An Analysis of Risk Factors for Complication Following Upper Extremity Amputation
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Abstract
Background. Upper extremity amputations (UEAs) comprise anywhere from 14% to 50% of amputations. Risk factors for lower extremity amputations (LEA), such as diabetes, have been established in the literature. The authors attempt to illuminate similar associations with UEA, which have been studied to a lesser degree. In this study, the authors explore preoperative risk factors that may predispose patients to complications after UEA.
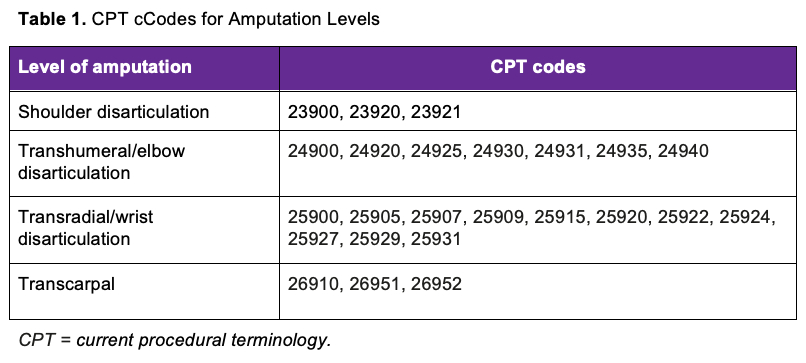
Methods. The American College of Surgeons National Surgical Quality Improvement Program Database was queried from 2006 to 2018 for patients undergoing various levels of UEA using current procedural terminology codes. Demographic and comorbidity data were collected, including level of amputation; levels included shoulder disarticulation (SD), transhumeral/elbow disarticulation, transradial/wrist disarticulation, and transcarpal. Outcomes included major systemic complications, prolonged length of stay (LOS), unplanned reoperation, surgical site infection (SSI), and death. Chi-squared and multivariate binary regression analysis were used to determine odds ratios.
Results. Overall, 3907 patients undergoing UEA were identified. Upon multivariate binary regression analysis, hyponatremia, hypoalbuminemia, history of cardiac disease, and SD were independent risk factors for major systemic complications. SD amputation was an independent risk factor for major systemic complications, shock/septic shock, and prolonged LOS. History of cardiac disease was an independent risk factor for major systemic complications, prolonged LOS, and death. Diabetes was an independent risk factor for prolonged LOS, unplanned reoperation, and SSI.
Conclusions. The study found that in patients undergoing UEA, there was an increased risk of 30-day complications in those with hyponatremia, hypoalbuminemia, cardiovascular disease, diabetes, and proximal amputations.
Introduction
The prevalence of limb loss in the United States is expected to reach 3.2 million by 2050.1 Although upper extremity amputations (UEAs) comprise a smaller portion of limb loss, it is still significant, varying anywhere from 14% to 50% of all amputations.2 UEA can greatly limit patients physically in their daily lives and is associated with mental disorders such as depression, post-traumatic stress disorder, and pathologic grief.2,3
Factors leading to UEA most frequently include trauma as well as tumors, vascular malformation, osteomyelitis, and soft tissue infections.1,4,5 Patients with diabetes are at significant risk of limb loss secondary to infectious causes.6 Diabetes-related gangrene has been established as a significant risk factor for lower extremity amputation (LEA).7,8 With the prevalence of diabetes increasing in the United States, more attention is being paid to the increasing prevalence of UEA in patients with diabetes.9 As such, there is an increased need for research into the treatment of these conditions.
There are several well-documented complications after a UEA, such as neuropathic pain and surgical site infection (SSI).5,10 Preoperative risk factors for complications include having received a blood transfusion, pulmonary circulation disorders, renal failure, and high blood pressure.11,12 Risk factors for complications relating to the injury and the treatment plan include the severity of the injury, whether a staged surgery was necessary, and the use of prostheses.11,12
The level of amputation has also been shown to contribute to the risk of complications. The most common UEA is of the hand. Amputations more proximal on the arm, such as transradial and transhumeral, occur less frequently but are associated with higher rates of secondary revision.1,5,13 This parallels LEA findings, as amputations above the knee are associated with more complications and lower overall survival rates compared with below.14 Associations with peripheral artery disease and LEA postoperative complications have been long-established; thus, we attempt to illuminate similar associations with UEA, which have been studied to a lesser degree in the current literature. In this study, we explore preoperative risk factors that may predispose patients to complications after UEA.
