Negative Pressure Wound Therapy for Management of Achilles Region Defects: A Systematic Review of the Literature
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Wounds or HMP Global, their employees, and affiliates.
Abstract
Background. Despite the efforts of plastic and orthopedic surgeons to elaborate the most appropriate treatment for lesions of the Achilles region and their reconstruction, no universal guideline exists. Regenerative treatments such as negative pressure wound therapy (NPWT) are increasingly being used in the management of these defects. Objective. To research the different usage protocols, roles, and outcomes of NPWT in the management and reconstruction of Achilles region defects. Methods. A scientific literature search was performed by querying Medline and Scopus using the terms “(Achilles tendon) AND ((vac) OR (vacuum assisted closure) OR (negative pressure) OR (NPWT)).” The authors used an online screening software. The investigation followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement for systematic review. Results. Of the initial 153 studies identified, only 14 fulfilled the eligibility criteria and were included in this review. Analyzed protocols mainly included surgical debridement combined with the use of NPWT as a primary dressing directly on the tendon or as a secondary dressing covering a split-thickness skin graft (STSG) or a flap. Additionally, the combination of negative pressure with matrices was found to provide optimal results even after STSG failure. Most of the reported complications described in the included studies involved partial loss of graft or flap. Conclusion. NPWT can be used either as a primary dressing (directly on the lesion) or as a secondary dressing (over a flap or a skin graft) for management of Achilles region defects. The combined use of negative pressure with matrices can also aid in wound reduction.
Abbreviations: ATR, Achilles tendon rupture; DLQI, Dermatology Life Quality Index; NPWT, negative pressure wound therapy; PICOT, population, intervention, comparator, outcome, time; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; PTAPF, posterior tibial artery perforator flap; STSG, split-thickness skin graft.
Although the Achilles tendon is the largest and strongest tendon in the human body,1 it has a rupture incidence rate ranging from 2.5 to 47 per 100 000 person-years in Europe and North America.2,3 The incidence of this medical condition is reportedly highest in males aged 40 to 49 years.4 Intrinsic and extrinsic predisposing factors for ATR have been previously described in the scientific literature.5-8 Sports and trauma are among the main factors related to soft tissue wounds of the Achilles region.9
Anatomically, despite the large tendon capacity, the Achilles region is particularly delicate due to the small thickness of the soft tissues covering the noble structures.1,10 Following trauma, exposure of the tendon is not unusual.
Various conservative and nonconservative treatments for ATR have been proposed and described in the scientific literature.11-13 Despite the efforts of plastic and orthopedic surgeons to elaborate the most appropriate treatment for lesions of the Achilles region and their reconstruction,14-16 as of this writing no universal guideline exists.
Infections, hematomas, necrosis, and other complications can contribute to increasing the rate of re-rupture, which may reach up to 2% when adopting nonsurgical protocols.17 Despite this, in cases of re-rupture, deep burns, infections, severe necrosis, and complex traumas of the Achilles region, conservative treatments based on regenerative medicine, such as the application of NPWT, are increasingly being used in plastic surgery and orthopedics to manage these defects.14,16 NPWT not only aids in stabilizing the wound environment, but it also tends to reduce edema and bacterial load while improving tissue perfusion and angiogenesis, and stimulating granulation tissue formation.18
The aim of this systematic review was to research the different NPWT usage protocols, roles, and outcomes in the management and reconstruction of the Achilles region.
Methods
Eligibility criteria
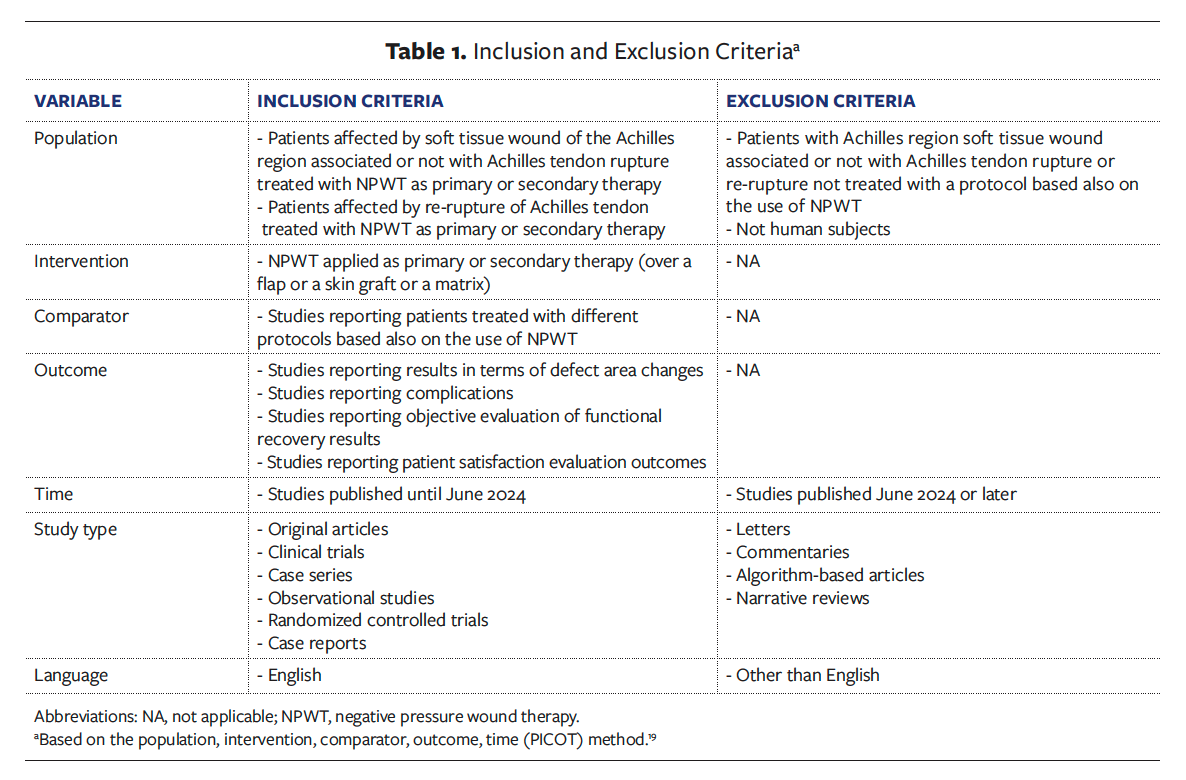
Inclusion and exclusion criteria were formulated according to the PICOT method19 and are reported in Table 1.
Search strategy and information sources
The authors of the present review performed a scientific literature search for the various NPWT usage protocols, roles, and outcomes in the management and reconstruction of the Achilles region by querying the Medline database and Scopus (Elsevier BV) using the following terms and Boolean operators: “(Achilles tendon) AND ((vac) OR (vacuum assisted closure) OR (negative pressure) OR (NPWT)).”
