Reduction in Acute Psychiatric and Emergency Department Admissions in a Long-Term Care Population Through Use of a Neurology-Based Clinical Paradigm
Abstract
The neuropsychiatric status of patients with dementia in long-term care (LTC) has remained static, despite 98% of LTC patients receiving Axis I diagnoses. To address this, a neurology-based multidisciplinary care program was implemented across 3 newly developed behavioral and psychological symptoms of dementia-focused skilled nursing facilities. Over a 12-month period, 2 US Centers for Medicare & Medicaid Services clinical key measures (acute inpatient psychiatric and emergency department [ED] admissions) were reported and analyzed. Across the 3 facilities, acute hospitalizations decreased from 1.79 to 0.76 per 1000 patient days, and ED visits decreased from 1.43 to 0.70 per 1000 patient days. Both metrics reached statistical significance (95% CI). These findings suggest that a neurology-based integrated clinical care program can improve clinical status among LTC residents with dementia. This program can potentially be installed across other LTC settings to globally improve neuropsychiatric and overall clinical status.
Citation: Ann Longterm Care. 2025. Published online September 26, 2025.
DOI:10.25270/altc.2025.11.004
The neuropsychiatric clinical status of patients with dementia and patients with other general neurological conditions in long-term care (LTC) settings has been stalled for several decades. For example, data from the US Centers for Medicaid & Medicare Services (CMS) show less than a 10% reduction in antipsychotic drug (APD) use in the past 15-year period.1 Similarly, broader efforts in typical dementia care have shown a lack of positive improvement in behavioral and neuropsychiatric symptoms of dementia.2,3
The Minimum Data Set (MDS) indicates that 98% of LTC residents with dementia have an Axis I diagnosis, and most of these residents are severely affected.4,5 However, only 6% have a prior history of serious mental illness (SMI).6,7,8 Since 2008, research has demonstrated that a primary neurological approach to behavioral and psychological symptoms of dementia (BPSD) and associated conditions can yield substantial health improvements.9 A 2023 review by Posar et al5 showed that applying this approach led to a 68% reduction in APD use within 5 months while maintaining or improving the overall clinical status of these patients. While conducting our review, we became cognizant of other measurable clinical outcomes improvements, including significant improvements in BPSD. This led us to shift our focus to measuring acute inpatient admissions and emergency department (ED) visits contained in the CMS dataset.
Beginning in 2019, a collaborative initiative was started with a major client skilled nursing facility (SNF) operator in Indiana to develop LTC Centers of Excellence for individuals with severe BPSD and/or associated neuropsychiatric conditions. These specialized buildings, serving a combined average census of 250 residents, implemented the Center of Excellence project inclusive of a “neurology-forward" interdisciplinary treatment model. This approach incorporates neurology, psychiatry, psychology, primary care, pharmacy, nursing, and social work, using the best available evidence and publication-based standards of care. In 2023, these buildings were serving residents with significant neuropsychiatric diagnoses.
Over time, we became aware that there were significant positive changes in the clinical status of this “pure” neuropsychiatric LTC population. To retrospectively quantify these improvements, we accessed published CMS datasets. We identified 2 primary clinical CMS retrospectively reported metrics, which indicated a change in resident clinical status: acute inpatient admissions and acute ED visits. Because of the retrospective nature of this analysis, we used the published CMS rates for these 2 variables, even though they represented a materially lower acuity level than the 3 buildings studied in this report. Additionally, because of the retrospective nature of this report, we could not reliably ascertain the prior utilization rates for these variables. The study period comprised 12 months, from July 1, 2023, to June 30, 2024. The interventions used in these buildings require approximately 1 year to reach full effect. The study period chosen was secondary to requiring no less than 1 year of operation in all 3 buildings.
The 7 components of our neurology-forward clinical paradigm are as follows:
- Create an interdisciplinary team led by neurology and including psychiatry, psychology, primary care, nursing, pharmacy, and social work.
- Conduct rigorous diagnostic and clinical status evaluation on all patients encompassing each clinical discipline.
- Comprehensive pharmacologic review of all prescribed medications.
- Initiation of neurologic pharmacotherapy for all primary and secondary diagnoses.
- Reassessment of psychiatric/psychological patient status after neuropharmacology achieves desired results.
- Amend or initiate psychiatric/psychological therapeutic interventions as clinically indicated.
- Frequent reassessment and therapeutic adjustment as indicated.
