Opening a New Cardiac Electrophysiology Lab: Planning Strategies and Takeaways From HCA Florida University Hospital
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of EP Lab Digest or HMP Global, their employees, and affiliates.
EP LAB DIGEST. 2025;25(12):8-10.
Awais K Humayun, MD, FACC, FHRS
Director, Heart Rhythm Solutions, Davie, Florida
HCA Florida University Hospital is a community-based, 165-bed teaching hospital located on Nova Southeastern University’s campus in Davie, Florida. The hospital has provided comprehensive healthcare services to Broward County since its opening in November 2021. The hospital offers a wide range of multispecialty services, including interventional cardiology. Since its inception, the hospital’s vision has been to grow strategically and expand specialty services to meet the needs of the community. Given the increasing prevalence of heart rhythm disorders, an aging population, and higher demand for advanced cardiac care, HCA Florida University Hospital was committed to the development of an electrophysiology (EP) program for expansion of cardiac care services. There are 2 cardiac catheterization labs, with one that was dedicated to EP; both were constructed from the ground up. The labs have predominantly been utilized over the last 3 years by practicing interventional cardiologists and electrophysiologists in the community who have actively been performing procedures such as cardiac catheterizations, transesophageal echocardiography, cardioversions, cardiac device implantations, and catheter ablations. The buildout of the EP lab was undertaken with the goal of anticipated growth opportunities such as atrial fibrillation (AF) ablations and structural heart cases. The purpose of this article is to outline the key steps taken in designing HCA Florida University Hospital’s new EP lab, which opened in May 2024.
Opening a new EP lab is a major initiative that requires strategic vision, meticulous planning, and close collaboration across multiple disciplines. Development of the lab was a collaborative effort that engaged primary stakeholders early in the planning process, as well as input from local and HCA healthcare enterprise-level experts with the goal of developing an exceptional patient-centered program.
Strategic Planning
Early in the project, the hospital assembled a multidisciplinary planning committee comprised of an electrophysiologist, cardiologist, anesthesiologist, nursing leader, technologist, architect, and hospital administrator. The committee defined function, growth, and operational goals that would guide design and construction of the EP lab. Primary goals included:
- Supporting a full range of procedures including complex ablations, device implantations, and structural heart cases
- Building flexibility into the design to accommodate future growth of new technologies
- Prioritizing design and construction that made patient safety, staff workflow, and operational efficiency paramount
Design and Construction
The design phase required translating specialists’ clinical and workflow needs, safety concerns, and operational efficiency into design of the physical space. Committee objectives were to create an environment that would optimize procedural workflow, ensure sterility, enhance safety, and allow for advanced technology integration. Construction of the EP lab was completed in approximately 8 months.
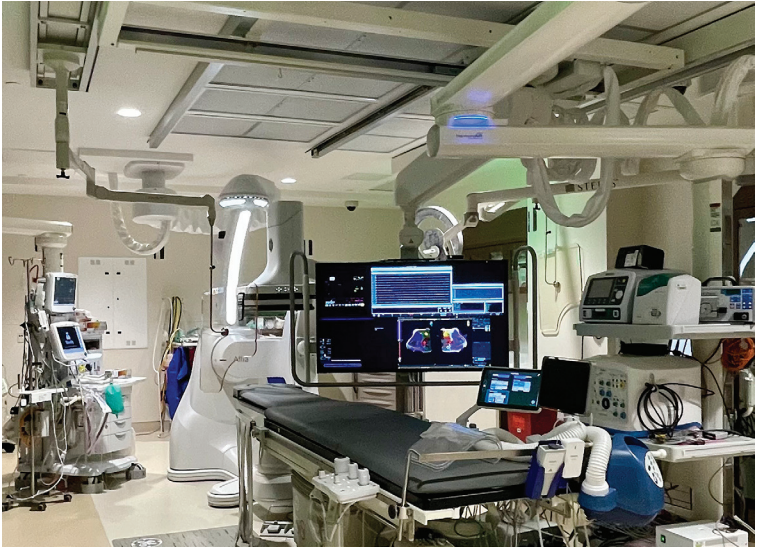
Key Design Highlights
- Room size and layout: The committee designed the 350-square-foot lab to offer ample space, allowing a full complement of equipment and personnel without crowding. Special attention was paid to the clear delineation of zones for sterile fields, anesthesia setups, and mapping systems. The design included enough storage in the procedure room for catheters and stackable arrangements for radiofrequency (RF) and pulsed field ablation (PFA) generators, as well as additional equipment such as intracardiac echocardiography (ICE) machines and cryoablation consoles.
- Control room positioning: The design included a spacious 30-square-foot control room with direct line of sight into the procedure room to ensure ease of communication and visibility during cases.
- Radiation safety: The space was fitted with lead-lined walls, strategically placed ceiling-mounted shields, and real-time Landauer radiation monitoring systems.
- Technology infrastructure: High-capacity electrical systems with redundant backup power as well as extra shielded conduit and cabling were installed to accommodate high-bandwidth needs of mapping, imaging, and recording systems. All systems were properly grounded with cables that did not cross over one another, minimizing electrical noise.
- Sterility considerations: Before entering the EP lab, specialists pass through a sub-sterile environment with a separate scrub sink. The lab was equipped with positive pressure ventilation air conditioning equipment with HEPA filters.
Equipment Selection
Significant equipment investments were influenced by product quality, vendors’ service agreements, training programs, and technical support availability.
- EP recording system: High-fidelity customizable recording systems (Prucka 3 with CardioLab Recording System [GE HealthCare] and Micropace EP) were selected to interface smoothly with mapping and imaging technologies.
- Three-dimensional (3D) mapping system: Recognizing the increasing complexity of arrhythmia ablation as well as need for open architecture, flexibility, and precision, the committee opted for EnSite X (Abbott) to provide a next-generation 3D mapping platform.
- Imaging system: The Allia fluoroscopy system (Precision 180 Radiography and Fluoroscopy System, GE HealthCare) was chosen to provide enhanced imaging and integration, and to minimize radiation exposure.
- ICE: To enhance real-time situational awareness in cardiac procedures and minimize fluoroscopy, a ViewMate Multi Ultrasound System and ViewFlex Xtra ICE Catheter (Abbott) were selected.
- Ablation systems: Both RF and PFA technologies (Ampere RF Generator and TactiFlex Ablation Catheter, Sensor Enabled [Abbott] and PulseSelect PFA System [Medtronic]) were incorporated to provide a full range of therapeutic options tailored to each patient’s clinical needs.
- Anesthesia support: Given the growing trend toward general anesthesia with complex EP procedures, the lab was equipped with full anesthesia capabilities, including ventilators, infusion pumps, and hemodynamic monitors.