The search strategy was performed independently by each author in June 2024. Keywords and Medical Subject Headings terms were detected in a preliminary setting by discussion among all authors of this review. In the preliminary setup, a date filter was not used; because the search was performed in June 2024, the authors commonly decided to stop the search at articles published within that month. Initially, no language restriction filter was applied; however, only English-language articles were selected during the screening process.
The authors used online screening software (RAYYAN) to import all the articles to be screened. Through a “blind-on mode,” the reviewers retrieved the data and independently analyzed each selected study. Articles tagged as “maybe” or “undecided” and other conflicts were resolved by the senior investigator (M.G.). Furthermore, duplicates were initially detected with a specific function and then resolved. The articles were screened for the presence of the inclusion criteria reported in Table 1. Articles for which full text was not available were excluded. The studies involving only patients with Achilles region soft tissue wound associated or not with ATR or Achilles tendon re-rupture not treated with a protocol based also on the use of NPWT were excluded. Letters, commentaries, narrative reviews, and algorithm-based articles not reporting clinical results were excluded from this systematic review. Authors used an internal, shared Excel worksheet (Microsoft Corporation) as a data collection system. Reviewers used uniform labeling for the data items and their setting (measures, time points, analyses) and for the list of abbreviations. Regarding the synthesis method, in case reports with multiple patients, standardization was achieved by having each reviewer summarize each case independently (eg, Case 1:...; Case 2:...).
The investigation followed the PRISMA 2020 statement for systematic review.20
Results
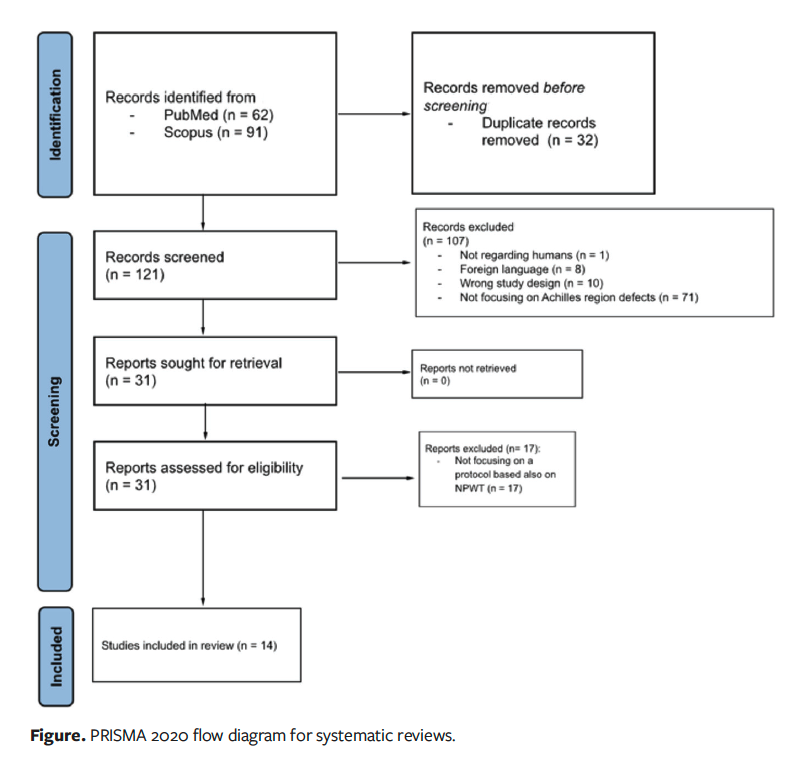
The initial search produced 153 studies, with 62 articles imported from PubMed and 91 from Scopus. Sixty-three duplicate articles were identified and resolved through a specific function of the online screening software. The screening process started with 121 articles, with the reviewers reading the title, abstract, language, study type, and applying the inclusion and exclusion criteria, and only after that reading the full text. A total of 107 studies were excluded for the following reasons: 1 was not a human study, 8 were written in a language other than English, 10 had the “wrong study design,” 71 did not focus on Achilles region defects, and 17 did not focus on a protocol that included NPWT. After the screening process, only 14 studies fulfilled the previously noted eligibility criteria and were included in the current study. The PRISMA flowchart for study selection is shown in the Figure.
