Pediatric Wound Prevention and Care: A Framework for Safer, Smarter NICU Practices
At the 2025 Symposium on Advanced Wound Care, Katherine McKeown, MSN, FNP-C, RNC-NIC, delivered a comprehensive and compelling session addressing the unique vulnerabilities and care strategies required for neonatal and pediatric skin injuries. With both clinical experience and personal passion, McKeown presented a standardized, evidence-based guideline tailored to the fragile physiology of preterm infants, many of whom lack fully developed skin structures and immune defense mechanisms.
Neonatal Skin: Unique Risks and Physiology
"Neonates are not just tiny adults," McKeown emphasized, underscoring the structural and functional immaturity of premature infant skin. Infants born as early as 23 to 26 weeks’ gestation often have no stratum corneum, poorly developed hair follicles, and are missing vital intracellular lipids. This makes them highly susceptible to medical adhesive-related skin injuries (MARSI) and medical device-related pressure injuries (MDRPIs), the latter being the leading cause of pressure injuries in neonates.
McKeown referenced postmortem skin analyses that confirmed longstanding hypotheses: “They actually found out when keratin is formed,” she said, highlighting the lack of skin barrier function in neonates and the implications for fluid loss, infection risk, and injury from common NICU devices such as CPAP masks and feeding tubes.
Infection Identification and Risks
Infections in NICU patients are particularly dangerous and hard to detect. McKeown noted that methicillin-sensitive Staphylococcus aureus (MSSA) can be just as deadly as methicillin-resistant Staphylococcus aureus (MRSA) in this population. “The burden of neonatal infection is huge,” she said, pointing to the fact that up to 15% of very low birth weight infants develop early-onset sepsis. She also provided practical tips for early recognition: “Anytime you hear your nurse say the skin fell off, you want to think to yourself, ‘Okay, this might be an infection.’”
Skin colonization, especially in the nasal passages, was another recurring red flag. “If you have a tiny baby that has diaper dermatitis in the first few weeks of life—that’s an infection,” McKeown said, describing two cases that tragically resulted in death due to undiagnosed infections.
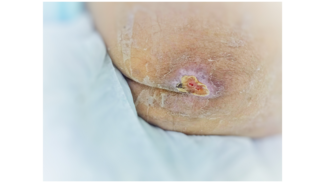
Dressing Selection and Wound Management
Dressings and topical products that are benign for adults can be devastating to neonates. Silicone contact layers, for example, must be changed every 3 to 4 days to prevent dermal ingrowth and subsequent trauma. “Even baby washes have some cytotoxic stuff,” McKeown warned. Instead, she advocated for amorphous hydrogel, hypochlorous acid (with caution), and medical-grade honey as safer alternatives, emphasizing their antimicrobial properties and tolerability.
In one case study, a nasal bridge injury healed completely with no visible scarring following the use of honey and hydrogel. McKeown noted, “He doesn’t even have a scar!”—a testament to proper wound care and gentle product selection.
Developmental Considerations and Pressure Injury Prevention
Bone ossification, or lack thereof, is another critical factor in pressure injury risk. “Babies won’t get coccyx or heel injuries until about age 8,” McKeown explained, but occipital pressure injuries are a concern in neonates due to their under-ossified skulls. This makes careful padding and device rotation essential.
She urged clinicians to tailor wound care strategies to the infant’s gestational age, emphasizing the need to ask, “How big, how old is my baby, and how long have they been in the NICU?”—a key determinant of skin maturity and risk.
Final Pearls for Practice
McKeown concluded with a call for vigilance, education, and innovation. “Moisture balance is everything; if the wound is too dry, you're going to stay de-wetted; if it's too wet, you'll macerate,” she said. She encouraged clinicians to advocate for noncytotoxic, breathable dressings and to approach every wound with individualized consideration.
Above all, McKeown’s talk was a reminder that neonatal skin care is a critical, life-saving discipline requiring creativity, compassion, and constant reevaluation of traditional practices. “I’m not worried that your son’s prematurity will kill him,” she recalled a practitioner once saying. “I’m worried that his skin will.”