Topical Timolol Reduces the Number of Electrocauterization Treatments Required for Treatment of Pyogenic Granulation After Bromhidrosis Surgery
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Wounds or HMP Global, their employees, and affiliates.
Abstract
Background. Pyogenic granulation is a common complication of bromhidrosis surgery, and multiple electrocauterization sessions are usually required to treat this condition. Objective. To investigate the effectiveness of topical timolol for improving electrocauterization outcomes for pyogenic granulation. Methods. The medical data of 20 patients who underwent bilateral bromhidrosis surgery followed by electrocauterization treatments for pyogenic granulation between January 2021 and December 2022 were retrospectively reviewed. The first 10 patients did not use topical timolol (non-timolol group), and the second 10 patients applied topical timolol maleate 0.5% drops twice daily (timolol group) after each session of electrocauterization. The total number of electrocauterization sessions received by the patients were compared between the 2 groups. Results. The number of electrocauterization sessions was significantly less in the timolol group compared with the non-timolol group (median [range]: 3.5 [2-5] vs 5.5 [2-9]; P = .007). There was no statistically significant difference in age and sex distribution between the groups. Conclusion. Application of topical timolol twice daily is effective in decreasing the number of electrocauterization treatments required to treat pyogenic granulation after bromhidrosis surgery. Topical timolol can enhance wound healing and improve electrocauterization treatment outcomes.
Axillary bromhidrosis is a sweat gland condition characterized by unpleasant malodor due to excessive secretion of apocrine glands in the armpit interacting with local bacterial flora.1 The condition often negatively affects the patient’s physical and mental status, as well as their quality of life.1 Various treatments have been proposed to decrease gland secretion or bacterial growth, including surgical (both conventional and minimally invasive) and nonsurgical approaches. The effects of nonsurgical treatments are primarily temporary and limited; thus, surgical treatments are often used.2,3 However, although most bromhidrosis surgeries can achieve satisfactory results, complications inherent to this operation still occasionally occur.4
Formation of pyogenic granulation tissue is among the more serious complications associated with bromhidrosis surgery. When pyogenic granulation develops, the patient must undergo electrocauterization treatments, and the wound healing process may be prolonged. In addition, even after electrocauterization, pyogenic granulation tissue may still recur, requiring further electrocauterization sessions. Thus, it is necessary to find an effective treatment to improve the skin healing process and reduce the number of electrocauterization treatments required. The results of a recent study may provide the evidence to support the potential benefit of β-blockers in the treatment of pyogenic granulomas.5
β-Adrenergic receptors belong to the family of cell surface G protein coupled receptors. They are widely expressed in the human heart, lungs, glands, blood vessels, skin, and central nervous system, and they play critical roles in fundamental biological regulation.6-8 Three subtypes of β-adrenergic receptors have been identified: β1, β2, and β3. β2-Adrenoceptors are highly expressed in major cell types of the skin, including keratinocytes,9 melanocytes,10 fibroblasts,11 and the secretory coil of apocrine glands.12 Skin wound healing is a complex and well-organized biological process involving the release of cytokines and growth factors in the wound area; the migration and proliferation of keratinocytes, fibroblasts, endothelial cells, and immune cells; and extracellular matrix remodeling.13 The use of β-adrenergic receptor antagonists (β-blockers) to improve wound healing was first reported after their systemic administration in adult burn patients.14 The role of β2-
adrenoceptors in wound healing has also been investigated. A study showed that β2-adrenoceptors regulate the rate of epidermal barrier penetration by limiting epidermal water loss.15 Another study found that the activation of β2-adrenoceptors by 1 µM epinephrine/adrenaline delayed wound healing in human and mouse skin through a decrease in keratinocyte migration and wound epithelialization.16
Various topical drugs are currently used to manage and accelerate the healing rate of different types of skin wounds. Timolol is a β-blocker that is available for both topical and systemic administration. Topical timolol is approved by the United States Food and Drug Administration for the treatment of ocular hypertension and open-angle glaucoma; off-label uses include treatment of some vascular disorders, especially infantile hemangioma.17
The aim of the present study was to evaluate the effectiveness of topical timolol in reducing the number of electrocauterization sessions required and improving skin wound healing in patients undergoing minimally invasive bromhidrosis surgery.