Materials and Methods
Study design
The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) Database was queried from 2006 to 2018 for patients undergoing various levels of UEA using current procedural terminology (CPT) codes (Table 1). The levels of amputation included shoulder disarticulation (SD), transhumeral/elbow disarticulation (TH), transradial/wrist disarticulation (TR), and transcarpal disarticulation (TC).
Collected demographic data included age, BMI, gender, race, and risk factors; risk factors included smoking history, hyponatremia (<135 mEq/L), hypoalbuminemia (<3.5 mg/dL), cardiovascular comorbidity (history of congestive heart failure [CHF], percutaneous coronary intervention, or myocardial infarction [MI]), hypertension (HTN) requiring medication, diabetes, renal failure, bleeding disorders, ventilator use, systemic sepsis, and obesity (> 30 kg/m2). Percentages were calculated based on the number of patients that had a value for the recorded variable. Since this study only used deidentified data from a national database, institutional review board approval was deemed not required as per our institutional guidelines.
Outcome measures
The outcomes evaluated included major systemic complications, prolonged length of stay (LOS), unplanned reoperation, SSI, and death. Major systemic complications were further broken down into cardiac, renal, and pulmonary complications. A prolonged LOS was defined as a postoperative hospital stay greater than the 75th percentile (2 days). The ACS-NSQIP database tracks patients through 30 days postoperatively, so only developments within this time frame were recorded.
Statistical analyses
Categorical variables were assessed via chi-square goodness-of-fit tests to determine the differences in distribution among amputation levels. All demographic and risk factor data were included in the multivariate binary regression model to calculate adjusted odds ratios (OR) of each risk factor. All ORs were reported with a 95% CI. All amputation level ORs were compared with the reference TC amputation group. All analyses were performed using SPSS v28 (IBM).
Results
Demographic and clinical characteristics
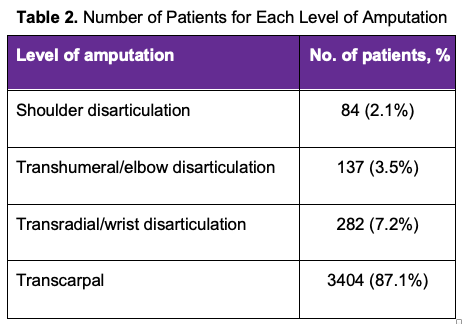
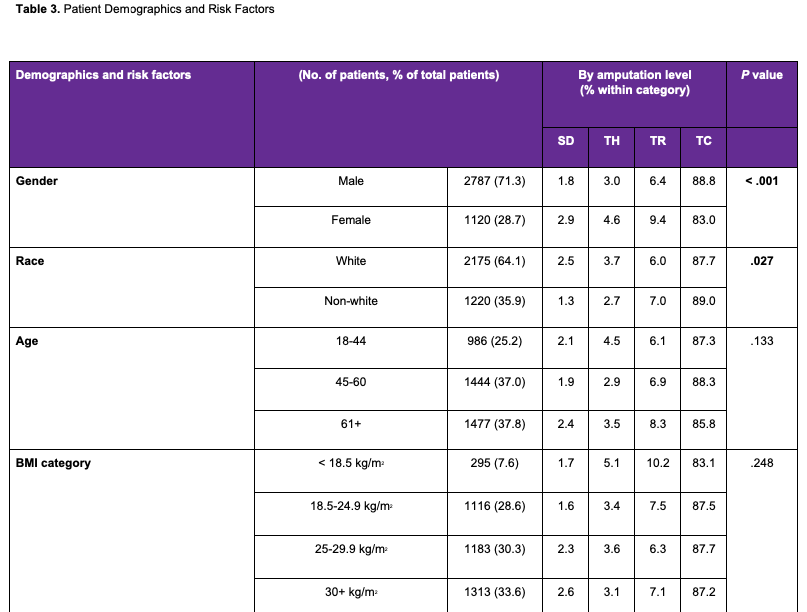
Overall, 3907 patients undergoing UEA were identified. The levels of amputation were SD, TH, TR, and TC. The number of patients for each level of amputation is displayed in Table 2, with the most common being TC, followed by TR, TH, and SD. Demographic characteristics and comorbidities are outlined in Table 3. Male, White, older (61 years or older), and obese patients were more likely to undergo a UEA. HTN requiring medication was the most common comorbidity, followed by hyponatremia, obesity, diabetes, smoking, hypoalbuminemia, bleeding disorders, systemic sepsis, history of cardiovscular disease, renal failure, and ventilator use. The distributions of these patients in the different amputation levels are also outlined in Table 3. There was a distributional difference in gender, race, and comorbidities upon bivariate chi-square analysis with amputation level. Female, White, hyponatremic, and hypoalbuminemic patients were more likely to undergo SD and TH amputations. There was no difference in the age group or BMI category.
