A Multicenter Hybrid Platform Trial Evaluating Amniotic Tissue Grafts in Chronic Wounds: A Real-World Evidence Protocol for Diabetic Foot and Venous Leg Ulcers
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Wounds or HMP Global, their employees, and affiliates.
Abstract
Background. Traditional randomized controlled trials of efficacy often lack generalizability due to strict inclusion criteria and controlled environments. Real-world evidence trials offer a complementary approach by evaluating the effectiveness of interventions in routine clinical practice. Objective. To prospectively assess the effectiveness of trilayer and single-layer amniotic tissue grafts in treating diabetic foot ulcers (DFUs) and venous leg ulcers (VLUs) using a hybrid platform design compared with historical controls. Methods. This multicenter, umbrella design study includes 2 parallel prospective cohorts (DFU and VLU) with 2 intervention arms each, and a shared retrospective standard of care (SOC) control group. Subjects will be randomized to receive either intervention product 1 or intervention product 2 in addition to SOC. Retrospective controls will be selected from the US Wound Registry using coarsened exact matching, comparing the primary end point of complete wound closure at 12 weeks and the secondary end point of wound area reduction. Change in quality of life as assessed using a patient-reported outcome measure and pain scores will be evaluated in the subjects in the prospective arm. Conclusion. This protocol outlines a pragmatic, patient-centered approach to evaluating advanced wound care therapies in real-world settings.
Clinical trials are essential in determining the safety and effectiveness of new medical interventions. Historically, clinical trials have followed a linear progression: Phase 1 trials focus on safety, phase 2 on efficacy, and phase 3 on comparative effectiveness.1 Such designs, often randomized controlled trials (RCTs), have set the standard in clinical research for the evaluation of treatment efficacy. However, the limitations of traditional prospective study designs—including compressed timelines, high costs, and strict eligibility criteria—pose significant challenges, especially in the context of wound management.2 Payer coverage policies, when developed based on these restrictive trials, often do not reflect the clinical realities of real-world patients. Such trials, which are typically conducted in tightly controlled environments with narrowly defined protocols, may overlook the heterogeneity and complexity of patients encountered in everyday wound care practice. As a result, rigid study designs are increasingly being questioned in favor of more adaptive, pragmatic, and patient-centered approaches that better inform clinical decision-making and policy development.3
Although the US Food and Drug Administration has not yet approved a wound care product based entirely on real-world data (RWD), its issuance of formal guidance on the use of real-world evidence (RWE) to support regulatory decision-making for medical devices—including those relevant to wound care—indicates a growing openness to this approach.4 This shift in regulatory perspective has been accelerated by increasing interest in personalized medicine and novel therapeutic modalities, particularly in the field of wound care. Thus, RWE trials are essential to contemporary wound management, because they provide insights that traditional RCTs may not fully capture and play a critical role in informing both payer coverage policy and the delivery of effective, patient-centered care.
RWE trials typically involve a more extensive and diverse patient population than RCTs, accurately reflecting real-world demographics. This inclusivity ensures that findings are applicable to various groups, including populations that are often underrepresented in clinical trials, thereby enhancing the relevance of the results to everyday clinical practice and helping clinicians determine which interventions are most effective for specific patient populations.5
Furthermore, RWE provides valuable context regarding the efficacy of treatments, considering factors such as comorbidities, concurrent medications, and socioeconomic status. This understanding facilitates the development of more personalized treatment strategies given that RWE trials frequently incorporate patient-reported outcomes (PROs), which shed light on patients’ experiences, preferences, and overall quality of life.6 This patient-centric approach is vital for the formulation of more effective and satisfactory treatment plans. The integration of PROs and the inclusion of patients in the trial design process are gaining prominence. The 13 WOUND-Q scales are summarized in 4 domains or PRO measures that can be used to measure outcomes important to people with nonhealing chronic wounds.7
Herein, the authors detail the rationale and design of an innovative multicenter hybrid platform trial design to gather RWE on the effects of a prospective cohort treated with a trilayer amnion graft or a single-layer amnion graft for comparison with a coarsened exact-matched (CEM) retrospective control cohort of patients receiving standard of care (SOC) therapies only with hard-to-heal diabetic foot ulcers (DFUs) and venous leg ulcers (VLUs).