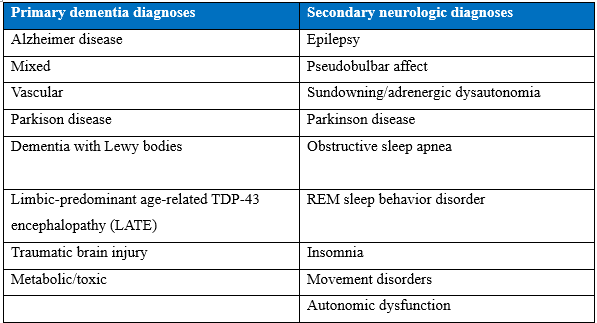
The primary and secondary diagnoses routinely encountered in these buildings are noted in the Box10,11. Neuropharmacologic interventions are specific to each of these diagnoses.
Methods
Dataset
CMS quarterly and aggregate retrospective data were collected for the review period, from the 3 Center of Excellence buildings owned by the client SNF operator. The dataset included the acute inpatient hospitalization and ED visit rates for the entire census across the 3 buildings, with an average daily sample size of 250 residents.
Key Measures
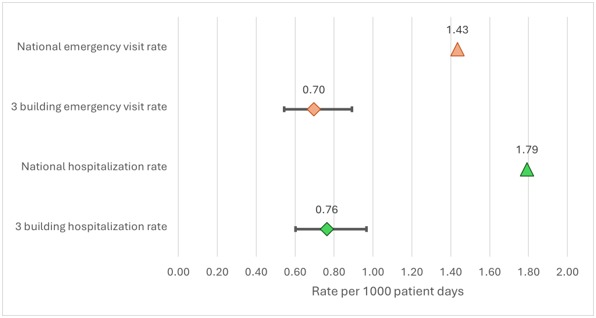
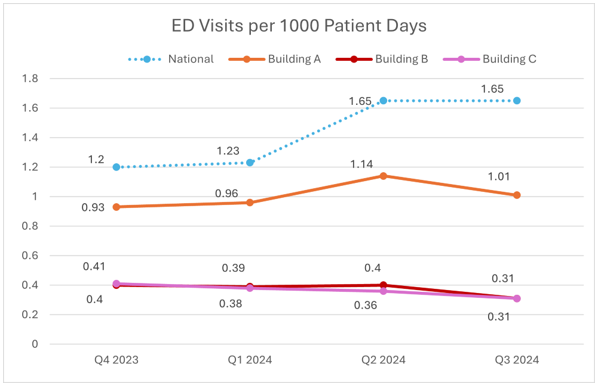
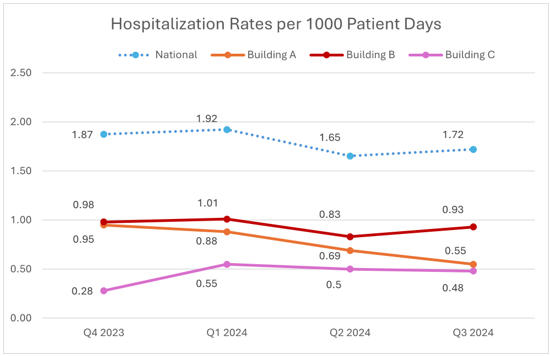
Key measures included individual and aggregate SNF building MDS census data quarterly and at 12 months; CMS published rates for acute hospitalizations and ED visits quarterly and at 12 months. These were measured as episodes per 1000 resident days (Figure 1 and Figure 2).
Analytic Plan
Using the average census data for each quarter and the reported hospitalization and ED visits per 1000 patient days, we assessed clinical significance using confidence interval (CI) analysis.
Figure 1. National ED rates compared with the 3 buildings’ ED rates
ED indicates emergency department.
Figure 2. National hospitalization rates compared with the 3 buildings’ hospitalization rates
ED indicates emergency department; Q, quarter.
Results
ED Visits
Across 90 410 patient days, we estimated 63 incidents, yielding an incidence rate of 0.70 per 1000 patient days (95% CI, 0.54-0.89). The mean national incidence rate during this time was 1.43, which is not included in the 95% CI, indicating that ED visits from patients at the 3 buildings are significantly lower than the national average (Figure 3).
Hospitalizations
Across 90 410 patient days, we estimated that 69 patients were hospitalized, yielding a hospitalization incidence rate of 0.76 per 1000 patient days (95% CI, 0.60-0.97). The CI does not include the mean national incidence rate, 1.79, indicating that the hospitalization rate at the 3 buildings is significantly lower than the national average (Figure 3).
Figure 3. Aggregate national ED and hospitalization rates compared with the 3 buildings’ ED and hospitalization rates with CIs
ED indicates emergency department; Q, quarter.