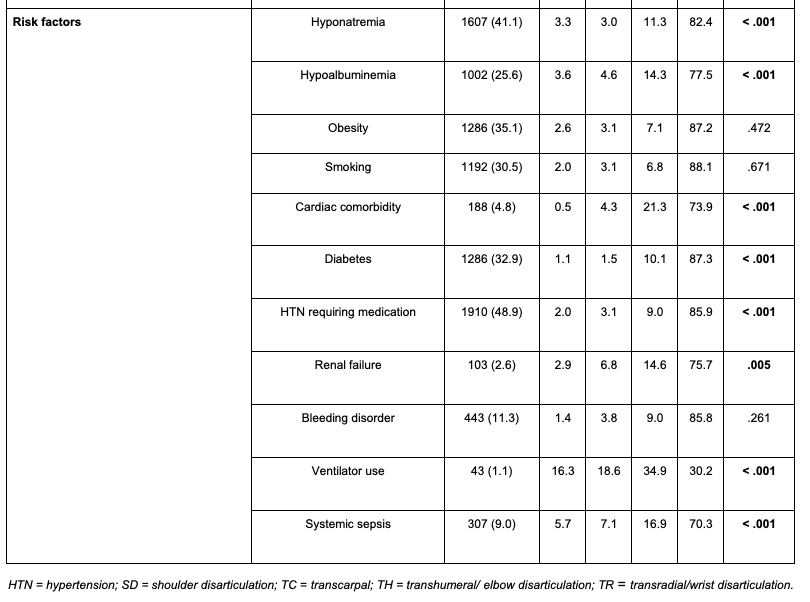
Thirty-day postoperative complications in UEA patients
Thirty-day morbidity and mortality data are displayed in Table 4. UEA patients most commonly experienced prolonged LOS, followed by major systemic complications, unplanned reoperation, SSI, and death. Within major systemic complications, septic shock/shock was the most common outcome, followed by pulmonary, cardiovascular, and renal. Upon bivariate chi-square analysis, the likelihood of mortality, major systemic complications, prolonged LOS, and unplanned reoperation increased with more proximal amputations. SSI was more likely in the TC group, but this difference was not significant.
Risk factors for 30-day complications
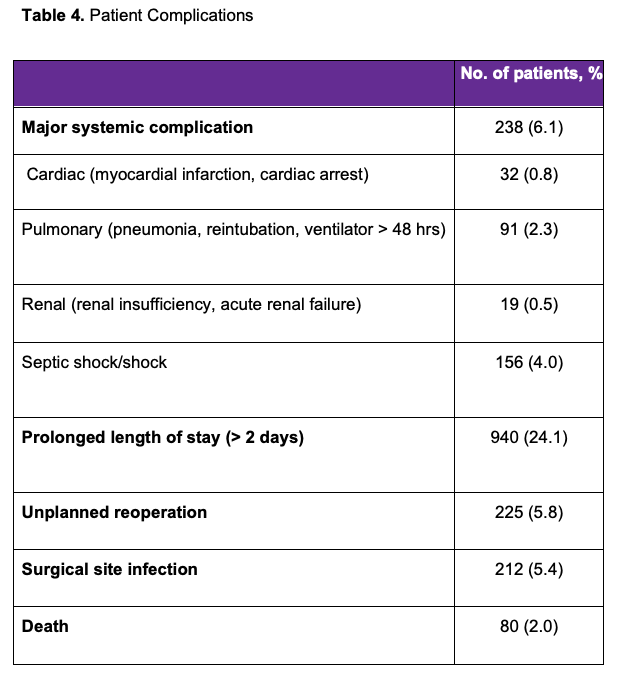
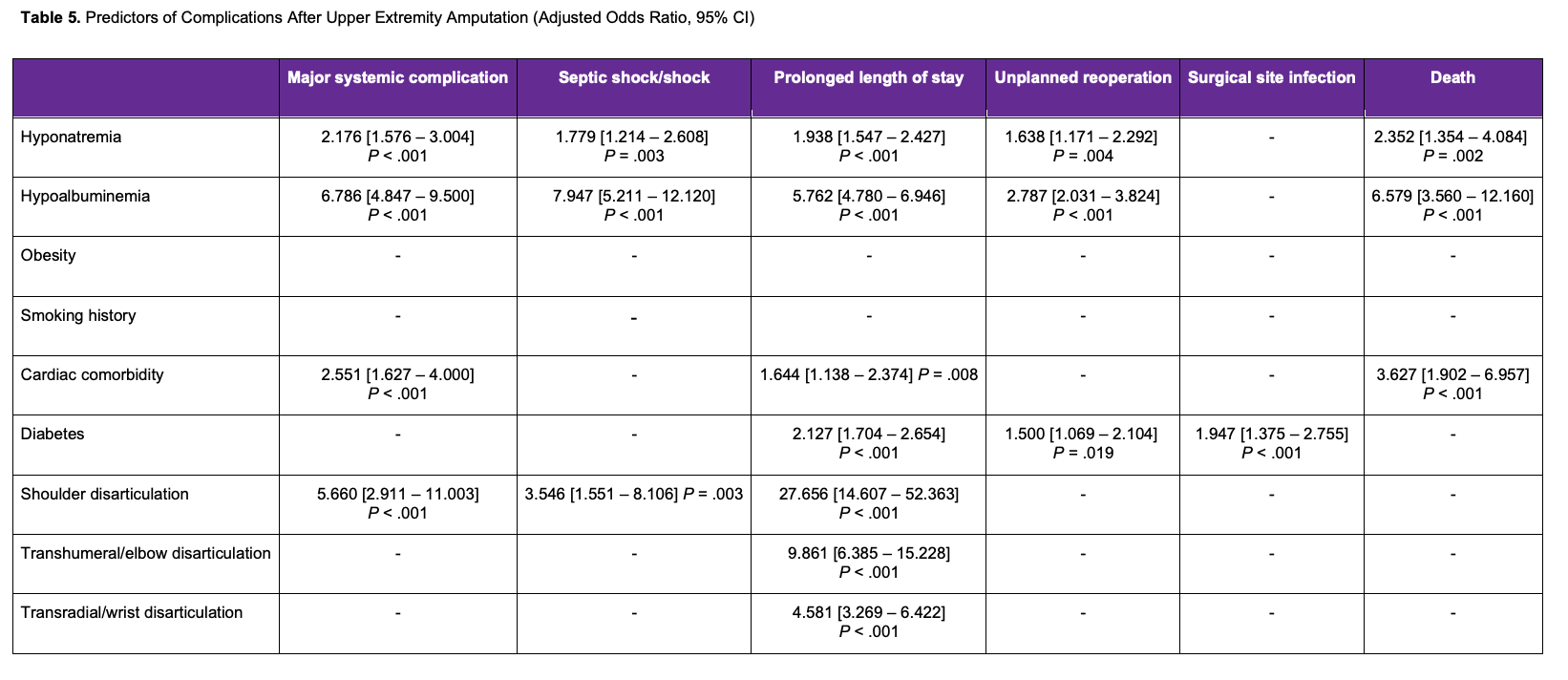
Upon multivariate binary regression analysis, hyponatremia, hypoalbuminemia, history of cardiovascular disease, and SD were independent risk factors for major systemic complications. Hyponatremia and hypoalbuminemia were independent risk factors for all recorded outcomes, except for SSI. SD amputation was an independent risk factor for major systemic complications, shock/septic shock, and prolonged LOS. History of cardiovascular disease was an independent risk factor for major systemic complications, prolonged LOS, and death. Diabetes was an independent risk factor for prolonged LOS, unplanned reoperation, and SSI. TH and TR amputations were independent risk factors for prolonged LOS. Obesity and smoking history were not associated with any recorded outcome. All adjusted ORs are listed in Table 5.
