Do Fungi Play a Role in Rosacea?
It is well established that differences in the microbiome—the ecological community of microorganisms that live within and on the human body—play a role in the development of rosacea and affect the severity of signs and symptoms. Research shows that patients with rosacea often have an overgrowth of Demodex mites, a natural inhabitant of the skin of nearly every human, and mounting evidence points to an imbalance of bacteria in both the skin and gut microbiome as influencing the development and severity of rosacea signs and symptoms.1 However, a new study has focused on an overlooked portion of the microbiome that may also be involved in rosacea’s development: yeasts and other fungi.2
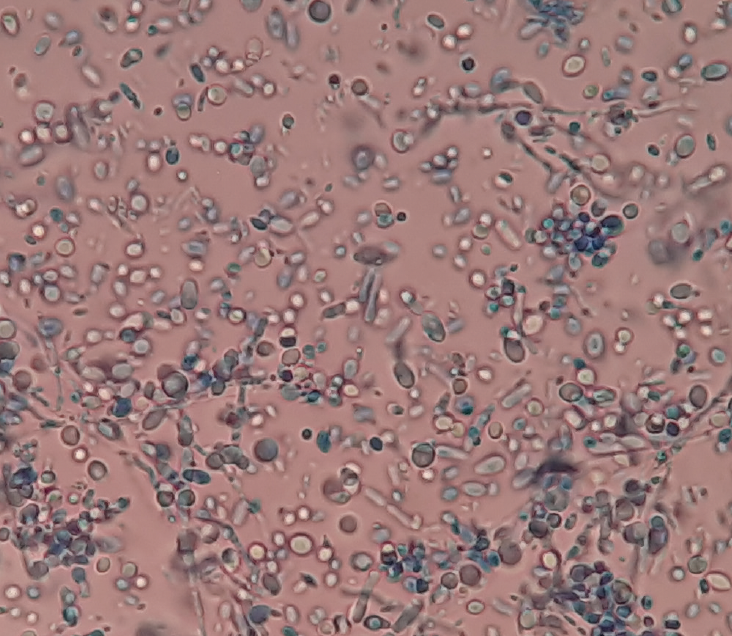
A team of researchers in Budapest, Hungary, collected skin, stool, and blood samples from 14 individuals with rosacea and 8 healthy control subjects, and performed genetic analysis on the samples to identify the bacterial and fungal species present in each. Blood samples were included to examine whether the bloodstream might be an avenue for changes in the gut microbiome to be transmitted to the skin.
The researchers noted that certain fungi in the microbiome, known as the mycobiome, have been shown to contribute to immune response, inflammation, and skin barrier disruption in eczema and seborrheic dermatitis.3 Changes in the variety and abundance of yeasts in the genus Malassezia appear to be involved. However, a previous study found no differences in the mycobiome of patients with rosacea compared to those with healthy skin.4
The new analysis also found no significant differences in terms of abundance or diversity of fungi in the skin, stool, or blood samples between the individuals with rosacea and the healthy control subjects. However, the investigators did find that among the patients with rosacea, fungi from 5 genera were present in significantly higher abundances in the skin samples than in stool or blood samples, with Malassezia species being the overwhelming majority. The stool samples of the individuals with rosacea had significantly greater abundances from 9 genera, especially Candida and Saccharomyces, compared to the skin and blood samples.
Although the skin of all study participants had high levels of Malassezia, only some subjects also had high levels of the yeast in their bloodstream, and this group had significantly higher levels of Cutibacterium on their skin. The investigators noted that some strains of Cutibacterium acnes have been found to contribute to an impaired skin barrier, which can lead to inflammation.
In the stool samples of the patients with rosacea, Candida was found at higher levels and Saccharomyces at lower levels compared to healthy controls. These fungi also exhibited relationships with bacteria. In the individuals with higher Saccharomyces levels, Prevotella and Agathobacter species, which offer anti-inflammatory benefits, were significantly more abundant. These beneficial bacteria were also more abundant in individuals with low levels of Candida.
The researchers concluded that imbalances in the mycobiome may contribute to the development of rosacea, and further study into the relationships between fungi and bacteria in the microbiome is needed.
Andrew Huff is the president and executive director of the National Rosacea Society.
This article is reprinted with permission from https://www.rosacea.org/ blog/2025/november/do-fungi-play-a-role-in-rosacea
References
1. Asees A, Sadur A, Choudhary S. The skin microbiome in rosacea: mechanisms, gut-skin interactions, and therapeutic implications. Cutis. 2025;116(1):20-23. doi:10.12788/cutis.1240
2. Joura MI, Nemes-Nikodém É, Jobbágy A, et al. Integrative analysis of fungal and bacterial microbiomes across skin, blood, and stool in rosacea patients. Int J Mol Sci. 2025;26(17):8127. doi:10.3390/ijms26178127
3. Jung WH. Alteration in skin mycobiome due to atopic dermatitis and seborrheic dermatitis. Biophys Rev (Melville). 2023;4:011309. doi:10.1063/5.0136543
4. Wang R, Farhat M, Na J, Li R, Wu Y. Bacterial and fungal microbiome characterization in patients with rosacea and healthy controls. Br J Dermatol. 2020;183(6):1112-1114. doi:10.1111/bjd.19315