Discussion
The aging population is highly vulnerable to the incidence and prevalence of neurologic disorders, which the World Health Organization has reported as the leading cause of disability worldwide.12 By 2050, 1 in every 5 Americans will be aged 65 years or older.13 Of this population, 25% to 35% (more than 50% of those aged 85 years or older) will develop some form of neurocognitive disorder.14,15
Virtually all disabling geriatric neurological disorders have a high expectation of accompanying neuropsychiatric illness, with greater severity often correlating with greater incidence and severity of comorbid psychiatric dysfunction.16 Although pre-existing SMI accounts for a distinct minority of these cases, it can compound the severity of subsequent neuropsychiatric problems. As neurologic care advances, it is reasonable to expect concomitant improvements in “downstream” comorbid psychiatric conditions, but this hypothesis has not been heretofore tested in the LTC patient cohort. Findings from our original APD study, accompanied by the results presented in this report, strongly support the adoption of a neurology-based approach to LTC patient care. This approach appears to be highly beneficial to these patients and surrounding communities of interest.
There are material limitations to the analysis of this data set. As indicated above, CMS data do not parse out the specific nature of these hospitalizations nor ED visits. Consequently, we cannot ascribe the specific nature of use reduction based on CMS direct data. Our internal audit indicated that 55% to 70% of acute inpatient admissions and ED visits were primarily psychiatric. It is, therefore, likely that in addition to an overall reduction in acute psychiatric admissions, there is a concomitant reduction in medical admissions, representing an overall improvement in patient clinical status. The limited sample size is another constraint, and additional studies are required to further define and test the specifics of these outcomes.
CMS research has already identified that LTC residents commonly experience potentially avoidable ED and acute hospital transfers.17 These residents are especially vulnerable to the risks and negative outcomes associated with ED and hospital admissions and transitions between nursing facilities and hospitals. Research by Rosvik and Mork Rokstad18 has shown that acute hospitalization among SNF residents with dementia can be confusing and frightening for the resident and may negatively affect their physical, mental, and cognitive abilities, even when the care is medically necessary.
Hospitalization often leads to an increase in BPSD, risk of poor outcomes, and higher incidence of harm and further cognitive decline for people with dementia. According to Afonso-Argilés and colleagues,19 despite the benefits of specialized care, multiple negative health outcomes have been associated with hospitalization, especially for those with dementia, including high risk of delirium, functional decline, fall-related injuries, nosocomial infections, decubitus pressure ulcers, and increased mortality. Clinical outcomes are generally poorer for LTC residents who are transferred to the ED or hospitalized compared with those who remain in their LTC facility.
Our novel care structure offers a neurology-forward paradigm based on a robust methodology to reduce hospitalizations and ED visits in the neuropsychiatric population of LC facilities. This approach uses evidence-based care to improve the overall clinical status and quality of life for this population, thereby helping residents remain in their living environments and reducing the negative impact of hospitalization and care transfers.
Conclusion
This study has shown that implementation of a certified, novel 7-step neurology-forward clinical model for LTC residents with neurocognitive impairment materially reduces the rate of ED and hospital admissions and improves resident quality of life. The structure and methodology of this approach is designed for replicability, making it a potential viable solution across any LTC setting.
Acknowledgments
Majestic Care Corporate: Thanks and recognition for the partnership, clinical excellence, and support and oversight of the care of our mutual residents/patients.
Joshua C. Reid: Thanks and recognition for the time and effort in formatting the data and figures for this article.
Authors: Steven L Posar, MD • Robert L Russell, MD, MBA • Olaniyi O Osuntokun, MD • James B Shackson, MD • Brendan M Daley, MD • Daniel M Heiser, PsyD • Anita D Arthur, APRN
Affiliations: Eldercare Foundation
Disclosures: The authors report no relevant financial relationships.