Methods
Ethical considerations
This study was approved by the Institutional Review Board of Chang Gung Medical Foundation (IRB 202200098B0), and written informed consent was obtained from patients for all procedures performed. The equator network Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines were followed.
Patients
The medical data of 20 patients who underwent bilateral bromhidrosis surgery followed by electrocauterization treatments for pyogenic granulation between January 2021 and December 2022 were retrospectively reviewed. The minimally invasive bromhidrosis surgery was performed similar to the procedure described in other studies.4 Briefly, the axilla region was thoroughly sterilized, after which 150 mL of tumescent solution (500 mL 0.9% normal saline containing 20 mL sodium bicarbonate) mixed with lidocaine 0.4% and epinephrine 0.002% was injected subcutaneously. A mini-incision of approximately 0.3 cm to 0.4 cm was made at the center of the armpit. A skin flap was gently detached from the subcutaneous tissue with iris scissors, and the subcutaneous apocrine glands and hair follicles were then carefully excised. The wound was finally sutured with quilting sutures. Gauze ball compression was applied to the wound, and patients were asked to return to the clinic 3 days later for wound examination.
Patients with diabetes, autoimmune diseases, and a history of smoking were excluded. Patients with electrocauterization wounds that were diagonally larger than 1 cm were also excluded due to the complexity of factors involving wound healing. The first 10 patients treated between January 2021 and December 2021 received only Aquacel Ag Foam dressing (Convatec) to cover the wound after electrocauterization; this dressing was changed once daily (non-timolol group). The second 10 patients treated between January 2022 and December 2022 applied topical timolol drops (timolol maleate 0.5% solution; Timoptol-XE, Taiwan Santen pharmaceutical Co, Ltd) to the wound twice daily (morning and evening), and then applied the aforementioned foam dressing to cover the wound (timolol group). Patients were asked to send photographs of the wound to the clinic every 3 days and were followed for 40 days. During the follow-up period, patients returned to the clinic if additional electrocauterization treatment was required.
Statistical analysis
Continuous data were expressed as median and range, and categorical data were expressed as number and percentage. Comparisons of continuous data between the 2 groups was performed using the Mann-Whitney U test, and the Pearson chi-square test was used for comparisons of categorical data. All statistical analysis was performed with SPSS version 22.0 (IBM Corporation). An alpha value less than .05 was considered to indicate statistical significance.
Results
Comparison of the number of electrocauterization treatments between the timolol and non-timolol groups
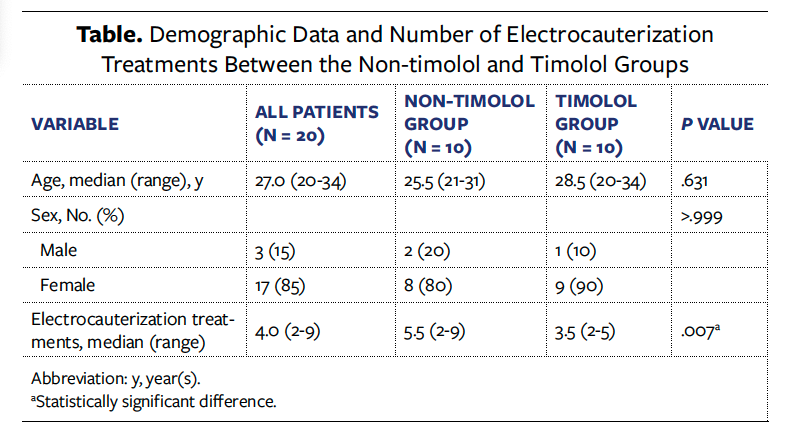
Twenty patients who underwent bilateral axillary bromhidrosis surgery and who afterward received electrocauterization treatments for pyogenic granulation were included, with 10 patients in the non-timolol group and 10 in the timolol group. Most patients were female (85%), and the remaining 15% were male; patient sex was self-reported. Patient demographic data and the number of electrocauterization treatments received by the patients are summarized in the Table. There was no statistically significant difference in the distribution of age and sex between the timolol and non-timolol groups (P = .631 and P > .999 for age and sex, respectively). The number of electrocauterization treatments was significantly less in the timolol group compared with the non-timolol group (median [range]: 3.5 [2-5] vs 5.5 [2-9]; P = .007).
