lesion assessment.
Looking forward, what gives you confidence that the NUVISION platform/portfolio will continue evolving with EP practice needs and trial-driven protocols?
Johnson & Johnson MedTech has made tremendous leaps with their ultrasound technology. While there has been so much focus on PFA, I think people have overlooked the developments that have been happening with ICE. The imaging quality has improved, and now with 4D integration into electroanatomic maps, there is much potential for it to improve ablation outcomes as well as LAA closure. The utility of ICE will be beyond just high-quality imaging; I believe there will be a role for ICE to assess the quality of the appendage closure and to assess lesion formation with ablation. ICE penetration is still low with regard to appendage closure in the United States and worldwide. Some of this represents issues with cost, but another reason is that users may not always feel comfortable manipulating the ICE catheter. I think that NUVISON NAV, which will be intuitive to use, can democratize the process for ICE usage for appendage closure. In addition, as structural cardiology and valve interventions continue to grow, there is tremendous potential for NUVISION and NUVISION NAV to facilitate these procedures. I am excited to see what the future holds with ultrasound and how it is further integrated into ablation procedures—not just AF ablation procedures, but PVC and ventricular tachycardia (VT) ablations, concomitant AF ablation procedures, and appendage closure.
Is there anything else you’d like to add?
I would like to recognize the exceptional team I work with every day at Houston Methodist. We are part of a dynamic and growing EP program, where collaboration, skill, and dedication drive our success. Our team performs a high volume of complex procedures, including AF ablations, device implantations, LAA closures, and ventricular tachycardia ablations. Our staff is well-trained, cohesive, and committed to excellence. We are proud to be part of an institution that fosters continuous growth and clinical excellence.
Reference
1. Patel A, Venkataraman R, Schurmann P, Dave A, Valderrábano M. Left atrial appendage occlusion using intracardiac echocardiography. Heart Rhythm. 2021;18(2):313-317. doi:10.1016/j.hrthm.2020.09.021
Disclosure: Dr Patel has completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest, and reports honoraria from Johnson & Johnson MedTech for lectures.
This content was published with support from Johnson & Johnson MedTech.
US_ELP_ULTR_405001











