A Rare Case of Cutaneous Metastasis of Hepatocellular Carcinoma to the Chin: Case Report and Review of Surgical Management
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Abstract
Hepatocellular carcinoma (HCC) is a debilitating complication of primary hepatic disease with a significant annual incidence worldwide. Untreated HCC may result in a severe reduction to life expectancy, dependent on staging at diagnosis. Typically, HCC has a propensity to metastasize to the lung, peritoneum, and bone. Cutaneous HCC metastases are rarely encountered, with few described in the literature. The authors present a case of a 66-year-old man with biopsy-proven cutaneous HCC metastasis to the chin. The patient was managed with excision, followed by staged reconstruction. Surgical management and a review of the literature are discussed.
Introduction
Hepatocellular carcinoma (HCC) has an annual incidence of 1% to 6% worldwide, with untreated cases demonstrating life expectancy reductions to 9 months, dependent upon staging.
Case Presentation
A 66-year-old man with a past medical history of hepatitis B, hyperlipidemia, and hypothyroidism was diagnosed with HCC confined to the liver in 2019. His initial management included partial hepatectomy with clear margins and no noted metastatic disease. A recurrent hepatic tumor and lung metastases were diagnosed 2 years later. Subsequent chemoembolization failed to control the disease. Concurrently, the patient noted a growing skin lesion on his chin that frequently hemorrhaged. A biopsy indicated metastatic HCC. The patient was referred to the plastic surgery clinic for evaluation and treatment.
Physical exam

Figure 1: Preoperative photograph demonstrating a 3.5 x 3.5-cm exophytic cutaneous mass located in the midline of the chin consistent with biopsy-proven metastatic hepatocellular carcinoma.
Diagnostic studies
Initial biopsy results of the chin lesion were reported as “carcinoma consistent with metastatic hepatocellular carcinoma, lesion transected at the deep and peripheral inked margins.” Surveillance PET scan demonstrated several new subcentimeter lung nodules consistent with progressive distant metastasis.
Treatment
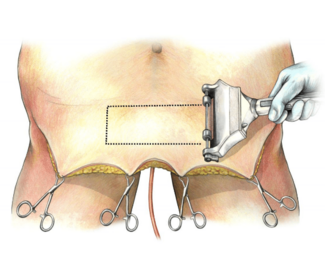
After collaborative discussion of the risks and benefits of palliative resection and reconstruction of the cutaneous lesion in the setting of metastatic HCC, excision was recommended. First-stage wide excision to the underlying musculature with wide margins was performed. A resultant 7 x 5-cm defect consisting of the chin subunit was temporized with placement of an Integra Bilayer Wound Matrix (Integra LifeSciences) and secured with a tie-over bolster (Figure 2). The specimen was sent for permanent pathologic evaluation of margins, which revealed adequate excision of the tumor with free margins.

Figure 2: Preoperative photograph at second-stage operation demonstrating a 7 x 5-cm open wound defect.
Reconstruction was performed 10 days after the index operation. The silicone layer of the wound matrix was removed, revealing a well-vascularized matrix. A 15 x 15-cm random pattern local skin advancement flap was designed caudal to the defect, incorporating the laxity of the submental and anterior neck skin. The flap was elevated in the pre-platysmal plane, extending to the level of the thyroid cartilage inferiorly and laterally to the anterior border of the masseter and sternocleidomastoid muscle bilaterally. The flap was advanced cephalad to resurface the entirety of the chin defect. Bilateral standing cutaneous deformities were addressed with M-plasties (Figure 3). A 10F Jackson-Pratt drain was placed subcutaneously in the neck. The patient was observed overnight and discharged on postoperative day 1 without issues.

Figure 3: Immediate postoperative photograph after inset of a 15 x 15-cm random pattern local advancement flap.
Follow-up
The flap healed well postoperatively, and the patient displayed preserved oral competence, full active neck range of motion, and intact mental nerve sensation (Figure 4). The patient proceeded with initiation of palliative immunochemotherapy with bevacizumab and atezolizumab for treatment of his other primary and metastatic sites.