Wound appearance before and after electrocauterization
Two examples of pyogenic granulation with different wound sizes before and after electrocauterization are shown in the Figure. Pyogenic granulation tissue that developed after axillary bromhidrosis is shown in the Figure, part A and part C. After electrocauterization treatment, the pyogenic granulation tissue shrunk and bleeding stopped (Figure, part B and part D).

Discussion
The present study demonstrated that topical timolol significantly reduced the number of electrocauterization treatments required for managing pyogenic granulation after bromhidrosis surgery, suggesting that topical timolol may effectively prevent the formation of pyogenic granulation and enhance skin wound healing. To the knowledge of the authors of the present study, very few studies have examined the use of topical timolol specifically for the treatment of pyogenic granulation after bromhidrosis surgery treated by electrocauterization. The results of the present study indicate the usefulness of topical timolol in this setting.
Pyogenic granuloma is a benign, acquired vascular proliferation of the skin and mucosa that can develop in response to trauma, skin irritation, hormonal effects, and viral pathogens.18,19 Despite its benign properties, pyogenic granulation is often a source of concern due to recurrent bleeding, even with minimal trauma, and it can have a notable negative effect on the patient’s quality of life. Current management for pyogenic granuloma is mainly ablative,5 including methods such as radiofrequency,20 laser,21 electrosurgery (cauterization),22 curettage,23 and cryotherapy.23 Although these methods have shown some effectiveness in the management of pyogenic granuloma, there is currently no standardized treatment.5 In addition, even with attentive care pyogenic granulation may recur frequently. Giblin et al24 reported a recurrence rate of 3.7% in 326 lesions treated by surgical excision. In the present study, there were recurrent episodes of pyogenic granulation that required multiple electrocauterization treatments.
Electrocauterization (or electrocautery) is a form of electrosurgery that involves passing a direct current through a metal wire that resists the flow of energy and thus generates heat; the thermal energy is used to cut or coagulate tissue.25 This method is quite useful for achieving hemostasis; however, the high-frequency electrical energy may impair wound healing. As a result, complications such as pyogenic granulation may occur. In the present study, the application of topical timolol after electrocauterization for the treatment of pyogenic granulation significantly reduced the number of electrocauterization treatments required. The results suggest that topical application of a β-blocker may improve the skin wound healing process after electrocauterization.
Topical timolol is widely used for the treatment of vascular dermatoses and injured skin, especially infantile hemangioma.26,27 It is thought that local vasoconstriction with a subsequent reduction in blood supply, as well as inhibition of pro-angiogenic factors, leads to lesion shrinkage and resolution over time. Topical timolol has also been used to treat pyogenic granulation. Ebrahimi et al28 used 0.5% timolol drops twice daily in combination with oral propranolol to treat postburn pyogenic granuloma in a 17-month-old boy and a 7-year-old girl and reported improvement in skin lesions with no adverse effects. A randomized study by Patra et al5 that included 40 patients reported that 0.5% timolol treatment significantly reduced the size of pyogenic granulation compared with placebo (percentage reduction in size: timolol, 40.9% vs placebo, 3.4%; P = .002); it also improved color and bleeding tendency. The results of that study also showed that fewer rescue treatments (electrosurgery) were required in the timolol group (n = 1) than in the placebo group (n = 5), although the difference was not statistically significant. The results of the present study showed that application of topical timolol maleate 0.5% drops significantly reduced the number of electrocauterization sessions required to treat pyogenic granulation compared with no use of timolol, with no noticeable complications. The results indicate that topical timolol is effective in preventing the formation of pyogenic granulation without generating considerable adverse effects.
Limitations
The present study has some limitations. First, the number of patients was small, which may limit the generalizability of the study conclusion. Second, the application of topical timolol drops was performed by the patients themselves, and the amount of timolol used could not be precisely controlled. Third, the follow-up time was short (40 days); recurrence of pyogenic granulation may be observed with longer follow-up. In addition, this study is limited due to its retrospective nature.