Methods
Study rationale
To collect prospective RWE related to DFUs and VLUs, this study seeks to deepen the understanding of how various treatment approaches perform in everyday clinical settings. By engaging with a more diverse patient population than what is typically targeted with traditional clinical trials, this study will gather invaluable insights. These comprehensive data are essential for assessing the effectiveness of cutting-edge wound care strategies and allowing observation of their effect in practical, real-life situations. Such a robust understanding will ultimately contribute to improving patient outcomes and advancing the field of wound care. Thus, the authors of this article developed an innovative trial design using a hybrid platform to compare the effects of treating a prospective cohort with either a trilayer amnion graft or a single-layer amnion graft to a CEM retrospective control cohort of patients with hard-to-heal DFUs and VLUs.
Study design
This multicenter study uses an umbrella design in which 2 studies will be run simultaneously: 1 involving DFUs and the other involving VLUs. Each study will have 2 prospective intervention product (IP) groups (IP1 and IP2) and 1 common SOC group as the comparator. After signing the informed consent form and successfully meeting all eligibility criteria, each patient will be randomized to 1 of the IP groups plus SOC.
Subjects for the prospective groups will be carefully chosen from those available within each investigator’s clinical practice. This selection process will involve a thorough application of the specific study inclusion and exclusion criteria tailored to either the DFU trial or the VLU trial. Each candidate will be evaluated to ensure they meet the necessary health profiles and conditions required for participation in these studies. Institutional Review Board (IRB) approval has been obtained for this study from Advarra. All prospective participants will undergo an informed consent process in accordance with the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use Good Clinical Practice guidelines to ensure ethical standards and participant protection throughout the study.
The control group will be retrospectively selected from deidentified data sourced from the US Wound Registry (USWR) by applying the established inclusion and exclusion criteria for either the DFU or the VLU trial. The aggregated, deidentified clinical data from this specialized repository will be matched to intervention subjects within each study using a CEM approach. Key variables such as age, sex, comorbid conditions, baseline wound area, tissue type exposed, total number of concomitant wounds, and baseline wound age will be used for matching purposes. Further details will be outlined in the statistical analysis plan (SAP). The target retrospective control subject pool is expected to be 3 times larger than the prospective treatment group, with a goal of a minimum of 165 subjects for each study.
Study population
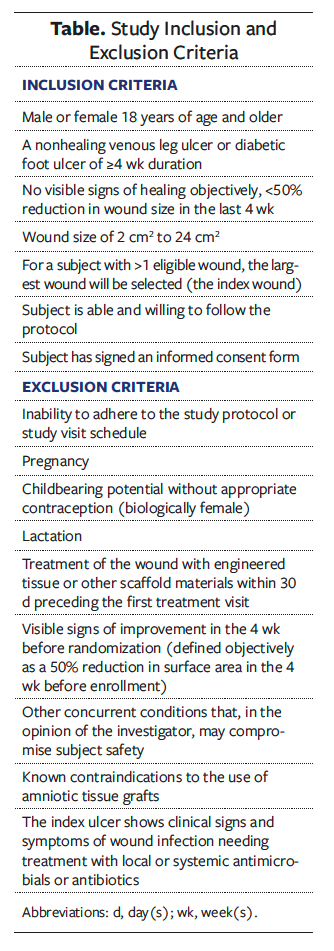
All study subjects will meet the following criteria: adults aged 18 years and older with a hard-to-heal DFU or VLU of at least 4 weeks’ duration, with a wound size between 2 cm² and 24 cm². All wounds must be nonhealing and exhibit less than 50% reduction in wound size in the past 4 weeks using traditional wound care therapies (Table). Exclusion criteria are listed in the Table.