Figure 4: One month postoperative, the incision was completely healed. The patient had intact oral competence and full neck range of motion.
Discussion
HCC most frequently results from cirrhotic liver disease; up to 80% of cirrhotic cases develop into HCC.
Metastasis primarily to lung, peritoneum, or bone is indicative of a poorer prognosis.
The clinical appearance of cutaneous metastatic HCC skin lesions varies significantly. Some case reports describe small, nodular-appearing lesions,
The importance of recognizing and treating HCC is highlighted by the fact that the appearance of skin lesions indicates likely metastasis to other organ systems such as the lungs.
Because of the limited life expectancy of our patient, we recommended palliative operative intervention to maintain his quality of life. Our patient did not demonstrate coagulopathy or delayed healing that would preclude surgical management of his cutaneous metastasis. Proceeding with operative palliation of the lesion would likely reduce the need for ongoing wound care, limit visits to health care clinics, decrease the financial burden, prevent frequent hemorrhage, and improve his limited quality of life. The patient stressed the importance of maintaining his usual appearance to continue to engage socially for the remainder of his life without stigma. We prioritized options with a quick recovery to maximize his time spent outside of the hospital.
A number of options exist for submental reconstruction. A pedicled submental flap can affect defect closure and be completed with a single operation, providing limited morbidity of the donor site.
Conclusions
In our management, a local advancement flap utilizing the redundancy of the submental and anterior neck skin and subcutaneous tissue was an ideal solution for this patient. It allowed reconstruction of the defect with like tissues, maintaining the patient’s normally styled facial hair. The operation was performed expeditiously, with minimal operative time. This rare case of metastatic HCC to the chin with palliative surgical management via local tissue advancement flap is an example of a treatment option that maintains patient dignity and quality of life in the context of a significantly shortened lifespan. Achieving satisfactory aesthetics, preserving functionality, and allowing for minimal social disruption in the patient’s life is a hallmark of reconstructive efforts, especially in the context of palliation for this patient.
Acknowledgments
Authors: Jonathan Ruiz, MD1; Jacqueline Ross, MD2; Kinsey Rice, MD2; Kristen Whalen, MD2; Nicole K. Le, MD, MPH2; Lisa Kettlestrings, PA-C3; Wyatt G. Payne, MD1,2,3
Affiliations: 1University of Central Florida College of Medicine, Orlando, Florida; 2University of South Florida Department of Plastic Surgery, Tampa, Florida; 3Bay Pines Veteran Affairs Healthcare System Plastic Surgery Section, Bay Pines, Florida
Correspondence: Wyatt G. Payne, MD, FACS, Bay Pines Veteran Affairs Healthcare Systems/Surgical Service (112), PO Box 5005, 10000 Bay Pines Blvd, Bay Pines, FL 33744, USA. Email: wyattgpayne@yahoo.com
Disclaimer: The contents of this work do not represent the views of the Department of Veterans Affairs or the United States Government.
Data availability: The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics: Written informed consent was received from the patient regarding the utilization and publication of the clinical data and images presented in this case report.
Disclosures: The authors disclose no relevant financial or nonfinancial interests.
References
- Llovet JM, Kelley RK, Villanueva A, et al. Hepatocellular carcinoma. Nat Rev Dis Primers. 2021;7(1):6. doi:10.1038/s41572-020-00240-3.
-
Giannini EG, Farinati F, Ciccarese F, et al. Prognosis of untreated hepatocellular carcinoma. Hepatology. 2015;61(1):184-190. doi:10.1002/hep.27443.
-
Abbas A, Medvedev S, Shores N, et al. Epidemiology of metastatic hepatocellular carcinoma, a nationwide perspective. Dig Dis Sci. 2014;59(11):2813-2820. doi:10.1007/s10620-014-3229-9.
-
Targe M, Yasam VR, Nagarkar R. Hepatocellular carcinoma with uncommon sites of metastasis: a rare case report. Egypt J Radiol Nucl Med. 2021;52:228. doi:10.1186/s43055-021-00612-z.