Conclusion
Although axillary bromhidrosis surgery is safe and satisfactory results can be achieved in most cases, complications such as pyogenic granulation may occur and impair patient quality of life. Electrocauterization is commonly used to treat pyogenic granulation that develops after bromhidrosis surgery, but typically, multiple sessions of electrocauterization are required. Application of topical timolol maleate 0.5% drops twice a day after each electrocauterization can significantly reduce the number of electrocauterization treatments required, suggesting that topical timolol is effective in improving electrocauterization outcomes
Author and Public Information
Authors: Wen-Tsao Ho, MD1; and Chin-Yi Yang, MD2,3,4
Affiliations: 1Department of Dermatology, Ho Wen Tsao Skin Clinic, New Taipei City, Taiwan; 2Department of Dermatology, New Taipei Municipal TuCheng Hospital, New Taipei City, Taiwan; 3Department of Dermatology, Linkou Chang Gung Memorial Hospital, Taoyuan City, Taiwan; 4Department of Cosmetic Science, Chang Gung University of Science and Technology, Taoyuan City, Taiwan
Disclosure: The authors have no financial or other conflicts of interest to disclose.
Ethical Approval: This study was approved by the Institutional Review Board of Chang Gung Medical Foundation (IRB 202200098B0), and written informed consent was obtained from patients for all procedures performed.
Correspondence: Chin-Yi Yang, MD; Department of Dermatology, New Taipei Municipal TuCheng Hospital, No. 6, Sec. 2, Jincheng Rd, Tucheng Dist., New Taipei City 236, Taiwan; sophiachinyi@gmail.com
Manuscript Accepted: March 11, 2025
References
1. Semkova K, Gergovska M, Kazandjieva J, Tsankov N. Hyperhidrosis, bromhidrosis, and chromhidrosis: fold (intertriginous) dermatoses. Clin Dermatol. 2015;33(4):483-491. doi:10.1016/j.clindermatol.2015.04.013
2. Lawrence CM, Lonsdale Eccles AA. Selective sweat gland removal with minimal skin excision in the treatment of axillary hyperhidrosis: a retrospective clinical and histological review of 15 patients. Br J Dermatol. 2006;155(1):115-118. doi:10.1111/j.1365-2133.2006.07320.x
3. Liu Q, Zhou Q, Song Y, Yang S, Zheng J, Ding Z. Surgical subcision as a cost-effective and minimally invasive treatment for axillary osmidrosis. J Cosmet Dermatol. 2010;9(1):44-49. doi:10.1111/j.1473-2165.2010.00477.x
4. Zhao H, Li S, Nabi O, Hu L, Gao X, Luo F. Treatment of axillary bromhidrosis through a mini-incision with subdermal vascular preservation: a retrospective study in 396 patients. Int J Dermatol. 2016;55(8):919-925. doi:10.1111/ijd.13313
5. Patra AC, Sil A, Ahmed SS, et al. Effectiveness and safety of 0.5% timolol solution in the treatment of pyogenic granuloma: a randomized, double-blind and placebo-controlled study. Indian J Dermatol Venereol Leprol. 2022;88(4):500-508. doi:10.25259/IJDVL_565_20
6. Goodarzi A, Mozafarpoor S, Dodangeh M, Seirafianpour F, Shahverdi MH. The role of topical timolol in wound healing and the treatment of vascular lesions: a narrative review. Dermatol Ther. 2021;34(2):e14847. doi:10.1111/dth.14847
7. Taylor MR. Pharmacogenetics of the human beta-adrenergic receptors. Pharmacogenomics J. 2007;7(1):29-37. doi:10.1038/sj.tpj.6500393
8. Wallukat G. The beta-adrenergic receptors. Herz. 2002;27(7):683-690. doi:10.1007/s00059-002-2434-z
9. Sivamani RK, Lam ST, Isseroff RR. Beta adrenergic receptors in keratinocytes. Dermatol Clin. 2007;25(4):643-653, x. doi:10.1016/j.det.2007.06.012
10. Gillbro JM, Marles LK, Hibberts NA, Schallreuter KU. Autocrine catecholamine biosynthesis and the beta-adrenoceptor signal promote pigmentation in human epidermal melanocytes. J Invest Dermatol. 2004;123(2):346-353. doi:10.1111/j.0022-202X.2004.23210.x