The study population will be drawn from among individuals receiving treatment for DFUs or VLUs. These subjects are expected to represent the general US population, regional differences notwithstanding. Investigators with wound care expertise will select patients with either DFUs or VLUs for inclusion in the study.
The diagnosis of subjects presenting with DFUs or VLUs will be determined through a comprehensive clinical assessment conducted by the investigators. This assessment will encompass a thorough patient evaluation, incorporating relevant diagnostic testing as deemed appropriate per the site standard operating procedures in order to capture real-world clinical practice.
This study uses broad inclusion criteria to reflect real-world patient populations and enhance generalizability. To preserve clinical flexibility and mirror routine practice, no specific vascular assessments, off-loading devices, compression therapy, or secondary dressings will be mandated. Instead, all relevant treatment modalities and assessments will be documented through detailed case report forms. These data will be used for post hoc analyses to identify patterns and trends that may inform future research and clinical decision-making.
Interventions
The IP1 group will receive trilayer amnion graft (Tri-Membrane Wrap; BioLab Holdings, Inc) in addition to SOC. The IP2 group will receive single-layer amnion graft (Membrane Wrap-Lite; BioLab Holdings, Inc) in addition to SOC. SOC includes debridement, moisture-balanced dressings, and compression (VLUs) or off-loading (DFUs).
Control group
This study uses data from the USWR to retrospectively establish a cohort of subjects who have received SOC, which will serve as a reference for comparing outcomes in the prospective arms of the clinical trial. The primary objective is to use contemporary patient data to create a robust control group that allows for meaningful comparative analysis with the intervention group subsequent to matching.
Eligibility criteria for data mining include adults (aged 18 years and older) who have been diagnosed with wounds similar to those in the target population of the trial. These patients must have received only SOC without any cellular and/or tissue-based product (CTP) treatment or other advanced therapeutic (eg, hyperbaric oxygen therapy, negative pressure wound therapy). Only control subjects with a sufficient number of clinical encounters and documented outcomes will be used for matching purposes.
The USWR collects patient information through a secure electronic health record (EHR) system (Intellicure, LLC). The study protocol received approval from The Woodlands IRB (Advarra), which determined that the secondary analysis of deidentified data qualifies as exempt research. This exemption is consistent with Title 45 of the Code of Federal Regulations, Part 46, which states that human subjects are exempt from informed consent requirements when their involvement is strictly limited to retrospective data analysis, their subsequent care is unaffected, and their identities are protected.
The USWR aggregates clinical data through secure electronic transmission and is used by over 1000 health care practitioners across 29 states.8 The EHR contains point-of-care reminders for SOC interventions based on clinical practice guidelines, such as compression for VLUs, off-loading for DFUs, and arterial assessments, all of which are recognized as quality measures by the Centers for Medicare & Medicaid Services (CMS), as outlined in the quality measures provided by the USWR and the US Podiatry Registry.9
Furthermore, the USWR is recognized by the CMS as a Qualified Clinical Data Registry (QCDR). The purpose of the QCDR is to collect data generated during routine clinical care to evaluate patient outcomes, safety, treatment effectiveness, and overall quality of care for patients with chronic wounds and ulcers. Data are aggregated nationally while ensuring compliance with Health Insurance Portability and Accountability Act regulations and IRB policies.
In the United States, diagnosis coding is standardized through the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM).10 Although this coding system includes codes for diabetes and venous insufficiency specifically related to ulcers, it does not provide specific codes for DFUs or VLUs. The EHR assists practitioners by guiding them through the use of appropriate clinical terms, mapping each ulceration to the most clinically relevant ICD-10-CM code combinations. DFUs are identified through the combination of diabetes-related codes (eg, E10.621, E11.621, or E13.621) with relevant non-pressure ulcer codes (eg, L97.4 or L97.5). VLUs are designated using venous insufficiency codes (eg, I83, I87.2, or I87.3) alongside the appropriate L97 codes to convey ulcer location and depth.