Patient Flow and Operational Efficiency
Key workflow strategies included preprocedural coordination, same-day discharge pathways, procedure turnover efficiency, and continuous quality improvement (CQI).
A centralized scheduling system was developed to coordinate inpatient and outpatient procedures and minimize cancellations. Most cases have been elective outpatient cases; these are scheduled on certain days in the morning. Any add-on patients from inpatient settings are managed through the cath lab coordinator; there are no blocked slots.
Protocols were developed for eligible device implants and uncomplicated ablations to allow same-day discharge, improving patient satisfaction and reducing bed utilization. Standardized turnover protocols were instituted to minimize downtime between cases. A CQI program was initiated, reviewing key metrics such as door-to-door procedure start times, complication rates, and patient satisfaction scores. These processes were designed to maintain high procedural volumes (over 232 thus far) without sacrificing safety or quality of care.
Early Outcomes and Reflections
Since opening, the EP lab has performed a wide array of successful procedures including ablations and device implants, with complication rates below the national average (ie, 1%). Early metrics have been encouraging, with steady growth of procedural volume and positive patient satisfaction scores. The hospital intends to expand EP procedures to include AF ablations and structural heart cases in the near future. The 2026 goal is to expand to include left atrial procedures, including AF ablations and left atrial appendage cases. The hope is that the culture of continuous learning and collaboration will foster a dynamic environment that will allow the lab to evolve as new technologies, therapies, and patient needs emerge.

Challenges
The new lab was located behind the red line and within the operating room (OR) corridor. Thus, our biggest challenge was building the lab according to OR standards. Originally, we planned a sink outside one of the catheter labs to serve both labs. We lost square footage because OR standards required a dedicated sink in each room for handwashing. This requirement resulted in the EP control room losing square footage. Another challenge was achieving compatibility between different manufacturers’ equipment as well as integrating properly with the hospital’s electronic medical record. Ultimately, it came together seamlessly, but took time and creative problem-solving from our IT team.

Conclusions
The design of an EP lab is a challenging project. The task can be better navigated toward successful completion with a dedicated team and focused leadership. Sharing this planning process hopefully provides useful insights to other institutions embarking on similar projects. The opportunity to shape the future of EP through thoughtful infrastructure development is both a privilege and profound responsibility.
Disclosure: Dr Humayan has completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest, and has no disclosures to report. He reports he is credentialed with privileges at 3 HCA hospitals, including HCA Florida University Hospital, but is not an employee of any HCA hospital. He also reports participation on an advisory committee for HCA Florida University Hospital related to development and design of their cardiac electrophysiology lab. In addition, he reports that Cynthia L Boyle, PhD, BCBA-D, assisted with editing the manuscript without financial compensation and did not contribute substantially to the content beyond editorial assistance.











