Concomitant Atrial Fibrillation Ablation and Left Atrial Appendage Occlusion: Practical Strategies for Safer, Smarter Adoption
Interview With Manish Shah, MD
Interview With Manish Shah, MD
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of EP Lab Digest or HMP Global, their employees, and affiliates.
EP LAB DIGEST. 2025;25(11):8-11.
Interview by Jodie Elrod
Manish Shah, MD, shares candid reflections on patient selection, workflow optimization and key lessons learned from performing concomitant atrial fibrillation (AF) ablation and left atrial appendage closure (LAAC) procedures. From addressing patient perceptions to integrating evolving technologies like pulsed field ablation (PFA), the discussion provides an in-depth look at the challenges and strategies that can transform uncertainty into confidence. For physicians considering concomitant AF ablation and LAAC, these insights offer practical guidance to streamline adoption and maximize both patient and procedural benefit.
 Can you start by briefly introducing yourself?
Can you start by briefly introducing yourself?
I am a cardiac electrophysiologist at MedStar Washington Hospital Center. I am the program director for the cardiac electrophysiology (EP) program and do a considerable amount of WATCHMAN (Boston Scientific) device implantation as well as catheter ablation of AF.
What patients do you discuss concomitant procedures with? Are there any you avoid?
That is a great question. Our approach to selecting patients for concomitant procedures is rapidly evolving. Much of our decision-making is guided by data from the OPTION study, which demonstrated 2 key points: first, the equivalence of the WATCHMAN device to newer oral anticoagulants (95% NOAC), and second, the safety of the WATCHMAN device in a concomitant fashion, allowing both procedures to be performed together. With those findings, and the demonstrated improvement in overall bleeding rates among patients who receive the WATCHMAN device, we now consider a broader range of patients with AF.
For example, patients with symptomatic AF—either paroxysmal or persistent AF—who are interested in catheter ablation are often appropriate candidates for discussion. We carefully evaluate several factors such as bleeding risk, the need or desire to take nonsteroidal anti-inflammatory drugs and prior history of anemia. All of these considerations go into our decision-making. Ultimately, the data from the OPTION study underpins our confidence in offering concomitant therapy.