Address correspondence to:
Steven L. Posar, MD
Eldercare Foundation
2100 North Main Street, Suite 304
Crown Point, IN 46307
References
- Long Term Care Community Coalition. A Decade of Drugging: Sedation of Nursing Home Residents with Dangerous Antipsychotic Drugs Persists Despite Federal Partnership. December 2022. Accessed July 29, 2025. https://nursinghome411.org/wp-content/uploads/2022/12/Decade-Drugging-LTCCC-122022.pdf
- Reuben DB, Gill TM, Stevens A, et al; D-Care Study. Health system, community-based, or usual dementia care for persons with dementia and caregivers: the D-CARE randomized clinical trial. JAMA. 2025;333(11):950-961. doi:10.1001/jama.2024.25056
- Sachs GA, Johnson NM, Gao S, et al. Palliative care program for community-dwelling individuals with dementia and caregivers: the IN-PEACE randomized clinical trial. JAMA. 2025;333(11):962-971. doi:10.1001/jama.2024.25845
- Phan SV, Osae S, Morgan JC, Inyang M, Fagan SC. Neuropsychiatric symptoms in dementia: considerations for pharmacotherapy in the USA. Drugs R D. 2019;19(2):93-115. doi:10.1007/s40268-019-0272-1
- Posar SL, Reid A, Heiser DM, Pinon J, Kinzie J. Antipsychotic drug reduction through the implementation of a neurologically oriented, interdisciplinary psycho-diagnostic and antipsychotic stewardship program. J Am Med Dir Assoc. 2023;24(11):1629-1631. doi:10.1016/j.jamda.2023.08.025
- National Institute of Mental Health. Statistics. Updated 2024. Accessed July 29, 2025. https://www.nimh.nih.gov/health/statistics
- Hudson C. G. (2012). Declines in mental illness over the adult years: an enduring finding or methodological artifact? Aging Mental Health, 16(6), 735-52.
- Substance Abuse and Mental Health (SAMHSA) Older Adults Living With Serious Mental Illness: The State of the Behavioral Work Force. Introduction. 2019. Accessed August 25, 2025. https://library.samhsa.gov/product/older-adults-living-serious-mental-illness-smi-state-behavioral-health-workforce/pep19
- Tible OP, Riese F, Savaskan E, von Gunten A. Best practice in the management of behavioural and psychological symptoms of dementia. Ther Adv Neurol Disord. 2017;10(8):297-309. doi:10.1177/1756285617712979
- Helvik AS, Selbæk G, Šaltytė Benth J, Røen I, Bergh S. The course of neuropsychiatric symptoms in nursing home residents from admission to 30-month follow-up. PLoS One. 2018;13(10):e0206147. doi:10.1371/journal.pone.0206147
- Akrour R, Courret-Gilgen C, Perrenoud B. Prevention and management of behavioural and psychological symptoms in patients with dementia in acute care: a best practice implementation project. JBI Evid Implement. 2022;20(4):289-300. doi:10.1097/XEB.0000000000000329
- World Health Organization. Over 1 in 3 people affected by neurological conditions—the leading cause of illness and disability worldwide. News release. March 14, 2024. Accessed July 29, 2025. https://www.who.int/news/item/14-03-2024-over-1-in-3-people-affected-by-neurological-conditions--the-leading-cause-of-illness-and-disability-worldwide
- Population Reference Bureau. Fact sheet: aging in the United States. January 9, 2024. Accessed July 29, 2025. https://www.prb.org/resources/fact-sheet-aging-in-the-united-states
- Fang M, Hu J, Weiss J, et al. Lifetime risk and projected burden of dementia. Nat Med. 2025;31(3):772-776. doi:10.1038/s41591-024-03340-9
- Solis-Moreira J. Annual U.S. dementia cases projected to rise to 1 million by 2060. Scientific American. December 19, 2024. Accessed July 29, 2025. https ://www.scientificamerican.com/article/annual-u-s-dementia-cases-projected-to-rise-to-1-million-by-2060
- Selbaek G, Engedal K, Benth JŠ, Bergh S. The course of neuropsychiatric symptoms in nursing-home patients with dementia over a 53-month follow-up period. Int Psychogeriatr. 2014;26(1):81-91. doi:10.1017/S1041610213001609
- US Centers for Medicare & Medicaid Services. Sharp reduction in avoidable hospitalizations among LTC residents. HealthCap; 2017. Accessed July 29, 2025. https://healthcapusa.com/wp-content/uploads/2017/01/Sharp-reduction-in-avoidable-hospitalizations-among-LTC-residents-002.pdf
- Rosvik J, Mork Rokstad AM. What are the needs of people with dementia in acute hospital settings, and what interventions are made to meet these needs? A systematic integrative review of the literature. BMC Health Serv Res. 2020;20(1):723. doi:10.1186/s12913-020-05618-3
- Afonso-Argilés FJ, Meyer G, Stephan A, et al; RightTimePlaceCare Consortium. Emergency department and hospital admissions among people with dementia living at home or in nursing homes: results of the European RightTimePlaceCare project on their frequency, associated factors and costs. BMC Geriatr. 2020;20(1):453. doi:10.1186/s12877-020-01835-x