11. Pullar CE, Isseroff RR. Beta 2-adrenergic receptor activation delays dermal fibroblast-mediated contraction of collagen gels via a cAMP-dependent mechanism. Wound Repair Regen. 2005;13(4):405-411. doi:10.1111/j.1067-1927.2005.130408.x
12. Lindsay SL, Holmes S, Corbett AD, Harker M, Bovell DL. Innervation and receptor profiles of the human apocrine (epitrichial) sweat gland: routes for intervention in bromhidrosis. Br J Dermatol. 2008;159(3):653-660. doi:10.1111/j.1365-2133.2008.08740.x
13. Gushiken LFS, Beserra FP, Bastos JK, Jackson CJ, Pellizzon CH. Cutaneous wound healing: an update from physiopathology to current therapies. Life (Basel). 2021;11(7):665. doi:10.3390/life11070665
14. Arbabi S, Ahrns KS, Wahl WL, et al. Beta-blocker use is associated with improved outcomes in adult burn patients. J Trauma. 2004;56(2):265-271. doi:10.1097/01.TA.0000109859.91202.C8
15. Denda M, Fuziwara S, Inoue K. Beta2-adrenergic receptor antagonist accelerates skin barrier recovery and reduces epidermal hyperplasia induced by barrier disruption. J Invest Dermatol. 2003;121(1):142-148. doi:10.1046/j.1523-1747.2003.12310.x
16. Yang HY, Steenhuis P, Glucksman AM, Gurenko Z, La TD, Isseroff RR. Alpha and beta adrenergic receptors modulate keratinocyte migration. PLoS One. 2021;16(7):e0253139. doi:10.1371/journal.pone.0253139
17. Barnes J, Moshirfar M. Timolol. StatPearls [Internet]. 2022.
18. Plachouri KM, Georgiou S. Therapeutic approaches to pyogenic granuloma: an updated review. Int J Dermatol. 2019;58(6):642-648. doi:10.1111/ijd.14268
19. Supekar BB, Wankhade VH, Chopkar AD, Singh RP, Bhat D. Multiple erythematous nodules: an intriguing entity. Indian Dermatol Online J. 2021;12(1):142-146. doi:10.4103/idoj.IDOJ_348_20
20. Singh S, Passi S. A 4-year multicentric experience of intravenous cannula-based intralesional radiofrequency ablation as an effective and safe office procedure for common cutaneous nodules. Indian J Dermatol Venereol Leprol. 2021;87(3):433-435. doi:10.25259/IJDVL_565_19
21. Rai S, Kaur M, Bhatnagar P. Laser: a powerful tool for treatment of pyogenic granuloma. J Cutan Aesthet Surg. 2011;4(2):144-147. doi:10.4103/0974-2077.85044
22. Hainer BL. Electrosurgery for the skin. Am Fam Physician. 2002;66(7):1259-1266.
23. Ghodsi SZ, Raziei M, Taheri A, Karami M, Mansoori P, Farnaghi F. Comparison of cryotherapy and curettage for the treatment of pyogenic granuloma: a randomized trial. Br J Dermatol. 2006;154(4):671-675. doi:10.1111/j.1365-2133.2005.06923.x
24. Giblin AV, Clover AJ, Athanassopoulos A, Budny PG. Pyogenic granuloma - the quest for optimum treatment: audit of treatment of 408 cases. J Plast Reconstr Aesthet Surg. 2007;60(9):1030-1035. doi:10.1016/j.bjps.2006.10.018
25. Baigrie D, Qafiti FN, Buicko Lopez JL. Electrosurgery. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025-. https://www.ncbi.nlm.nih.gov/books/NBK482380/
26. Wang X, Feng W, Zhao X, Liu Z, Dong L. The efficacy and safety of topical beta-blockers in treating infantile hemangiomas: a meta-analysis including 11 randomized controlled trials. Dermatology. 2021;237(3):433-443. doi:10.1159/000510029
27. Chen QY, Chang L, Qiu YJ, et al. Comparison of the efficacy between topical timolol and pulsed dye laser in the treatment of ulcerated infantile haemangiomas: a randomized controlled study. J Eur Acad Dermatol Venereol. 2021;35(12):e303-e305. doi:10.1111/dth.15907
28. Ebrahimi Z, Mahdi Z, Khairi AA, et al. Oral propranolol and topical timolol in the treatment of post-burn pyogenic granuloma: two cases and a review of the literature. Clin Case Rep. 2022;10(11):e6538. doi:10.1002/ccr3.6538
