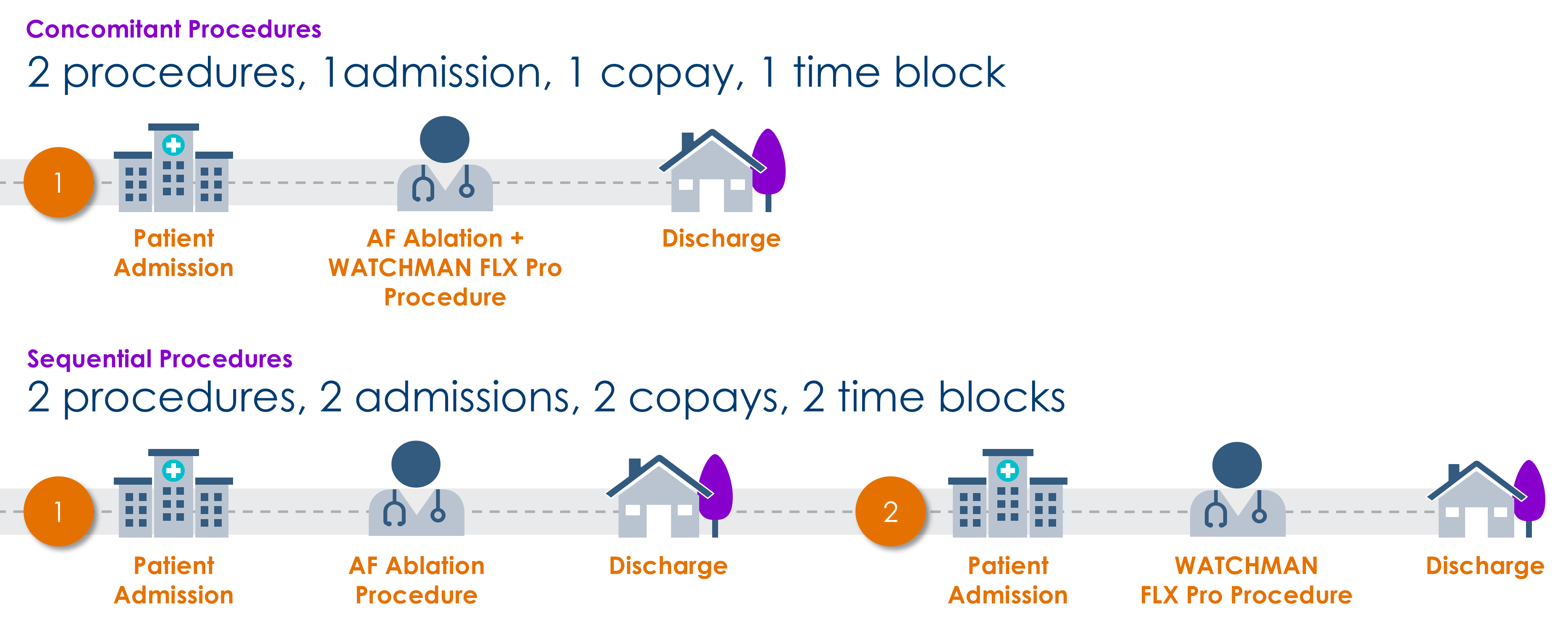
How have patients responded to the option of combining procedures? Are they generally receptive, and how do you present the potential benefits during consultations?
Quite frankly, the response has been overwhelmingly positive. Patients are thrilled that we can accomplish everything utilizing a concomitant approach rather than 2 separate procedures, which many view as unnecessary. They often ask, “Is it safe to do both at the same time?” We now have ample data showing that adding a WATCHMAN procedure to an ablation does not result in an increased complication rate. So, patients truly appreciate the improved safety profile with a concomitant approach and are overall very pleased to have everything completed in one visit.
How did the concomitant and sequential subgroup analysis from OPTION inform the safety and efficacy of concomitant ablation and WATCHMAN?
The efficacy data is quite strong. The study met the noninferiority criteria, which means that the WATCHMAN device is just as effective as blood thinners in reducing stroke risk—and in fact showed numerically fewer stroke or systemic embolism events. This is an important point because prior to the OPTION study, we did not have a solid comparison between the WATCHMAN device and newer blood thinners (95% NOAC) like apixaban or dabigatran. So, I think patients are reassured by this efficacy data.
The safety data is also encouraging. Among the 40% of patients in the OPTION trial who underwent a combined procedure, the cumulative complication risk within 7 days of the ablation procedure was about 2.1% with a combined approach, compared with about 2.7% from the ablation only. So, there was no increase in procedural events with concomitant WATCHMAN FLX implantation. In addition, the cohort who received the WATCHMAN device had significantly fewer bleeding episodes—a 50% risk reduction in ISTH bleeding at 36 months, inclusive of procedural bleeding—which was a major outcome of the study. Patients are excited by these results, as many dislike taking blood thinners and often experience clinically relevant but nonmajor bleeding, which drives their decision-making.
Can you describe the workflow you have developed for performing concomitant AF ablation and LAAC?
