UCHealth Memorial Hospital
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of EP Lab Digest or HMP Global, their employees, and affiliates.
EP LAB DIGEST. 2026;26(1):16-18.
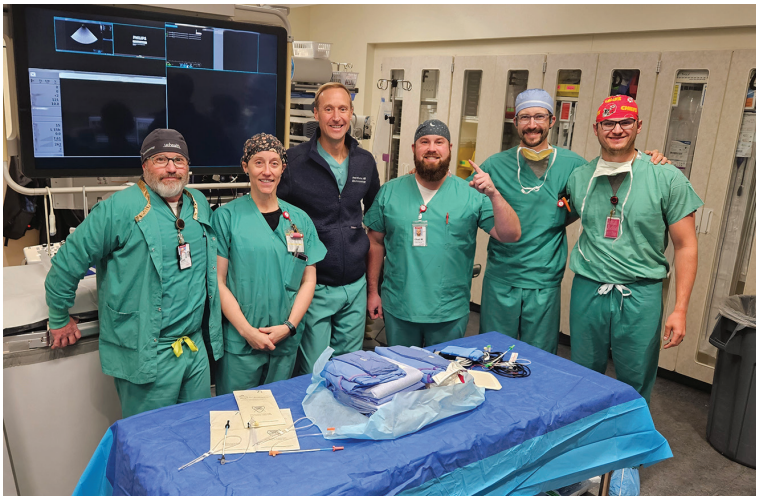
Katie Smith, RCIS, and Lindsay Salas, BSN, RN
UCHealth Memorial Hospital, Colorado Springs, Colorado
When was the cardiac electrophysiology (EP) program started, and by whom? What drove the need to implement an EP program?
The EP program has a long-established presence within the organization. As the patient population grew rapidly and leadership brought on an additional electrophysiologist, the need to expand services to the north hospital became clear. This expansion required a specialized EP team focused on these procedures. The EP team separated from the main cardiac catheterization laboratory staff about 5 years ago.

What is the size of the EP lab facility? Has the EP lab recently expanded in size, or will it soon?
The EP staff covers 2 campuses, with one designated EP lab at each facility. The plan is to expand the specialty by adding another EP lab at the main campus, which will provide 3 dedicated EP labs in total.
Who manages the EP lab, and what is the mix of credentials and experience? What is the number of staff members?
The central EP lab is managed by Audrey Taylor, MSN, RN, CCRN, and the north EP lab is managed by Stephen Andersen, MHA, EP-C. The program includes 11 staff members, consisting of registered nurses (RNs) and registered cardiovascular invasive specialists (RCISs), as well as 3 electrophysiologists—Jaime Gonzalez, MD; Ryan Borne, MD; and Brad Mikaelian, MD. Anesthesia is typically provided for all procedures. Nurses in the EP lab circulate, administer medication, scrub, and perform programmed electrical stimulation. In Colorado, RNs must hold RCIS or registered cardiac electrophysiology specialist certification to operate x-ray equipment. EP technologists also scrub and operate the external stimulator to perform programmed electrical stimulation. Each campus is staffed by 4 team members who rotate through the roles of the lab.
What types of procedures are performed?
Procedures performed include radiofrequency ablation for supraventricular tachycardia (SVT), atrial flutter (AFL), ventricular tachycardia (VT), premature ventricular contractions (PVC), and Wolff-Parkinson-White (WPW) syndrome); pulsed field ablation [PFA] for atrial fibrillation (AF) and AFL; left atrial appendage occlusion (LAAO); implantation of the remedē System (ZOLL Medical) for central sleep apnea, implantation of permanent pacemakers (PPMs), implantable cardioverter-defibrillators (ICDs), and biventricular devices; Micra (Medtronic) leadless pacemaker implantation; concomitant procedures; procainamide challenges; and implantable loop recorder placement.
Approximately how many ablations, device implants, and LAAO procedures are performed each week?
On average, 11 PFAs, 6 concomitant procedures, 5 ablations, 5 ICD implantations, 2 biventricular device implantations, and 2 PPM implantations are performed each week across the separate campuses.
Tell us about a typical day in the EP lab.
The day begins at 0700, with the first case start time of 0730. Each day, procedures are typically clustered by type, focusing on devices, PFA, concomitant procedures/LAAO, and other ablations. Mondays may include 4 to 5 PFA/LAAO cases at the main campus and SVT ablation and PFA at the other campus. Tuesdays may be designated for device cases, such as 5 to 6 PPM, ICD, biventricular, or Micra implantations. Wednesdays may include PFA/LAAO procedures at the main campus with a different physician, and generator change, VT ablation, and PFA at the other campus. Thursdays may include Watchman device (Boston Scientific) implantation and PFA/LAAO procedures at the central campus. Fridays may include lead revision, SVT ablation, and PFA at the main campus, and PFA, PVC ablation, and atypical AFL ablation at the other campus. The team will stay at their respective campus until all the procedures are completed. Call shifts are covered on Saturdays and Sundays from 0900-1700 for urgent PPM implantations.
How do you ensure timely case starts and patient turnover?
One team member arrives daily at 0600 to open the lab, power on equipment, and perform the necessary quality control checks. The EP team maintains one of the quickest turnover rates in the department, working efficiently to get the patients out of the room and set up for the next procedure. The EP team works hard and is dedicated to maintaining on-time starts.