-
Reuben S, Owen D, Lee P, Weiss A. Hepatocellular carcinoma with cutaneous metastases. Can J Gastroenterol. 2009;23(1):23-25. doi:10.1155/2009/274357.
-
de Agustín P, Conde E, Alberti N, Pérez-Barrios A, López-Ríos F. Cutaneous metastasis of occult hepatocellular carcinoma: a case report. Acta Cytol. 2007;51(2):214-216. doi:10.1159/000325720.
-
Subasinghe D, Keppetiyagama CT, Sudasinghe H, Wadanamby S, Perera N, Sivaganesh S. Solitary scalp metastasis—a rare presentation of hepatocellular carcinoma. Ann Surg Innov Res. 2015;9:4. doi:10.1186/s13022-015-0013-2.
-
Ackerman D, Barr RJ, Elias AN. Cutaneous metastases from hepatocellular carcinoma. Int J Dermatol. 2001;40(12):782-784. doi:10.1046/j.1365-4362.2001.01319.x.
-
Kubota Y, Koga T, Nakayama J. Cutaneous metastasis from hepatocellular carcinoma resembling pyogenic granuloma. Clin Exp Dermatol. 1999;24(2):78-80. doi:10.1046/j.1365-2230.1999.00423.x.
-
Amador A, García Monforte N, Bejarano N, et al. Cutaneous metastasis from hepatocellular carcinoma as the first clinical sign. J Hepatobiliary Pancreat Surg. 2007;14(3):328-330. doi:10.1007/s00534-006-1141-1.
-
Raza A, Sood GK. Hepatocellular carcinoma review: current treatment and evidence-based medicine. World J Gastroenterol. 2014;20(15):4115-4127. doi:10.3748/wjg.v20.i15.4115.
-
Saito A, Toyoda H, Kobayashi M, et al. Prediction of early recurrence of hepatocellular carcinoma after resection using digital pathology images assessed by machine learning. Mod Pathol. 2021;34(2):417-425. doi:10.1038/s41379-020-00671-z.
-
Aggarwal A, Te HS, Verna EC, Desai AP. A national survey of hepatocellular carcinoma surveillance practices following liver transplantation. Transplant Direct. 2021;7(1):e638. doi:10.1097/TXD.0000000000001086.
-
El-Serag HB, Davila JA. Surveillance for hepatocellular carcinoma: in whom and how? Therap Adv Gastroenterol. 2011;4(1):5-10. doi:10.1177/1756283X10385964.
-
Lazaro M, Allende I, Ratón JA, Acebo E, Diaz-Perez JL. Cutaneous metastases of hepatocellular carcinoma. Clin Exp Dermatol. 2009;34(8):e567-e569. doi:10.1111/j.1365-2230.2009.03245.x.
-
Zeng JX, Tian X, Zhu HL, Zhang XB, Luo Q. A case of hepatocellular carcinoma diagnosed as facial cutaneous metastasis survives for 18 months. Chin Med J (Engl). 2019;132(5):616-617. doi:10.1097/CM9.0000000000000083.
-
Nggada HA, Ajayi NA. Cutaneous metastasis from hepatocellular carcinoma: a rare presentation and review of the literature. Afr J Med Med Sci. 2006;35(2):181-182.
-
Faisal M, Adeel M, Riaz S, et al. The submental island flap in head and neck cancer. Ann Maxillofac Surg. 2018;8(2):287-291. doi:10.4103/ams.ams_225_18.
-
Liu M, Liu W, Yang X, Guo H, Peng H. Pectoralis major myocutaneous flap for head and neck defects in the era of free flaps: harvesting technique and indications. Sci Rep. 2017;7:46256. doi:10.1038/srep46256.
-
Brenner MJ, Moyer JS. Skin and composite grafting techniques in facial reconstruction for skin cancer. Facial Plast Surg Clin North Am. 2017;25(3):347-363. doi:10.1016/j.fsc.2017.03.007.