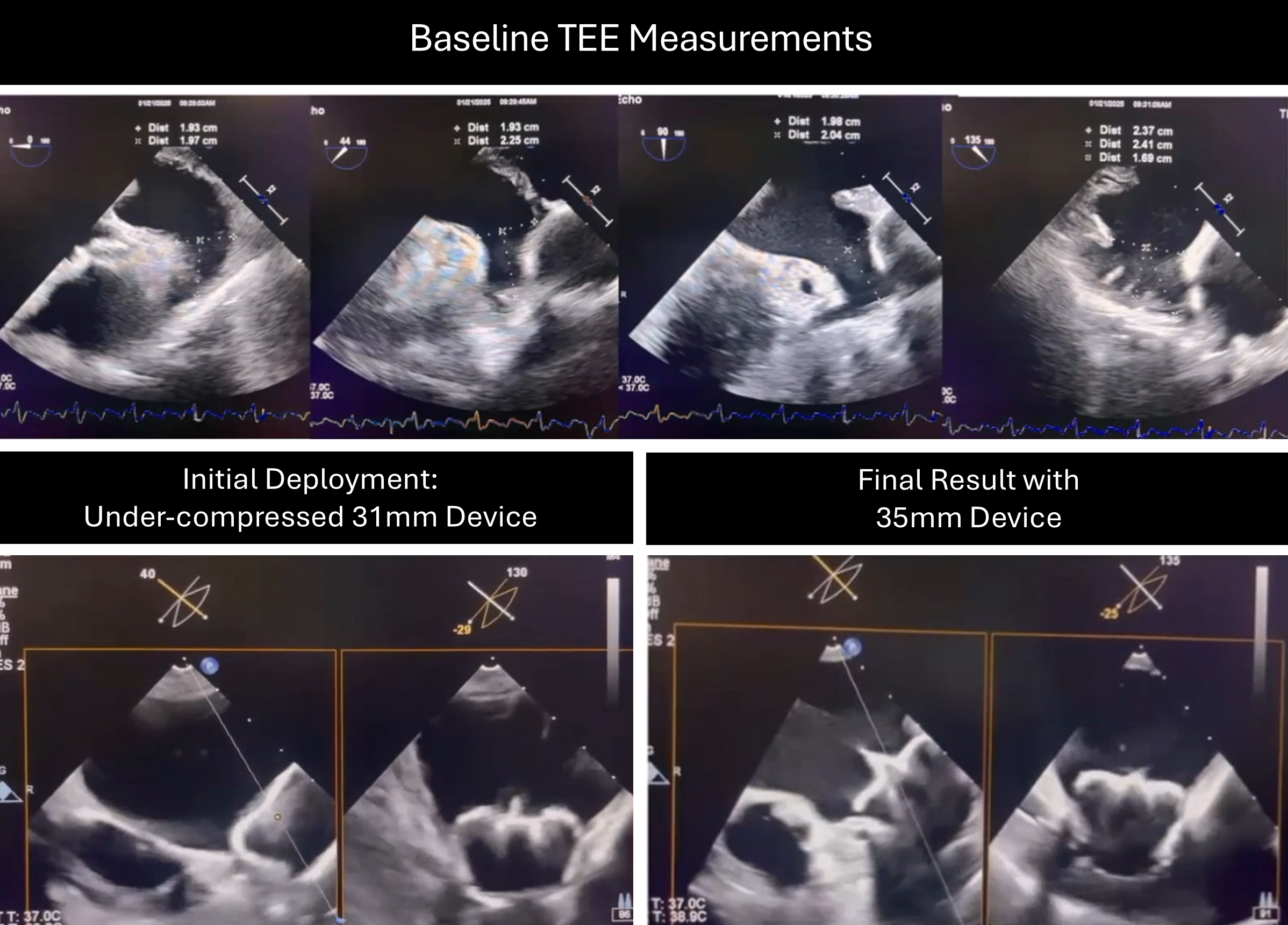
As a general rule, when scheduling patients for concomitant procedures, we obtain preprocedural imaging with a computed tomography (CT) scan. We do that for a few reasons. First, it excludes any thrombus in the LAA. Just as important, it gives us valuable sizing information prior to performing catheter ablation. For example, when performing an ablation, we know that some patients may develop tissue edema around the areas where we are going to place the WATCHMAN device. So, having preablation measurements—which for us is best achieved with a CT scan—helps us identify the size of the device in advance.
We have also used intracardiac ultrasound (ICE) and transesophageal echocardiography (TEE) as imaging modalities, but for our workflow, TEE is preferred. Typically, once the patient is intubated and prepared for catheter ablation, we perform PFA with the FARAWAVE NAV™ PFA catheter (part of the integrated FARAPULSE™ Platform) for pulmonary vein isolation, and, in some cases, posterior wall treatment. We then exchange catheters or sheaths for the WATCHMAN access sheath and deploy the device under TEE guidance. This requires close coordination with our noninvasive colleagues who perform the imaging; they have been great to work with, and we receive great images that facilitate precise device delivery.