CEM
CEM is an exact matching process and will use subjects in the deidentified dataset to match the intervention groups based on categories or “bins” of the 4 variables for both the DFU and VLU cohorts independently. The bin values will be described in the SAP. Individuals in the treatment and control groups will then be paired based on their shared bin values. If 2 individuals have the same bin values for all the coarsened variables, then they are considered a match. If any of the subjects in the intervention groups cannot be matched, then unmatched individuals are dropped, and the remaining observations are reweighted to account for the lost data. Further details will be available in the SAP. Following the matching process, the investigators will assess the balance between the intervention and SOC arms using standardized mean differences and visual inspection of covariate distributions (eg, quantile-quantile plots), both for the 4 matched variables and for other selected variables.
Outcomes
Primary and secondary outcomes will be established in alignment with the primary clinical trial protocol. These outcomes will be assessed within the CEM SOC arm to evaluate the relative efficacy of the intervention in comparison to SOC practices. The primary end point is defined as the proportion of wounds that achieve complete wound closure (CWC) by 12 weeks. The secondary end points are the percentage area reduction (PAR), measured at 4 weeks, 8 weeks, and 12 weeks, and time to CWC. It is noteworthy that the WOUND-Q metric is not traditionally collected in standard clinical care and that pain scores are documented infrequently; consequently, these metrics cannot be matched to control subjects. In the prospective arm of the study, WOUND-Q and pain scores will be collected and assessed with each participant serving as their own control. The exploratory outcomes of this study will encompass the frequency of clinic visits as well as the comparative analysis of the number of CTP applications between subjects who successfully obtain CWC and those who do not.
Sample size
Fifty-five subjects per group (DFU, VLU, SOC) will be enrolled, for a total of 165 subjects. The study is powered to detect a 30% difference in healing rates (80% power at an α level of .05).
Randomization
Randomization will be performed at a 1:1 allocation to IP1 or IP2 using block randomization.
Statistical analysis
Data will be analyzed using intention-
to-treat (ITT) principles. Comparisons between groups will utilize appropriate statistical tests. Adjustments for multiple comparisons will be made as necessary. Descriptive statistical methods will be used to summarize the data from this study, with hypothesis testing performed for the primary and other selected efficacy end points. All testing for end points will be 2-sided, with α set at .05 as the level of significance. The ITT analysis will be conducted via the Fisher exact test for the primary end point. Linear mixed models will be used to determine PAR. Multiplicity of statistical testing of secondary end points will be handled with hierarchical testing.
The primary end point analysis will be performed at 12 weeks, and a series of secondary and exploratory/tertiary end points will be analyzed at the same time point. The SAP will provide a more technical and detailed description of the proposed data analysis methods and procedures. Any deviation from the analyses outlined in the protocol will be described in the most current version of the SAP. All statistical analyses and matching processes will be conducted using programs described in the SAP.
Descriptive statistics (mean, standard deviation, median, and range) will be calculated for the exploratory end points of number of visits and number of CTP applications over the 12-week study period. No formal hypothesis testing adjustments will be applied, because these end points are exploratory in nature.
Sample size estimates are based on having a common control group for each of the separate trials (DFU, VLU). This parallel, 3-group design (1 common control group and 2 treatment groups) will be used to test whether the proportion for each treatment group is different from the control group proportion (H0: Pi = Pc versus H1: Pi ≠ Pc). The hypotheses will be evaluated using 2 2-sided, 2-sample, unadjusted (Bonferroni divisor = 1) Fisher exact tests, with an overall (experiment-
wise) type I error rate (α) of .05. The control group proportion is assumed to be 0.3. To detect the treatment proportions 0.6 and 0.6 with at least 80% power for each test, the (equal) group sample size needed for each of the 3 groups (control and treatments) will be 49 (totaling 147 subjects). These numbers are rounded up to 55 in each group to account for an up to 10% dropout rate in each group.
Ethical considerations
The use of deidentified data for this analysis will adhere to all ethical guidelines related to patient privacy and data security. Participation in the trial does not mandate patient consent for the use of deidentified data, as per the institutional policies, but efforts will be made to ensure transparency regarding the use of such data in published findings.