Discussion
Large database studies of this nature have previously only been conducted on LEA, perhaps because of its considerable social burden and decrease in life expectancy.6 However, in the current study, we posit that similar burdens upon a patient's well-being exist in the case of any kind of UEA. For this reason, we have conducted an analysis of risk factors for complications following UEA. Our study found that, in patients undergoing UEA, there was an increased risk of 30-day complications in those with hyponatremia, hypoalbuminemia, cardiovascular disease, diabetes, and proximal amputations.
Hyponatremia is one of the most common electrolyte imbalances and contains the most varying etiologies—it may be a syndrome of inappropriate antidiuresis, protein malnutrition, cancer, or medicine-related—often making it difficult to delineate a cause.15 For this reason, hyponatremia is a very common condition that leads to an increased risk for serious adverse outcomes and poor prognosis. It is described as a sodium level lower than 135 mEq/L, and severe hyponatremia is described as sodium levels lower than 120 mEq/L.15,16 Preoperative hyponatremia has also been shown to be a risk factor for postoperative complications across multiple procedures.17-20 Leung et al used the NSQIP database to determine whether preoperative hyponatremia was a predictor of 30-day morbidity and mortality after any major surgery; they reported that hyponatremia was associated with a significantly greater risk of 30-day mortality, especially in patients undergoing nonemergent surgery.21 While the aforementioned studies have shown an increased risk of sepsis and wound infection with preoperative hyponatremia, no study to date has been conducted in patients undergoing UEA.
Hypoalbuminemia is a frequently used surrogate marker of malnutrition. Surgical procedures in general surgery, otolaryngology, and orthopedics have shown an increased risk of complication and mortality in malnourished individuals.20,22-24 Hypoalbuminemia has a strong predictive value for morbidity and mortality in hospitalized patients, regardless of the underlying etiology.25 Low albumin has often been used as a surrogate marker for malnutrition and poor overall health. Lee et al focused on patients who underwent total shoulder arthroplasty with preoperative hypoalbuminemia, and the most notable findings were an increased risk of pulmonary complications and reoperation.26 Previous studies in orthopaedic procedures have suggested that, especially in older patients, preoperative albumin levels, as a surrogate for nutritional status, should be used to assess the likelihood of perioperative or postoperative events.27 Our findings offer further support for this notion, in that malnutrition was associated with all assessed postoperative complications (outside of infection) on multivariate-adjusted analysis.
There were a number of studies that found diabetes to be a significant comorbidity associated with adverse events following LEA, but others found no relationship of diabetes with postoperative complications.28,29
Cardiovascular disease is one of the common illnesses in the United States, especially in the older population. It has been shown to be a risk factor for complications in surgical procedures involving UEA and LEA. Cardiovascular disease has also been shown to be a predictor for adverse events following other general surgical procedures.30,31
The incidence of diabetes has been increasing in the United States for the last 20 years,32 and it estimated that diabetes could be affecting more than 13% of adults in the United States.32 Patients diagnosed with diabetes are subject to several sequelae related to their diagnosis, including complications following surgical procedures. These postoperative complications include increased risk for infection, reoperation, surgery-related death, wound-healing, MI, urinary tract infection, and renal failure.33,34 The increased risk of complications in patients with diabetes has been shown to be related to their blood-glucose levels and whether the patient is insulin-dependent.35-36
The literature regarding risk factors and predictors for complications following amputations is dominated by the lower extremity. Curran et al also used the ACS-NSQIP to investigate indicators for readmission to the hospital after LEA.37 Their sample size (n = 5732) was similar to the sample used in our analysis (n = 3907). Their analysis found that chronic nursing home residence, nonelective surgery, prior revascularization/amputation, preoperative CHF, and preoperative dialysis were predictors of readmission following LEA. They did not find any statistically significant difference of readmission with regards to proximity of amputation between transmetatarsal, below-knee, or above-knee amputation. Curran et al did not mention hyponatremia, hypoalbuminemia, or diabetes as risk factors for complications following LEA. Our search of the literature did not produce any other studies that noted hyponatremia or hypoalbuminemia as risk factors for patients undergoing UEA or LEA. Future studies on the level of UEA as it impacts outcomes are necessary. Our preliminary findings suggest that an association exists between more proximal amputations and worsened 30-day outcomes.
