Fluoroless Radiofrequency Ablation With Esophageal Protection: Interview With Brett Gidney, MD
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of EP Lab Digest or HMP Global, their employees, and affiliates.
EP LAB DIGEST. 2025;25(6):12-13.
Interview by Jodie Elrod
 Dr Brett Gidney, a cardiac electrophysiologist at Marian Regional Medical Center in Santa Maria, California, discusses his recent incorporation of the esolution® esophageal retractor device (S4 Medical) into his paroxysmal and persistent radiofrequency (RF) workflows. The esolution has an indication for reducing the risk of thermal injury in any atrial fibrillation (AF) ablation modality.
Dr Brett Gidney, a cardiac electrophysiologist at Marian Regional Medical Center in Santa Maria, California, discusses his recent incorporation of the esolution® esophageal retractor device (S4 Medical) into his paroxysmal and persistent radiofrequency (RF) workflows. The esolution has an indication for reducing the risk of thermal injury in any atrial fibrillation (AF) ablation modality.
How did you find out about the esolution device?
When the EASY AF trial results1 were published, I read them with interest and thought that esophageal deviation performed with the use of the esolution device would be a good fit. I liked the control of movement that it offered, rather than fixed movement. I also liked the steerability aspect of it. I contacted the company, was an early adopter, and it stood up to my expectations.
Tell us about how you use intracardiac echocardiography (ICE) plus esophageal protection for a fluoroless procedure.
Fluoroscopy is not good for anyone, especially the repeat exposure received by the EP team, so I look for any way possible to utilize mapping and ultrasound rather than ionizing radiation. I have been using CARTOSOUND® (Johnson & Johnson MedTech) to overlay the esophagus on my map for some time, and so I was curious whether I could translate this technique over to the esolution device.
What I found is that the esolution device has landmark features and echogenic materials that provide excellent visualization with ICE. I start my procedure by identifying the initial position and overlay this onto my map. I can then assess whether deviation is needed, and if so, I deviate and then perform another overlay. As I am performing my ablation, I will use the overlay for guidance, but I can quickly check with ICE to confirm that I still have adequate distance. Working with my mapping specialist, we have become very proficient at performing our overlays and periodically confirming position.
In combination with esolution, the whole workflow is fluoroless. Working with S4 Medical, we have developed a good technique that gives me peace of mind that I am providing enhanced safety to the patient as well as the EP team in a way that integrates well into the workflow.
Is this an easily translatable technique for other electrophysiologists?
I think this approach and process to identify the esophagus is easily transferable to most electrophysiologists who are using CARTOSOUND and mapping. Further, the esophageal retractor has great features to easily identify position.
It was eye-opening to realize that with this device, I was in control of the esophagus rather than the esophageal location controlling me. With the use of esolution, the anxiety of the esophagus fades away once you see it has been relocated away from the ablation energy. There are also additional workflow tweaks that we have discovered along the way that have helped the procedure overall.
Tell us more about some of those procedural tweaks.
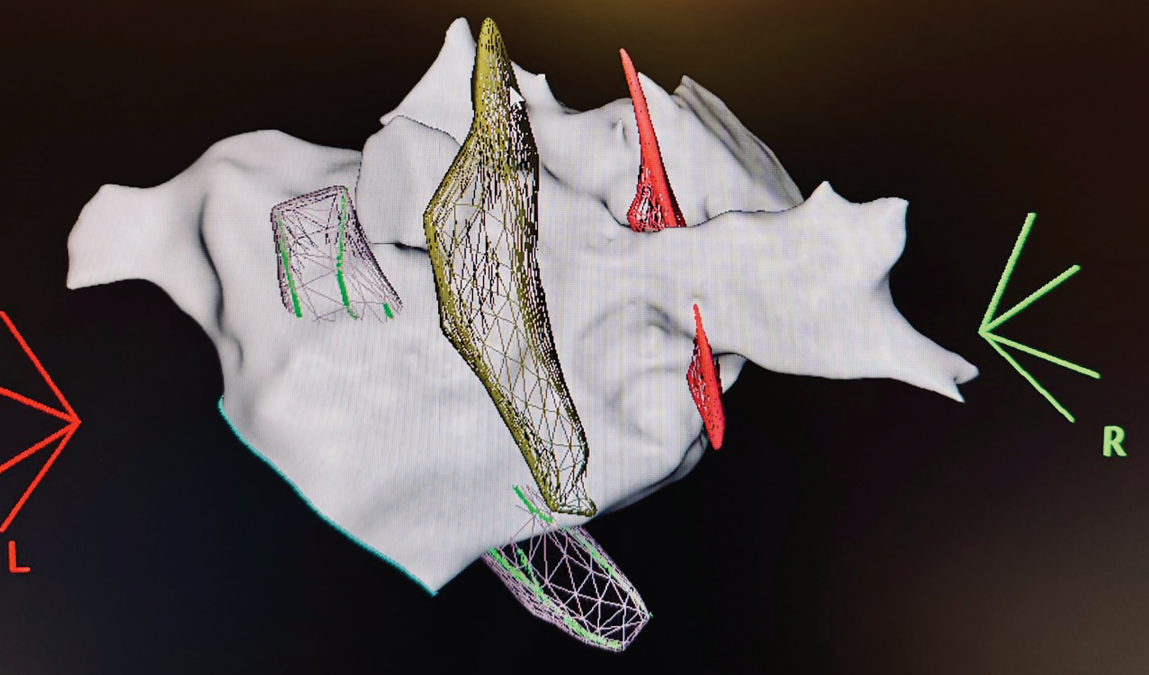