The findings from the CEM analysis will be reported in accordance with Consolidated Standards of Reporting Trials guidelines, highlighting the methodology of data mining, matching techniques, and the resultant effect on study outcomes.11 In summary, this approach will ensure that the SOC arm is rigorously constructed, allowing for valid comparisons against the intervention arm within the clinical trial framework.
Safety monitoring
All observed adverse effects and abnormal test findings—regardless of treatment group, suspected causal relationship to the investigational device or, if applicable, other study treatment or diagnostic product or products—will be recorded.
Discussion
The incidence of hard-to-heal wounds is alarmingly high, affecting approximately 16% of Medicare beneficiaries according to a 2019 analysis.12 Although there is an escalating need for effective treatments, clinical studies assessing wound care therapies have significant design flaws. Many of these studies include patients who do not adequately represent the diversity of the populations seen in clinical practices, in turn limiting the translation of these results in real-world scenarios.13
In contrast, the trial protocol presented herein represents a modern approach to wound care research, balancing methodological rigor with real-world applicability. The strength of this study stems from its examination of a medically complex patient population, many of whom present with intricate wounds, polypharmacy, and significant comorbidities. The hybrid design allows for efficient data collection while maintaining relevance to clinical practice. The inclusion of PROs and diverse populations enhances the study’s translational value. Engaging patients in the design process allows researchers to align trial objectives with patient needs, thereby improving recruitment and retention rates. Additionally, comprehending the patient experience through PROs can provide significant insights into treatment effectiveness and overall quality of life.
As the field of clinical research continues to advance, it is imperative to design clinical trials that maintain both rigor and flexibility. Innovations in the capture of RWD, along with an increasing emphasis on patient perspectives and the integration of technology, are driving the evolution of more efficient and pertinent clinical research methodologies. By adapting to these changes, researchers can accelerate the development of effective treatments, thereby enhancing patient outcomes.
The reporting of trial data will conform to the recommendations established by the Strengthening the Reporting of Observational Studies in Epidemiology initiative.14 These guidelines provide critical direction on the necessary components for producing an accurate and comprehensive report of an observational study, thereby ensuring the integrity and reliability of the findings presented.14
Furthermore, by utilizing data from EHRs, registries, and other real-world sources, RWE can significantly expedite the research and development of new therapies by providing rapid insights into treatment performance. By mining SOC data from the USWR, the proposed study will minimize the likelihood of selection bias by acquiring research-ready data directly at the point of care through a dedicated EHR system.15
Trial protocols that use RWE, such as the one described herein, are crucial for bridging the gap between clinical research and clinical practice. The translation and implementation of wound care therapies in patient populations commonly encountered in clinical practice is essential to developing care plans that are informed by robust evidence of treatment efficacy and safety within the heterogeneous and evolving conditions of real-world wound management.
Conclusion
This multicenter hybrid platform trial design represents a significant advancement in the evaluation of chronic wound therapies by integrating RWE with rigorous clinical methodology. By leveraging CEM and retrospective controls from the USWR, the study design ensures both scientific validity and practical relevance. The inclusion of diverse patient populations and PROs enhances the generalizability and patient-centeredness of the prospective findings. Ultimately, this protocol aims to generate actionable insights into the effectiveness of trilayer and single-layer amniotic tissue grafts for DFUs and VLUs, thereby informing clinical decision-making and improving outcomes in routine wound care practice.
Author and Public Information
Authors: Windy Cole, DPM1; Marissa Carter, PhD2; Caroline Fife, MD3; and Marissa Docter, MD, BSN, RN4
Affiliations: 1Kent State University College of Podiatric Medicine, Independence, OH, USA; 2Strategic Solutions, Inc, Bozeman, MT, USA; 3Intellicure, LLC, The Woodlands, TX, USA; 4Capsicure, LLC, Hazelwood, MO, USA
Disclosure: The authors disclose no financial or other conflicts of interest.