There were risk factors that we did not assess that were found to be contributory to postoperative complications in other studies. These include injury severity score, blood transfusion, pulmonary circulation disorders, renal failure, high blood pressure, transfer from health care facilities (inpatient hospital, emergency room, nursing home), bleeding disorders, preoperative ventilator use, preoperative sepsis, peripheral vascular disease, hypertension, renal disease, A1c levels, bypass graft occlusion, chronic nursing home residence, prior revascularization, and amputation.5,11 There were also studies in the literature that found an increased risk of adverse events in patients with obesity or a history of smoking, which our analysis did not find to be significant.38,39
Limitations
Our study has certain limitations. First, some of the risk factors assessed relate to preoperative laboratory values, but these numbers do not necessitate clinical significance in those patients. Additionally, since the study is retrospective and uses a preexisting database, there are inherent biases and confounding variables for which we cannot account. Further, data past 30 days is not recorded by the NSQIP, imposing a major limitation on assessing the long-term impact on patient outcomes. Lastly, data regarding postoperative protocols and intraoperative techniques was not available, which could have possibly influenced postoperative outcomes.
This study demonstrates an opportunity for research in UEA optimization and further investigation. Its strength is in the number of patients assessed for postoperative adverse events and from whom risk factors were identified, about which upper extremity surgeons will now be able to counsel and educate their patients.
Conclusions
This study is one of the first analyses of risk factors for complications following UAE using a national surgical database. Going forward, surgeons conducting UAEs should be aware of patients with risk factors such as hyponatremia, hypoalbuminemia, cardiovascular disease, diabetes, and proximal amputations to help reduce complications in patients who are at higher risk.
Acknowledgments
Authors: Dhruv Mendiratta, BS; Connor Fletcher, BS; Isabel Herzog, BA; Ashok Para, MD; Tej Joshi, MD; Michael M. Vosbikian, MD; Irfan H. Ahmed, MD
Affiliation: Department of Orthopaedic Surgery, Rutgers New Jersey Medical School, Newark, New Jersey
Correspondence: Dhruv Mendiratta, BS, 140 Bergen St, Newark, NJ 07103, USA. Email: dm1332@njms.rutgers.edu
Ethics: The data used was from a deidentified national database that did not require informed consent from subjects.
Disclosures: The authors disclose no relevant financial or nonfinancial interests.
References
1. Maduri P, Akhondi H. Upper limb amputation. 2023 Aug 8. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–.
2. Shue S, Wu-Fienberg Y, Chepla KJ. Psychiatric disease after isolated traumatic upper extremity amputation. J Hand Microsurg. 2021;13(2):75-80. doi:10.1055/s-0040-1701156
3. Pomares G, Coudane H, Dap F, Dautel G. Psychological effects of traumatic upper-limb amputations. Orthop Traumatol Surg Res. 2020;106(2):297-300. doi:10.1016/j.otsr.2019.12.013
4. Wyman M, Dargan D, Caddick J, Giblin V. Hand osteomyelitis in arterial calcification, diabetes mellitus and end-stage renal failure: a comparison of 210 cases over 12 years. J Hand Surg Eur Vol. 2021;46(7):768-773. doi:10.1177/1753193420981871
5. Chawla S, Sebastian A, George Hazboun R, Glasgow A, Habermann EB, Kakar S. Complications after upper extremity revision amputation and replantation. J Plast Reconstr Aesthet Surg. 2021;74(2):407-447. doi:10.1016/j.bjps.2020.08.056
6. Lin C, Liu J, Sun H. Risk factors for lower extremity amputation in patients with diabetic foot ulcers: a meta-analysis. PLoS One. 2020;15(9):e0239236. doi:10.1371/journal.pone.0239236
7. Boyko EJ, Seelig AD, Ahroni JH. Limb- and person-level risk factors for lower-limb amputation in the prospective Seattle Diabetic Foot Study. Diabetes Care. 2018;41(4):891-898. doi:10.2337/dc17-2210
8. Rosien L, van Dijk PR, Oskam J, et al. Lower extremity amputation rates in people with diabetes mellitus: a retrospective population based cohort study in Zwolle region, the Netherlands. Eur J Vasc Endovasc Surg. 2023;66(2):229-236. doi:10.1016/j.ejvs.2023.05.030
9. Ting YJ, Tan AS, Lai CT, Satku M. Clinical factors and mortality rates for non-traumatic upper extremity amputations. J Hand Surg Eur Vol. 2022;47(3):314-320. doi:10.1177/17531934211042720
10. Lans J, Hoftiezer Y, Lozano-Calderon SA, Heng M, Valerio IL, Eberlin KR. Risk factors for neuropathic pain following major upper extremity amputation. J Reconstr Microsurg. 2021;37(5):413-420. doi:10.1055/s-0040-1718547
11. Saito T, Uehara T, Nakahara R, Shimamura Y, Nakao A, Ozaki T. Risk factors for infection following operative treatment of traumatic upper extremity amputation injury. J Hand Surg Asian Pac Vol. 2022;27(4):691-697. doi:10.1142/S2424835522500709
12. Diaz Balzani L, Ciuffreda M, Vadalà G, Di Pino G, Papalia R, Denaro V. Osseointegration for lower and upper-limb amputation a systematic review of clinical outcomes and complications. J Biol Regul Homeost Agents. 2020;34(4 Suppl. 3):315-326. Congress of the Italian Orthopaedic Research Society.