We have been able to complete these combined procedures in a predictable manner, which is something that would have been difficult to imagine just a few years ago. We are excited to be able to offer both AF ablation and LAAC utilizing a concomitant approach.
Having performed concomitant procedures regularly for over 18 months, what lessons have you learned that you wish you had known at the outset?
The first thing I have realized is just how grateful patients are. At follow-up visits, they are thrilled—sometimes they even want to give you a hug—because not only have we treated their AF, but we have been able to get them off their blood thinners. For many patients, that is incredibly meaningful. It lowers their overall risk, and the satisfaction I see in my concomitant patients is truly off the charts—which is important.
The second lesson is that concomitant procedures require some experience with WATCHMAN device implantation. At our institution, we have many expert ablation attendings who are still early in their WATCHMAN experience. For those individuals, we encourage a deliberate approach, since it can take time to become comfortable with this new technology. Not everyone is immediately proficient with the WATCHMAN device, so rolling it out safely is critical. For us, using TEE has been the preferred approach as we view it as the standard way to learn WATCHMAN device implantation. This has been a valuable method for bringing our colleagues into the workflow as they gain WATCHMAN experience.
What do you see as the most significant benefits of combining AF ablation and LAAC in a concomitant case?
Our patients love it, and our confidence has grown significantly with the OPTION dataset. Before those results were available, there were some open-ended questions about the efficacy of the device compared with newer medications. Now we have much clearer answers, and we expect even more information in the near future from the CHAMPION study. Overall, I believe most of our patients are excited about the opportunity to have everything done in one sitting.
With the rise of PFA, how has your AF ablation practice changed, and has this influenced your approach to concomitant procedures?
I am not sure the concomitant procedure could be easily done without a platform like FARAPULSE PFA—these technologies have really made AF ablation predictable. Before this technology, there was more uncertainty around procedure time and predictability. Now we can schedule consistently, because we know exactly how long the procedure will take. In addition, the risks associated with the procedure have been significantly reduced, which has improved overall procedural safety. With FARAPULSE PFA as our ablation tool set, we feel much more confident about offering a combined approach.
There is ongoing discussion around LAA tissue edema postablation and its impact on device sizing and placement. What steps do you take to manage this during concomitant procedures?
Preablation imaging can be very helpful to determine whether tissue edema is present. It is not seen in every patient—only a minority of patients show edema significant enough to influence our decision-making—but when we do see it, we typically opt for a larger size device when possible, allowing sufficient depth for safe delivery of the WATCHMAN device. We select the largest device that will appropriately fit the appendage. Sizing to achieve about 25% to 30% compression has become fairly standard for concomitant patients.
In follow-up, across roughly 40 to 50 of my patients, outcomes have been very reassuring. We have not seen a high incidence of leaks or device-related thrombus on post-procedural imaging.
What would you say to peers who are still doing sequential procedures or are hesitant to combine therapies?
First, your patients will truly appreciate what you are doing for them with concomitant procedures. They feel you have saved them not only time but, more importantly, reduced their risk. Patients intuitively understand that 2 separate procedures carry a higher risk than a combined approach, even in experienced hands. So, they appreciate that.
Second, if you are already familiar with the WATCHMAN device, then performing it concomitantly should come with ease. If you are less experienced with the WATCHMAN, but more experienced with catheter ablation, be patient—there is a learning curve of about 10 to 20 cases before you start to feel confident. Give yourself time to get there.
Disclosure: Dr Shah has completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest. He reports payment to his institution for research-related costs for the SIMPLAAFY Study, OPTION Study and CHAMPION Study. He reports that he is a consultant/advisor to Boston Scientific and has received support from Boston Scientific for attending meetings and/or travel.
The transcripts were edited for clarity and length.
This content was published with support from Boston Scientific.