What works well in the lab for onboarding new team members? What continuing education opportunities are provided for staff members? How do staff typically maintain and renew credentials?
The EP program has a robust onboarding process. A nurse with no procedural experience can complete onboarding for the RN role in about 12 weeks, while onboarding for a scrub role with no experience typically takes about 5 to 6 months. A technologist associate pathway is available to cross-train allied health professionals into the EP lab. A pathway program was created that includes a specific orientation outline to guide staff through the onboarding process with goals and objectives for each phase of learning. Didactic classes cover core EP concepts, and preceptors provide hands-on training and instruction of daily lab tasks. The team also participates in a dedicated monthly education hour led by physicians, product representatives, and the education team.
Discuss the program’s use of PFA, including patient selection and initial experience.
According to Dr Borne, the EP program has incorporated PFA as a core component of its AF ablation strategy. PFA represents a major advancement in catheter ablation technology, utilizing nonthermal electroporation to selectively ablate myocardial tissue while minimizing collateral injury to surrounding structures such as the esophagus, phrenic nerve, and pulmonary veins. Since its integration into the program’s approach for AF ablation in Spring 2024, over 1000 ablations have been performed using PFA. It is now employed as the ablation approach for all patients undergoing AF ablation, including first-time and redo ablation procedures. The program’s experience suggests that PFA can offer a more rapid and safer alternative to traditional thermal ablation methods, enabling efficient lesion formation with a reduced risk of complications.

What are some of the dominant trends you see emerging in the practice of EP?
Dr Borne anticipates ongoing advancement in technique and technology as it pertains to catheter ablation for AF. Future developments are expected to include evolving mapping systems capable of integrating contact force and mapping data for lesion assessment, as well as catheter designs that enable focal PFA and dual-energy delivery. In addition to technological progress, continued collection of observational data and randomized clinical trials assessing optimal ablation strategies will further improve care for patients with AF.
Share a memorable case from the EP lab and how it was addressed.
According to Brad Mikaelian, MD, while positive outcomes are often emphasized, it is the challenging experiences that most effectively test a team and drive improvement. One such case occurred during a day of routine procedures when, at the end of an otherwise unremarkable case, the patient suddenly developed a pericardial effusion and tamponade. The team responded immediately to communicate, stabilize the patient, provide necessary supplies, and coordinate with staff outside the procedure room. Their efficient and coordinated response likely saved the life of the patient, who was discharged several days later and continues to do well.

What is considered historic about the EP program or hospital? Has the program or hospital recently experienced any “firsts”?
The EP program ranks in the top 5% nationwide for Watchman implantations year to date. Memorial Hospital has performed 2000 Watchman procedures and has one of the highest concomitant procedure volumes in Colorado. Dr Mikaelian was the first physician in Colorado to implant both the Watchman FLX and the 40-mm Watchman device at Memorial Hospital. The program is currently participating in the SIMPLAAFY trial, with prior participation in the OPTION and HEAL-LAA studies. The EP lab was the first in Colorado to achieve HeartCARE Center Accreditation from the American College of Cardiology. Memorial Hospital also serves as a Center of Training for Boston Scientific and has been featured multiple times on the company’s EDUCARE website, including a recent video highlighting Dr Mikaelian’s concomitant workflow and educational initiatives for national training use.
Please describe what is unique and special about the EP lab and its staff.
The EP program has had a dedicated laboratory team since 2020. Many team members have prior experience in inpatient cardiology and other areas of invasive cardiology, bringing valuable expertise in patient care. This experience benefits newer team members through enhanced onboarding, education, and direct clinical support. According to Dr Mikaelian, a defining characteristic of the EP team is its seamless ability to transition between roles within procedures and across cases. When patients or staff members require assistance, team members respond promptly, facilitating case transitions and efficient room turnover. The team shares a unified commitment to delivering the highest level of care, which is reflected in its strong culture of collaboration and teamwork.