Ethical Approval: This clinical trial protocol was developed in accordance with the ethical principles outlined in the Declaration of Helsinki and International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use Good Clinical Practice guidelines, and it received Institutional Review Board approval from Advarra. All participants (or their legally authorized representatives) will provide written informed consent before enrollment.
Correspondence: Windy Cole, DPM; Director of Wound Care Research, Kent State University, College of Podiatric Medicine, 6000 Rockside Woods Blvd, Independence, OH 44131; Wcole4@kent.edu
Manuscript Accepted: October 17, 2025
References
1. Torres-Saavedra PA, Winter KA. An overview of phase 2 clinical trial designs. Int J Radiat Oncol Biol Phys. 2022;112(1):22-29. doi:10.1016/j.ijrobp.2021.07.1700
2. Venkatraman P, Anand S, Dean C, Nettleton R. Clinical trials in wound care I: the advantages and limitations of different clinical trial designs. J Wound Care. 2002;11(3):91-94. doi:10.12968/jowc.2002.11.3.26380
3. Maw AM, Hoppe JA, Wagner NM, Mitchell J, Bean M, Trinkley KE. Pragmatic integration of user-centered design and implementation science: a new methodological approach for clinical decision support implementation in EHRs. Appl Clin Inform. 2025;16(5):1531-1540. doi:10.1055/a-2716-4479
4. U.S. Food and Drug Administration. Use of real-world evidence to support regulatory decision-making for medical devices: guidance for industry and Food and Drug Administration staff. Docket number FDA-2016-D-2153. Updated September 17, 2018. Accessed July 21, 2025. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/use-real-world-evidence-support-regulatory-
decision-making-medical-devices.
5. Cullum N, Buckley H, Dumville J, et al. Chapter 5: Discussion. Wounds Research for Patient Benefit: a 5-Year Programme of Research (Programme Grants for Applied Research, No. 4.13). NIHR Journals Library; 2016. https://www.ncbi.nlm.nih.gov/books/NBK379913/
6. Klassen AF, van Haren ELWG, van Alphen TC, et al. International study to develop the WOUND-Q patient-reported outcome measure for all types of chronic wounds. Int Wound J. 2021;18(4):487-509. doi:10.1111/iwj.13549
7. Gallo L, Rae C, Voineskos S, et al. Further psychometric evaluation of the WOUND-Q: a responsiveness study. Wound Repair Regen. 2024;32(4):451-463. doi:10.1111/wrr.13179
8. Fife C; US Wound Registry. Unpublished data from the US Wound Registry. https://uswoundregistry.com/. Accessed July 24, 2025.
9. US Wound & Podiatry Registries. Measure the right thing: quality measures. US Wound & Podiatry Registries. https://uswoundregistry.com/quality-measures/
10. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). Hyattsville, MD: National Center for Health Statistics, Centers for Disease Control and Prevention. Updated annually. https://www.cdc.gov/nchs/icd/icd-10-cm/index.html. Accessed July 11, 2025.
11. Merkow RP, Kaji AH, Itani KMF. The CONSORT Framework. JAMA Surg. 2021 Sep 1;156(9):877-878. doi:10.1001/jamasurg.2021.0549
12. Carter MJ, DaVanzo J, Haught R, Nusgart M, Cartwright D, Fife CE. Chronic wound prevalence and the associated cost of treatment in Medicare beneficiaries: changes between 2014 and 2019. J Med Econ. 2023;26(1):894-901. doi:10.1080/13696998.2023.2232256
13. Carter MJ, Fife CE, Walker D, Thomson B. Estimating the applicability of wound care randomized controlled trials to general wound-care populations by estimating the percentage of individuals excluded from a typical wound-care population in such trials. Adv Skin Wound Care. 2009;22(7):316-324. doi:10.1097/01.ASW.0000305486.06358.e0
14. von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344-349. doi:10.1016/j.jclinepi.2007
15. U.S. Wound Registry. Analysis of bias criteria checklist for wound care registries & EHRs. 2019. https://uswoundregistry.com/wp-content/uploads/2019/07/USWR-White-Paper.pdf.


