13. Adapa N, Adkins ZB, Hidden KA, Goyal KS. Risk factors for secondary revision after finger amputations. Hand (N Y). 2024;19(8):1321-1329. doi:10.1177/15589447231174480
14. Vuorlaakso M, Kiiski J, Salonen T, Karppelin M, Helminen M, Kaartinen I. Major amputation profoundly increases mortality in patients with diabetic foot infection. Front Surg. 2021;8:655902. doi:10.3389/fsurg.2021.655902
15. Seay NW, Lehrich RW, Greenberg A. Diagnosis and management of disorders of body tonicity-hyponatremia and hypernatremia: core curriculum 2020. Am J Kidney Dis. 2020;75(2):272-286. doi:10.1053/j.ajkd.2019.07.014
16. Sterns RH. Treatment of severe hyponatremia. Clin J Am Soc Nephrol. 2018;13(4):641-649. doi:10.2215/CJN.10440917
17. Liu XY, Zhang B, Kang B, et al. Does hyponatremia affect the short-term outcomes of colorectal cancer surgery: a propensity score matching analysis. Dis Markers. 2022;2022:5109999. doi:10.1155/2022/5109999
18. Holleran TJ, Napolitano MA, Duggan JP, et al. Predictors of 30-day pulmonary complications after video-assisted thoracoscopic surgery lobectomy. Thorac Cardiovasc Surg. 2023;71(4):327-335. doi:10.1055/s-0042-1748025
19. Malik AT, Quatman CE, Phieffer LS, Ly TV, Khan SN. Clostridium difficile colitis in patients undergoing surgery for hip fractures: an analysis of 17,474 patients. Hip Int. 2020;30(1):22-32. doi:10.1177/1120700019831950
20. Bindels BJJ, Thio QCBS, Raskin KA, Ferrone ML, Lozano Calderón SA, Schwab JH. Thirty-day postoperative complications after surgery for metastatic long bone disease are associated with higher mortality at 1 year. Clin Orthop Relat Res. 2020;478(2):306-318. doi:10.1097/CORR.0000000000001036
21. Leung AA, McAlister FA, Rogers SO Jr, Pazo V, Wright A, Bates DW. Preoperative hyponatremia and perioperative complications. Arch Intern Med. 2012;172(19):1474-1481. doi:10.1001/archinternmed.2012.3992
22. Hennessey DB, Burke JP, Ni-Dhonochu T, Shields C, Winter DC, Mealy K. Preoperative hypoalbuminemia is an independent risk factor for the development of surgical site infection following gastrointestinal surgery: a multi-institutional study. Ann Surg. 2010;252(2):325-329. doi:10.1097/SLA.0b013e3181e9819a
23. Tanos P, Ablett AD, Carter B, et al. SHARP risk score: a predictor of poor outcomes in adults admitted for emergency general surgery: a prospective cohort study. Asian J Surg. 2023;46(7):2668-2674. doi:10.1016/j.asjsur.2022.10.049
24. Lahes S, Fischer C, Spiliotis AE, et al. Effect of immunosuppressive medication on postoperative complications following abdominal surgery in Crohn's disease patients. Int J Colorectal Dis. 2022;37(12):2535-2542. doi:10.1007/s00384-022-04287-4
25. Gatta A, Verardo A, Bolognesi M. Hypoalbuminemia. Intern Emerg Med. 2012;7 Suppl 3:S193-S199. doi:10.1007/s11739-012-0802-0
26. Lee D, Lee R, Cross MT, Tran A, Kappa J, Moghtaderi S. Low serum albumin levels are associated with increased 30-day cardiopulmonary complications, reoperation, and readmission rates following total shoulder arthroplasty. Iowa Orthop J. 2019;39(2):27-34.