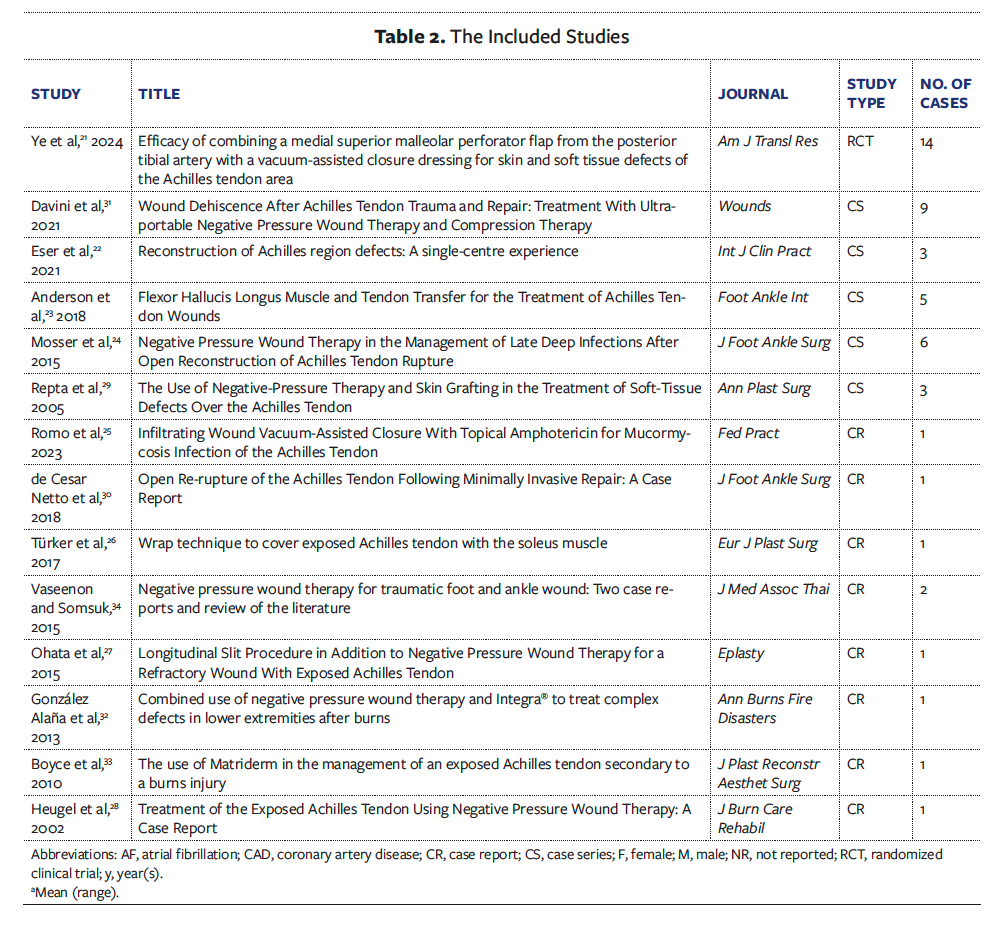
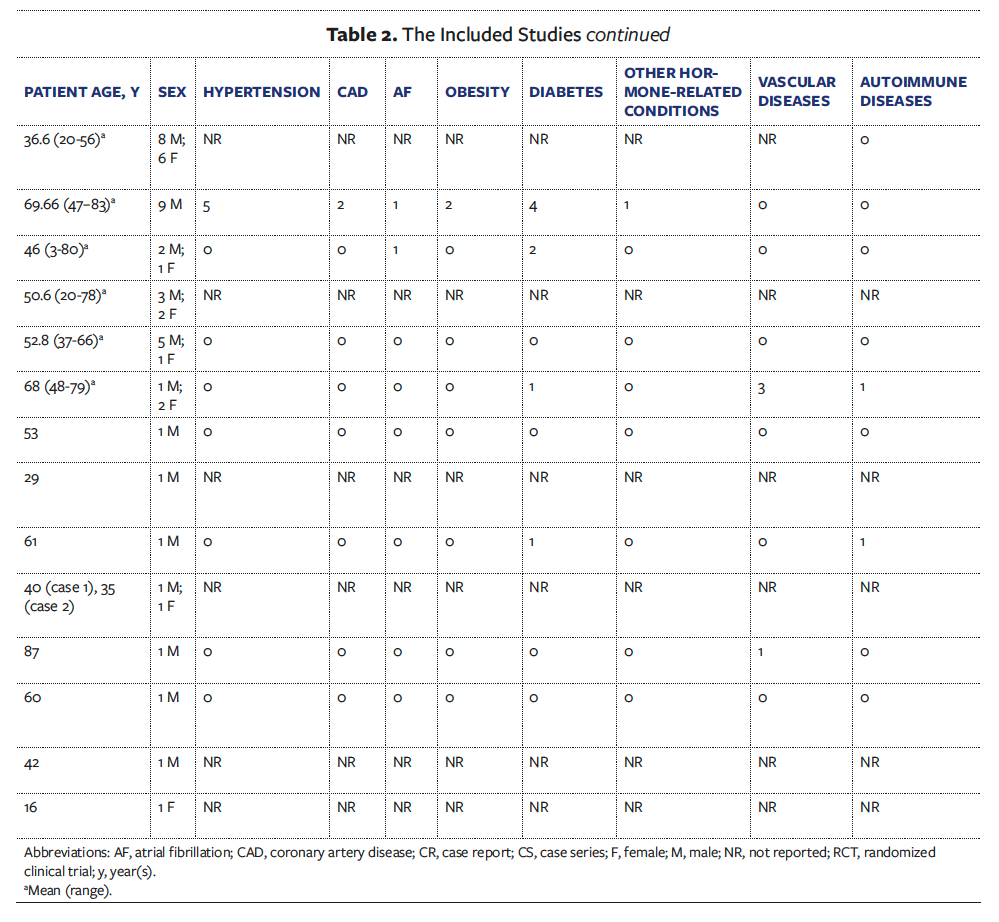
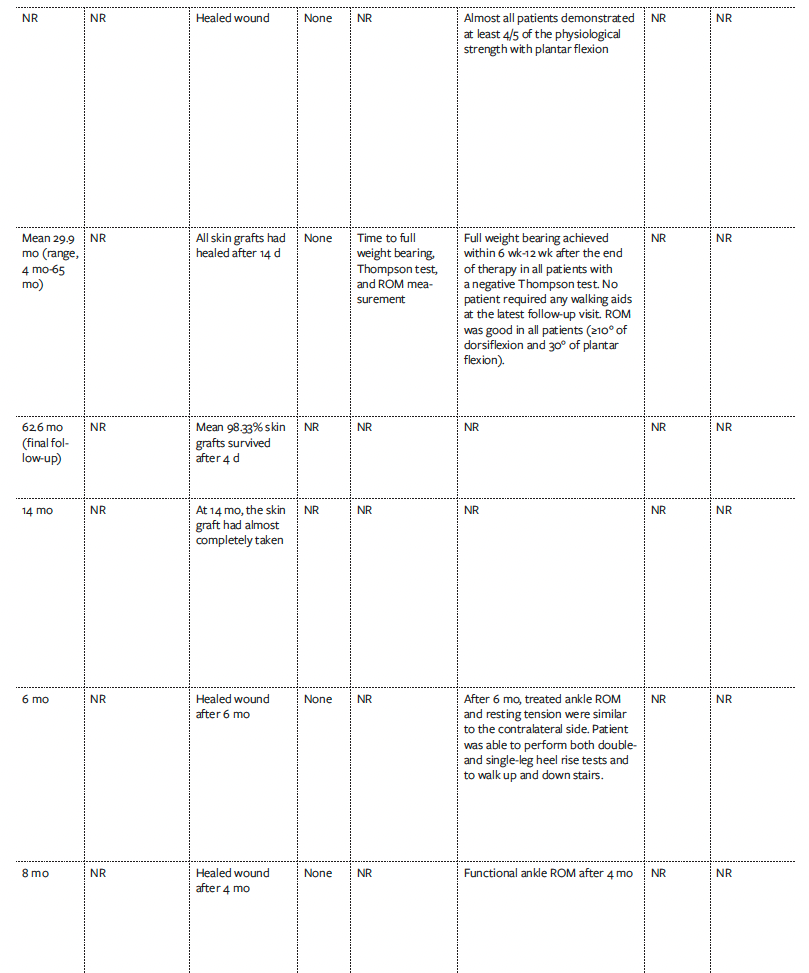
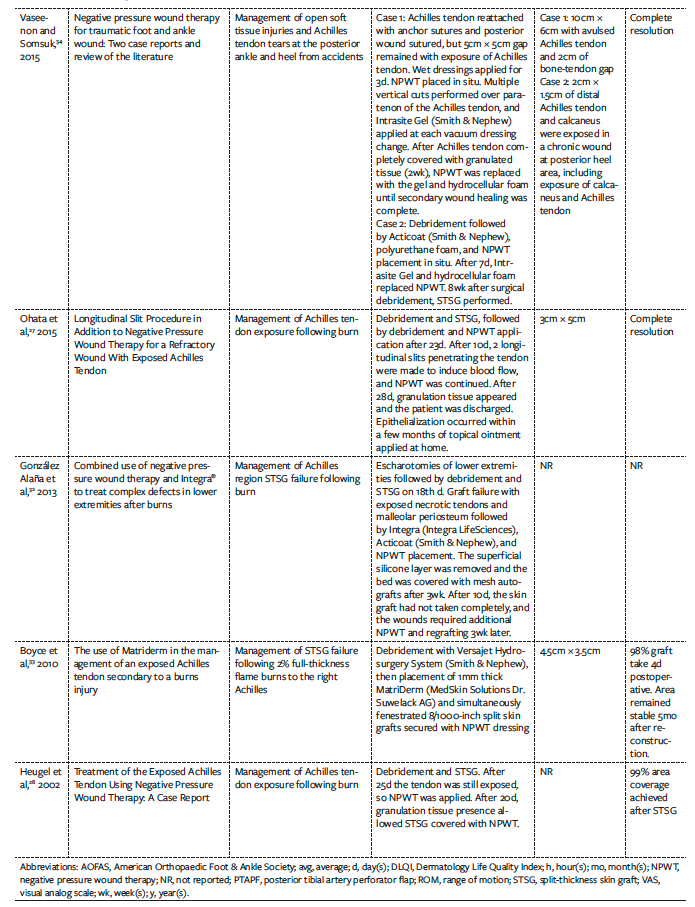
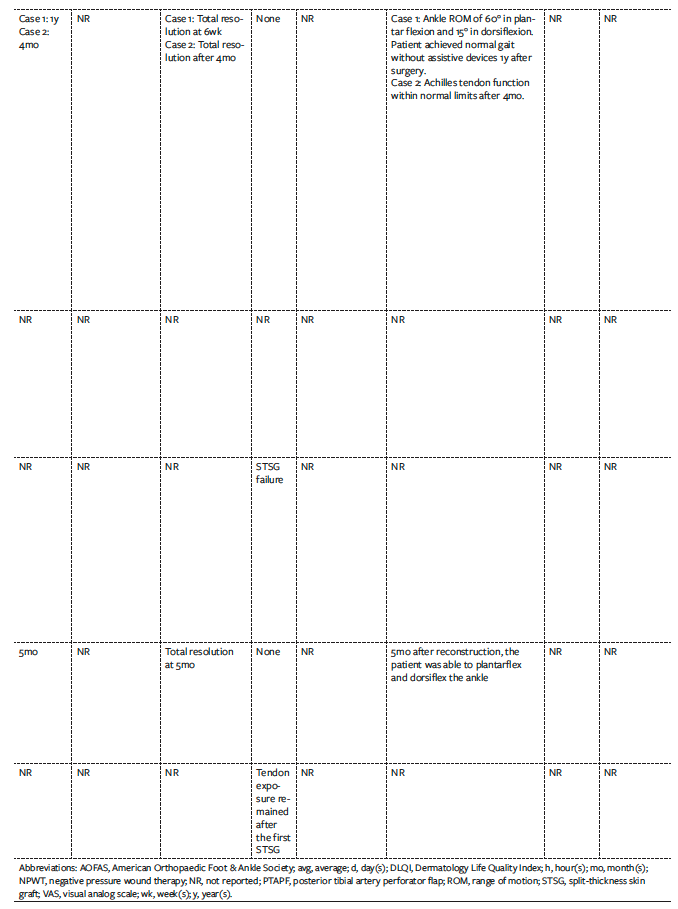
One randomized clinical trial, 5 case series, and 8 case reports were included in the systematic review of the literature (Table 2). These articles were published between 2002 and 2024. A total of 49 patients were included in this study, ranging in age between 3 years and 87 years. The vast majority of patients were males (35 males, 14 females). The overall mean follow-up time was 18.22 months; however, this data point was not reported in 5 of the included articles.
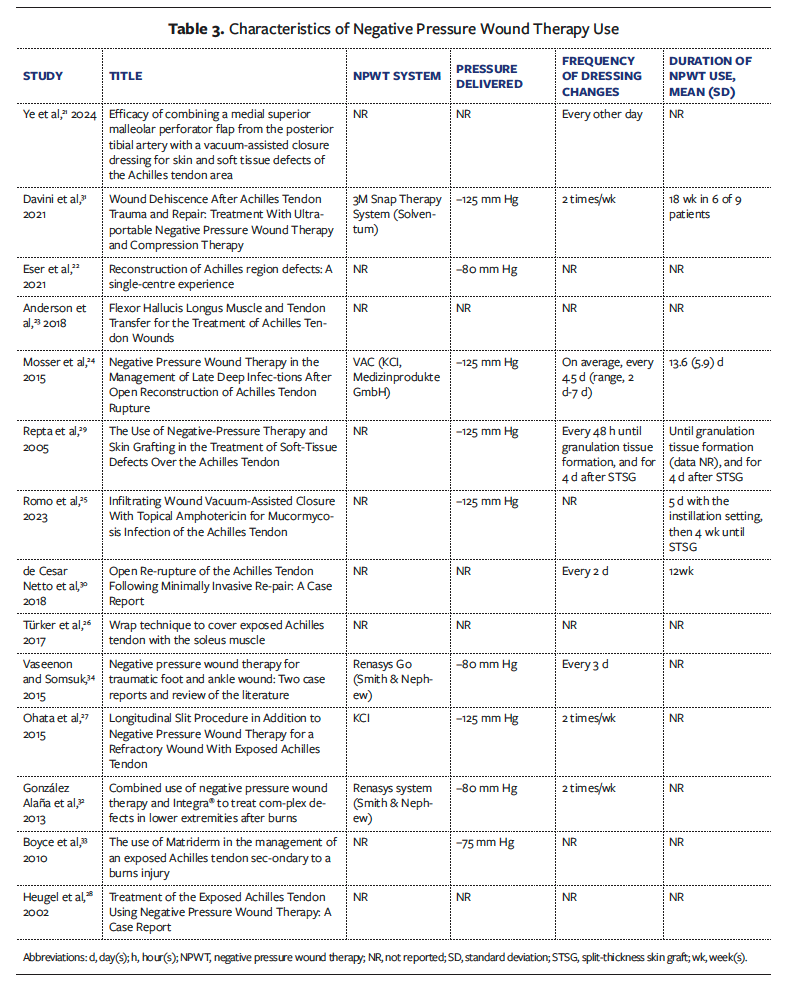
The specific NPWT system was reported in 5 articles, with 2 using a Renasys system (Smith & Nephew),32,34 2 using VAC (KCI),24,27 and 1 using the 3M Snap Therapy System (Solventum).31 In 5 articles the pressure delivered was −125 mm Hg,24,25,27,29,31 in 3 articles the pressure was −80 mm Hg,22,32,34 and in 1 article the pressure was −75 mm Hg.33 This information was not reported in 5 articles. Frequency of dressing changes ranged from every 2 days to twice a week.