Moving the esophagus can alter the anatomy, so we often build the anatomical shell with the retractor withdrawn and slide it behind the target location followed by deviation only when we are ready to ablate. It can take a few seconds to complete moving, so after deviation, we keep an eye on it with ICE and begin creating the ultrasound contours after it has completed movement with suction applied (Figure). We learned that each patient is different, so while in some we place the probe directly behind the planed ablation site followed by deviation, we often experiment and place it slightly above or below with much better results. Finally, in a small number of patients, the esophagus will not move much, so we withdraw the device above the level of the left atrium.
Does esophageal protection make you rethink the choices for ablation modality?
As pulsed field ablation (PFA) is new to the US market, the vast majority of the AF ablations I have performed in my career have been with thermal energy. Current RF technology is highly evolved, very well understood, and predictable. The latest RF catheters can deliver high power/short duration energy with temperature and force feedback to give us an exquisite level of lesion control. One of the things we have noticed with the current generation of PFA technology is a challenge with achieving adequate ablation depth. The consequence is that we are seeing more reconnection of veins than we have seen with thermal ablation.
So, the reconnections from PFA procedures we have seen are often where we normally identify thicker areas of the atrium. This has been a point of frustration with PFA, and we have had some patients come back with more symptomatic atrial arrhythmias due to the multiple reconnected and discrete reconnections of the pulmonary veins (PVs) that result in atrial tachycardias rather than fibrillation. Further, when you get reconnections that were performed with PFA, there is no point in applying the same generation of PFA again.
Specifically, there are areas by the posterior part of the right carina and inferior to the left inferior where the esophagus can be very close, yet the tissue is thick. I like RF for the ability to titrate and control the delivery of energy, and esophageal protection gives me the ability to comfortably ablate and maintain safety.
When we look back at the atrial-esophageal fistulas that occur, it is generally impossible to figure out why it happens in some patients and not in others. It can happen regardless of the attention to temperature monitoring, identification of the location of the esophagus, and careful ablation technique. Moving the esophagus out of the way is the safest and most secure way of applying energy.
Other than increased safety, did you find any other benefits (such as speed, power/delivery, etc)?
Because the esophagus always runs on the posterior wall, even with PV isolation-only procedures, you still need to apply energy to the posterior wall, and you inevitably will have to make some compromises on the posterior wall. Some patients require additional lesion sets on the posterior wall, which become stressful or impossible near the esophagus. Using esolution gives me more security to create durable lesions with the energy that I select. I no longer feel handicapped by the location of the esophagus forcing me to use a specific setting. I can do what is right for that specific anatomy because the esophagus is now in my control. n
The transcripts were edited for clarity and length.
Disclosures: Dr Gidney has completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest. He reports consulting fees, support for attending meetings and/or travel, and payment or honoraria for lectures, presentations, speakers’ bureaus, manuscript writing, or educational events, from Johnson & Johnson MedTech, Medtronic, and Boston Scientific. He also reports participation on a Data Safety Monitoring Board or Advisory Board from Johnson & Johnson MedTech.
This content was published with support from S4 Medical.
Reference
1. Weiss R, Osorio J, Nair D, et al. EsophAguS deviation during radiofrequencY ablation of Atrial Fibrillation: the EASY AF trial. JACC Clin Electrophysiol. 2024;10(1):68-78. doi:10.1016/j.jacep.2023.09.004