27. Tan Y, Jiang L, Liu H, Pan Z, Wang H, Chen L. The effect of preoperative hypoalbuminemia on complications after primary hip arthroplasty. J Orthop Surg Res. 2021;16(1):562. doi:10.1186/s13018-021-02702-0
28. Ries Z, Rungprai C, Harpole B, et al. Incidence, risk factors, and causes for thirty-day unplanned readmissions following primary lower-extremity amputation in patients with diabetes. J Bone Joint Surg Am. 2015;97(21):1774-1780. doi:10.2106/JBJS.O.00449
29. Phair J, DeCarlo C, Scher L, et al. Risk factors for unplanned readmission and stump complications after major lower extremity amputation. J Vasc Surg. 2018;67(3):848-856. doi:10.1016/j.jvs.2017.08.061
30. Ahmad W, Fernandez L, Bell J, et al. Assessment of postoperative outcomes of spine fusion patients with history of cardiac disease. J Am Acad Orthop Surg. 2022;30(8):e683-e689. doi:10.5435/JAAOS-D-21-00850
31. Fu H, Zheng J, Lai J, Xia VW, He K, Du D. Risk factors of serious postoperative outcomes in patients aged ≥90 years undergoing surgical intervention. Heliyon. 2023;9(2):e13117. doi:10.1016/j.heliyon.2023.e13117
32. McAlexander TP, Jagai JS, McClure LA. Latent growth trajectories of county-level diabetes prevalence in the United States, 2004-2017, and associations with overall environmental quality. Environ Epidemiol. 2022;6(4):e218. doi:10.1097/EE9.0000000000000218
33. Wintermeyer E, Ihle C, Ehnert S, et al. Assessment of the influence of diabetes mellitus and malnutrition on the postoperative complication rate and quality of life of patients in a clinic focused on trauma surgery. Z Orthop Unfall. 2019;157(2):173-182. doi:10.1055/a-0654-5504
34. Luo M, Cao Q, Wang D, et al. The impact of diabetes on postoperative outcomes following spine surgery: a meta-analysis of 40 cohort studies with 2.9 million participants. Int J Surg. 2022;104:106789. doi:10.1016/j.ijsu.2022.106789
35. Lee D, Lee R, Gowda NB, et al. Impact of diabetes mellitus on surgical complications in patients undergoing revision total knee arthroplasty: insulin dependence makes a difference. J Clin Orthop Trauma. 2020;11(1):140-146. doi:10.1016/j.jcot.2019.07.009
36. Chen JY, Nassereldine H, Cook SB, Thornblade LW, Dellinger EP, Flum DR. Paradoxical association of hyperglycemia and surgical complications among patients with and without diabetes. JAMA Surg. 2022;157(9):765-770. doi:10.1001/jamasurg.2021.5561
37. Curran T, Zhang JQ, Lo RC, et al. Risk factors and indications for readmission after lower extremity amputation in the American College of Surgeons National Surgical Quality Improvement Program. J Vasc Surg. 2014;60(5):1315-1324. doi:10.1016/j.jvs.2014.05.050
38. Chahrour MA, Habib JR, El Moheb MN, et al. Incidence and predictors of surgical site infection complications in diabetic patients undergoing lower limb amputation. Ann Vasc Surg. 2022;81:343-350. doi:10.1016/j.avsg.2021.09.040
39. Ciufo DJ, Thirukumaran CP, Marchese R, Oh I. Risk factors for reoperation, readmission, and early complications after below knee amputation. Injury. 2019;50(2):462-466. doi:10.1016/j.injury.2018.10.031