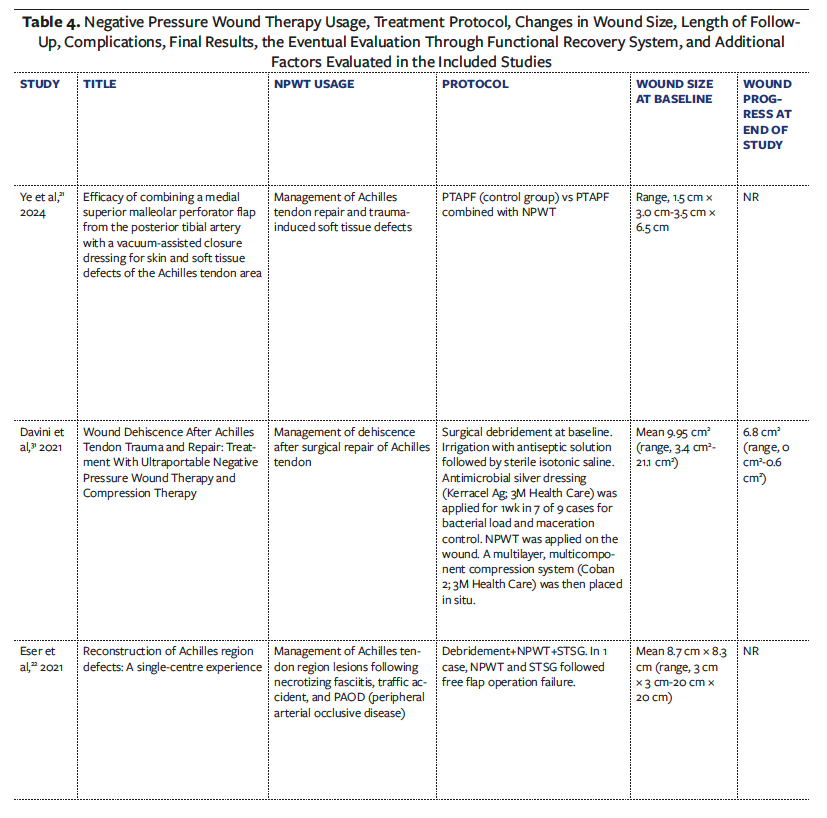
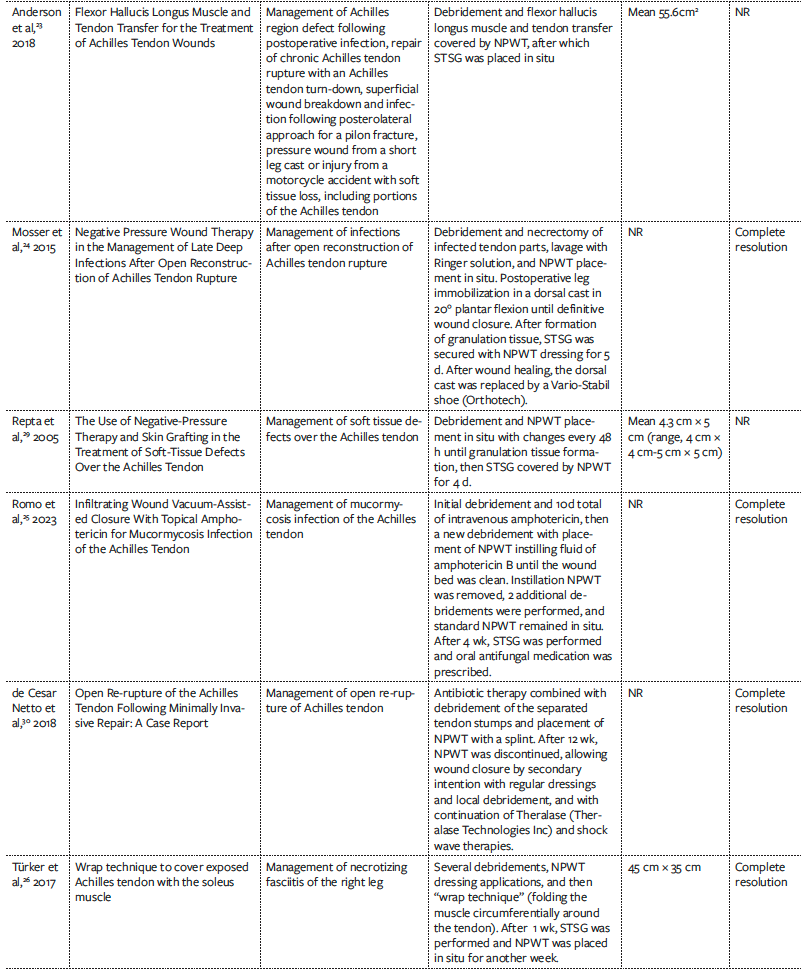
Analyzed protocols mainly included surgical debridement combined with the use of NPWT as the primary dressing directly on the tendon or as a secondary dressing covering an STSG or a flap.21-28
In some cases NPWT was described as useful until the formation of granulation tissue, after which the wound was eventually covered with an STSG or closed by secondary intention.29,30
Other protocols based on the combination of NPWT with other secondary dressings over time were described with satisfactory results.31 Additionally, the combination of negative pressure with matrices provides optimal results, although several steps are required.32,33
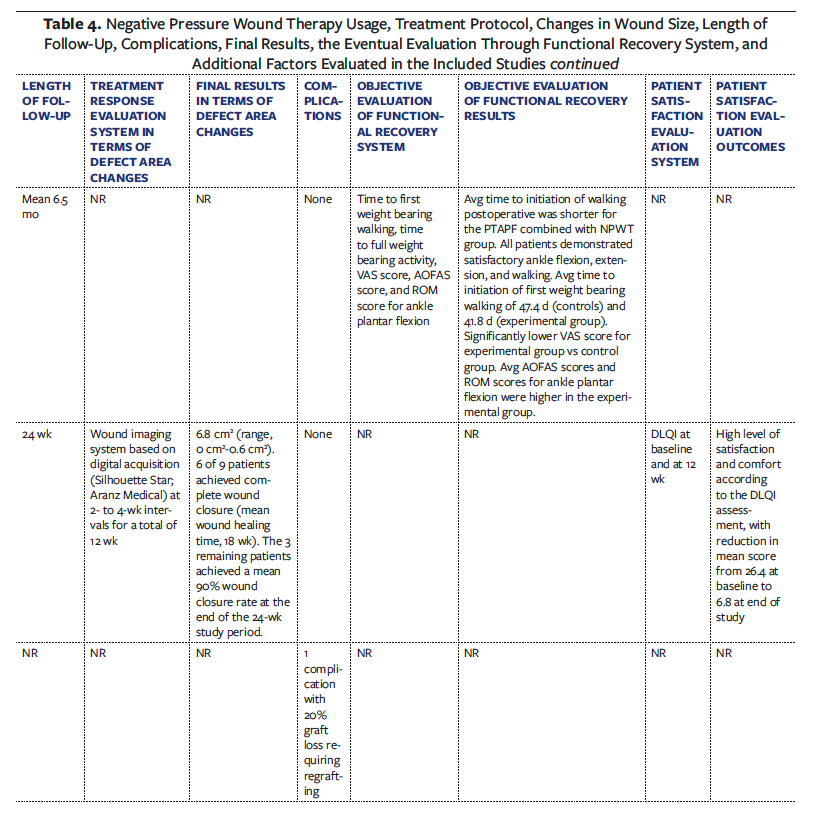
Most of the reported complications described in the included articles consisted of partial loss of graft or flap. In these cases, the NPWT and regrafting22,28,34 or matrix (eg, Integra; Integra LifeSciences32) has proven useful in achieving a decrease in wound area. Davini et al31 investigated patient satisfaction at baseline and at 12 weeks using the DLQI.
Characteristics regarding NPWT use in each study are summarized in Table 3, including the type of NPWT used, pressure delivered, frequency of dressing changes, and average duration of NPWT use. Table 4 lists the type of NPWT used, usage protocol, centimetric variations over time, length of follow-up, complications, results, evaluation of the functional recovery system, and patient satisfaction evaluation.
Discussion
The incidence of ATR has increased in industrialized countries in the past 2 decades.35 It is generally accepted that surgery is the primary treatment for ATR in young and physically active patients, whereas conservative treatments may be acceptable in older patients with sedentary lifestyles.36 Surgical repair is generally related to an early return to sport.37
The clinical condition is not always easy to resolve. Etiology includes complete and partial rupture of the Achilles tendon, as well as trauma, burns, degenerative diseases, vascular diseases, and intrinsic and extrinsic predisposing factors, with resulting injuries of varying severity. Injury severity can potentially range from bone exposure to simple de-epithelialization.38
There are no globally accepted guidelines for the treatment, management, and reconstruction of different types of Achilles region defects. However, several articles in the scientific literature highlight the experience of individual centers in managing such lesions through conservative and nonconservative treatments.
Currently, increasing numbers of authors are using new conservative treatments, especially for chronic ulcerated lesions that are not prone to healing easily. Platelet-rich plasma, adipose-
derived stem cells, and NPWT are conservative regenerative treatments that can potentially help patients with conditions that negatively affect their quality of life long-term.39-41
With NPWT, negative pressure is applied to wounds to promote the healing process.42 Subatmospheric pressure generated within a closed dynamic delivery system can be delivered continuously or discontinuously.43,44 Newer NPWT systems allow for the selection of the negative pressure to be delivered.44 The effects of NPWT with instillation and dwell time have been described in orthoplastic surgery.45 Such treatment allows increased local blood flow, has the potential to reduce edema and local bacterial load, and allows granulation tissue to develop.43 It is also helpful in facilitating easier grafting of the defect area.46 In their 2018 review article, Yin et al46 confirmed what was also observed by Romo et al25 and Repta et al,29 who successfully performed STSG after debridement and achieved granulation tissue formation with the application of NPWT.
NPWT can also be used simultaneously with STSG or flap to facilitate improved graft take. In 2017, Türker et al26 described using a wrap technique to cover exposed Achilles tendon with the soleus muscle. In that case report, they also described the use of NPWT and skin graft beginning 1 month after the wrap technique, with complete resolution of necrotizing fasciitis of the right leg after only 8 months.
Flexor hallucis longus muscle and tendon transfer is another effective treatment option for Achilles tendon wounds. In the 5 patients in the case series by Anderson et al,23 NPWT and skin graft had to be applied after this procedure. The combination of medial superior malleolar PTAPF with a vacuum-assisted closure dressing proved effective for the management of Achilles tendon repair and trauma-
induced soft tissue defects in the randomized clinical trial published by Ye et al21 in 2024. In that study, patients treated with NPWT in addition to PTAPF had superior outcomes compared with patients treated with PTAPF alone.
Some types of negative pressure devices also allow infiltration of the tissues being treated. Romo et al25 described in a case report the instillation of amphotericin B fluid until the wound bed was sufficiently clean for STSG.
Achilles tendon re-rupture is a possibility that needs to be considered even when the primary treatment used to correct the defect is surgical.9 The authors of a 2018 case report successfully treated a re-rupture of the Achilles tendon following minimally invasive repair through antibiotic therapy combined with debridement of the separated tendon stumps and placement of NPWT with a splint.30 After 12 weeks, NPWT was discontinued to allow wound closure by secondary intention with the combination of regular dressings and local debridement, Theralase (Theralase Technologies Inc), and shock wave therapies.
The combination of NPWT with matrices has also been described in a case of STSG failure.32 Similarly, a 2010 case report discussed the application of −75 mm Hg combined with MatriDerm (MedSkin Solutions Dr. Suwelack AG) for the management of STSG failure following 2% full-thickness flame burns on the right Achilles.
Of the 14 trials included in the present study, only 1 assessed patient satisfaction based on the DLQI (at baseline and at 12 weeks).31 Modern medicine increasingly uses patient-reported outcome measures to understand and study the most appropriate type of treatment for the patient based on the patient’s subjective experience, and more studies need to include patient satisfaction evaluation outcomes.47-50
Limitations
The present study has limitations. The variability in treatment protocols and follow-up durations between studies makes it difficult to draw definitive conclusions and indications for the management of Achilles region defects. Small sample sizes and retrospective study designs limit the generalizability of the findings of this systematic review. Furthermore, the lack of large-scale prospective studies in this field leaves a notable gap in the literature that has not yet enabled the development of universally accepted evidence-based guidelines. Additional limitations of the present study include the exclusion of letters, commentaries, algorithm-based articles, and other narrative reviews and articles that are not English-language publications. Finally, because of the poor data derived from the included studies, results were not stratified based on patient population characteristics, wound etiology, comorbidities, treatment duration, number of procedures, smoking status, vascular status, recurrence rates, and other medical conditions.
Conclusion
NPWT can be used as either a primary dressing (directly on the lesion) or a secondary dressing (over a flap or a skin graft) for management of Achilles region defects. The combination of negative pressure with matrices can be a valid option. The findings of the present review did not permit creation of a definition of a universally accepted way to use NPWT in the management of Achilles region defects.
Author and Public Information
Authors: Marco Gratteri, MD1; Claudia Luciano, MD2; Fara Desiree Romano, MD1; Luigi Abate, MD1; Carlo Mirra, MD1; Luca Savani, MD1; Giuseppe Francesco Papalia, MD3; Rocco Papalia, MD, PhD3; Pasquale Farsetti, MD, PhD2; Giovanni Francesco Marangi, MD, PhD1; and Paolo Persichetti, MD, PhD1
Affiliations: 1Department of Plastic, Reconstructive and Aesthetic Surgery, Campus Bio-Medico University of Rome, Rome, Italy; 2Section of Orthopaedics and Traumatology, Department of Clinical Science and Translational Medicine, University of Rome “Tor Vergata,” Rome, Italy; 3Department of Orthopaedic and Trauma Surgery, Campus Bio-Medico University of Rome, Rome, Italy.
Disclosure: The authors declare that they have no conflicts of interest to disclose. The authors did not receive any financial support for the research, authorship, or publication of this article.
Data Availability: Collected data can be requested from the corresponding author.
Ethical Approval: Not required.
Correspondence: Fara Desiree Romano, MD, Department of Plastic, Reconstructive and Aesthetic Surgery, Campus Bio-Medico University of Rome, Via Alvaro del Portillo 200, 00128, Rome, Italy; faradesiree.romano@unicampus.it
Date Accepted: March 4, 2025
References
1. O’Brien M. The anatomy of the Achilles tendon. Foot Ankle Clin. 2005;10(2):225-238. doi:10.1016/j.fcl.2005.01.011
2. Leino O, Keskinen H, Laaksonen I, Mäkelä K, Löyttyniemi E, Ekman E. Incidence and treatment trends of Achilles tendon ruptures in Finland: a nationwide study. Orthop J Sports Med. 2022;10(11):23259671221131536. doi:10.1177/23259671221131536
3. Huttunen TT, Kannus P, Rolf C, Felländer-Tsai L, Mattila VM. Acute achilles tendon ruptures: incidence of injury and surgery in Sweden between 2001 and 2012. Am J Sports Med. 2014;42(10):2419-2423. doi:10.1177/0363546514540599
4. Sheth U, Wasserstein D, Jenkinson R, Moineddin R, Kreder H, Jaglal SB. The epidemiology and trends in management of acute Achilles tendon ruptures in Ontario, Canada: a population-based study of 27 607 patients. Bone Joint J. 2017;99-B(1):78-86. doi:10.1302/0301-620X.99B1.BJJ-2016-0434.R1
5. Xergia SA, Tsarbou C, Liveris NI, Hadjithoma M, Tzanetakou IP. Risk factors for Achilles tendon rupture: an updated systematic review. Phys Sportsmed. 2023;51(6):506-516. doi:10.1080/00913847.2022.2085505
6. Claessen FMAP, de Vos RJ, Reijman M, Meuffels DE. Predictors of primary Achilles tendon ruptures. Sports Med. 2014;44(9):1241-1259. doi:10.1007/s40279-014-0200-z
7. Park YH, Kim TJ, Choi GW, Kim HJ. Age is a risk factor for contralateral tendon rupture in patients with acute Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc. 2020;28(5):1625-1630. doi:10.1007/s00167-019-05380-y
8. Hartman H, Cacace A, Leatherman H, et al. Gender differences in Achilles tendon ruptures-a retrospective study and a review of the literature. J Foot Ankle Surg. Published online May 17, 2024:S1067-2516(24)00087-5. doi:10.1053/j.jfas.2024.04.005
9. Bullock M, Pierson Z. Achilles tendon rupture. Clin Podiatr Med Surg. 2024;41(3):535-549. doi:10.1016/j.cpm.2024.01.009
10. Winnicki K, Ochała-Kłos A, Rutowicz B, Pękala PA, Tomaszewski KA. Functional anatomy, histology and biomechanics of the human Achilles tendon - a comprehensive review. Ann Anat. 2020;229:151461. doi:10.1016/j.aanat.2020.151461
11. Park SH, Lee HS, Young KW, Seo SG. Treatment of acute Achilles tendon rupture. Clin Orthop Surg. 2020;12(1):1-8. doi:10.4055/cios.2020.12.1.1
12. Silbernagel KG, Hanlon S, Sprague A. Current clinical concepts: conservative management of Achilles tendinopathy. J Athl Train. 2020;55(5):438-447. doi:10.4085/1062-6050-356-19
13. Patch DA, Andrews NA, Scheinberg M, et al. Achilles tendon disorders: an overview of diagnosis and conservative treatment. JAAPA. 2023;36(10):1-8. doi:10.1097/01.JAA.0000977720.10055.c4
14. Liles J, Adams SB. Management of complications of Achilles tendon surgery. Foot Ankle Clin. 2019;24(3):447-457. doi:10.1016/j.fcl.2019.04.008
15. Winters B, Da Rin de Lorenzo F, Beck D. What is the treatment “algorithm” for infection after Achilles tendon repair/reconstruction? Foot Ankle Int. 2019;40(1_suppl):71S-73S. doi:10.1177/1071100719861646
16. Innocenti M, Innocenti A, Ghezzi S, Delcroix L. Achilles region soft-tissue defects: a reconstructive algorithm based on a series of 46 cases. J Reconstr Microsurg. 2017;33(S 01):S40-S47. doi:10.1055/s-0037-1606554
17. Briggs-Price S, Mangwani J, Houchen-Wolloff L, et al. Incidence, demographics, characteristics and management of acute Achilles tendon rupture: an epidemiological study. PLoS One. 2024;19(6):e0304197. doi:10.1371/journal.pone.0304197
18. Agarwal P, Kukrele R, Sharma D. Vacuum assisted closure (VAC)/negative pressure wound therapy (NPWT) for difficult wounds: a review. J Clin Orthop Trauma. 2019;10(5):845-848. doi:10.1016/j.jcot.2019.06.015
19. Riva JJ, Malik KMP, Burnie SJ, Endicott AR, Busse JW. What is your research question? An introduction to the PICOT format for clinicians. J Can Chiropr Assoc. 2012;56(3):167-171.
20. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi:10.1136/bmj.n71
21. Ye H, Xu X, Sun Y, Zhao X. Efficacy of combining a medial superior malleolar perforator flap from the posterior tibial artery with a vacuum-assisted closure dressing for skin and soft tissue defects of the Achilles tendon area. Am J Transl Res. 2024;16(4):1209-1218. doi:10.62347/LSIM3562
22. Eser C, Karagoz Ceylan OI, Gencel E, Tabakan I, Kokacya O, Yavuz M. Reconstruction of Achilles region defects: a single-centre experience. Int J Clin Pract. 2021;75(12):e14908. doi:10.1111/ijcp.14908
23. Anderson MR, Bell DE, Ketz JP. Flexor hallucis longus muscle and tendon transfer for the treatment of Achilles tendon wounds. Foot Ankle Int. 2018;39(2):205-209. doi:10.1177/1071100717739395
24. Mosser P, Kelm J, Anagnostakos K. Negative pressure wound therapy in the management of late deep infections after open reconstruction of achilles tendon rupture. J Foot Ankle Surg. 2015;54(1):2-6. doi:10.1053/j.jfas.2014.09.040
25. Romo MA, Leach G, Reid CM, Dean RA, Suliman A. Infiltrating wound vacuum-assisted closure with topical amphotericin for mucormycosis infection of the Achilles tendon. Fed Pract. 2023;40(2):47-49. doi:10.12788/fp.0359
26. Türker T, Lawson K, Larson EE. Wrap technique to cover exposed Achilles tendon with the soleus muscle. Eur J Plast Surg. 2017;40(1):57-60. doi:10.1007/s00238-016-1214-6
27. Ohata E, Yuzuriha S, Mishima Y, Matsuo K. Longitudinal slit procedure in addition to negative pressure wound therapy for a refractory wound with exposed achilles tendon. Eplasty. 2015;15:e9.
28. Heugel JR, Parks KS, Christie SS, Pulito JF, Zegzula DH, Kemalyan NA. Treatment of the exposed Achilles tendon using negative pressure wound therapy: a case report. J Burn Care Rehabil. 2002;23(3):167-171. doi:10.1097/00004630-200205000-00005
29. Repta R, Ford R, Hoberman L, Rechner B. The use of negative-pressure therapy and skin grafting in the treatment of soft-tissue defects over the Achilles tendon. Ann Plast Surg. 2005;55(4):367-370. doi:10.1097/01.sap.0000181342.25065.60
30. de Cesar Netto C, Bernasconi A, Roberts L, Saito GH, Hamilton WG, O’Malley MJ. Open re-rupture of the Achilles tendon following minimally invasive repair: a case report. J Foot Ankle Surg. 2018;57(6):1272-1277. doi:10.1053/j.jfas.2018.04.002
31. Davini G, Dini V, Janowska A, et al. Wound dehiscence after Achilles tendon trauma and repair: treatment with ultraportable negative pressure wound therapy and compression therapy. Wounds. 2021;33(12):E93-E98.
32. González Alaña I, Torrero López JV, Martín Playá P, Gabilondo Zubizarreta FJ. Combined use of negative pressure wound therapy and Integra® to treat complex defects in lower extremities after burns. Ann Burns Fire Disasters. 2013;26(2):90-93.
33. Boyce A, Atherton DD, Tang R, Jawad M. The use of Matriderm in the management of an exposed Achilles tendon secondary to a burns injury. J Plast Reconstr Aesthet Surg. 2010;63(2):e206-207. doi:10.1016/j.bjps.2009.02.054
34. Vaseenon T, Somsuk W. Negative pressure wound therapy for traumatic foot and ankle wound: two case reports and review of the literature. J Med Assoc Thai. 2015;98(1):111-116.
35. Järvinen TAH, Kannus P, Maffulli N, Khan KM. Achilles tendon disorders: etiology and epidemiology. Foot Ankle Clin. 2005;10(2):255-266. doi:10.1016/j.fcl.2005.01.013
36. Saltzman CL, Tearse DS. Achilles tendon injuries. J Am Acad Orthop Surg. 1998;6(5):316-325. doi:10.5435/00124635-199809000-00007
37. Vaidya SR, Sharma SC, Al-Jabri T, Kayani B. Return to sport after surgical repair of the Achilles tendon. Br J Hosp Med (Lond). 2023;84(5):1-14. doi:10.12968/hmed.2022.0239
38. King CM, Vartivarian M. Achilles tendon rupture repair: simple to complex. Clin Podiatr Med Surg. 2023;40(1):75-96. doi:10.1016/j.cpm.2022.07.006
39. Marangi GF, Segreto F, Morelli Coppola M, Arcari L, Gratteri M, Persichetti P. Management of chronic seromas: a novel surgical approach with the use of vacuum assisted closure therapy. Int Wound J. 2020;17(5):1153-1158. doi:10.1111/iwj.13447
40. Segreto F, Marangi GF, Nobile C, et al. Use of platelet-rich plasma and modified nanofat grafting in infected ulcers: technical refinements to improve regenerative and antimicrobial potential. Arch Plast Surg. 2020;47(3):217-222. doi:10.5999/aps.2019.01571
41. Segreto F, Carotti S, Marangi GF, et al. The use of acellular porcine dermis, hyaluronic acid and polynucleotides in the treatment of cutaneous ulcers: single blind randomised clinical trial. Int Wound J. 2020;17(6):1702-1708. doi:10.1111/iwj.13454
42. Thompson G. An overview of negative pressure wound therapy (NPWT). Br J Community Nurs. 2008;13(6):S23-24, S26, S28-30. doi:10.12968/bjcn.2008.13.Sup3.29469
43. Huang C, Leavitt T, Bayer LR, Orgill DP. Effect of negative pressure wound therapy on wound healing. Curr Probl Surg. 2014;51(7):301-331. doi:10.1067/j.cpsurg.2014.04.001
44. Apelqvist J, Willy C, Fagerdahl AM, et al. EWMA document: negative pressure wound therapy. J Wound Care. 2017;26(Sup3):S1-S154. doi:10.12968/jowc.2017.26.Sup3.S1
45. De Pellegrin L, Feltri P, Filardo G, et al. Effects of negative pressure wound therapy with instillation and dwell time (NPWTi-d) versus NPWT or standard of care in orthoplastic surgery: a systematic review and meta-analysis. Int Wound J. 2023;20(6):2402-2413. doi:10.1111/iwj.14072
46. Yin Y, Zhang R, Li S, Guo J, Hou Z, Zhang Y. Negative-pressure therapy versus conventional therapy on split-thickness skin graft: a systematic review and meta-analysis. Int J Surg. 2018;50:43-48. doi:10.1016/j.ijsu.2017.12.020
47. Marangi GF, Faiola A, Cimmino AA, et al. Relevance of self-consciousness of appearance on patient satisfaction in primary rhinoplasty: a 12-month follow-up prospective study. Aesthetic Plast Surg. 2024;48(12):2269-2277. doi:10.1007/s00266-023-03803-3
48. Marangi GF, Gratteri M, Mirra C, et al. The correlation between the improvement in patient’s quality of life and surgeon’s satisfaction following primary breast augmentation: a prospective study. Aesthet Surg J. 2023;43(7):741-747. doi:10.1093/asj/sjad052
49. Gratteri M, Marangi GF, Mirra C, et al. Impact of incisional access site in primary breast augmentation: evaluation of patient satisfaction with SCAR-Q. Aesthetic Plast Surg. Published online July 26, 2023. doi:10.1007/s00266-023-03502-z
50. Marangi GF, Mirra C, Gratteri M, et al. Switching from galenic to advanced dressings or vacuum assisted closure therapy can improve quality of life of patients with chronic non-responsive pressure skin ulcers: preliminary data with Italian translation of WOUND-Q. Adv Wound Care (New Rochelle). 2024;13(3):131-139. doi:10.1089/wound.2022.0150
















